Emergency Medical Teams in Disasters and Conflicts: Difference between revisions
No edit summary |
No edit summary |
||
| Line 28: | Line 28: | ||
|+'''Table.1''' Four Domains of Disaster Preparedness<ref name=":0">Lathia C, Skelton P, Clift Z. Early rehabilitation in conflicts and disasters. Handicap International: London, UK. 2020.</ref> | |+'''Table.1''' Four Domains of Disaster Preparedness<ref name=":0">Lathia C, Skelton P, Clift Z. Early rehabilitation in conflicts and disasters. Handicap International: London, UK. 2020.</ref> | ||
|- | |- | ||
! scope="col" | | ! scope="col" |Type | ||
! scope="col" | | ! scope="col" |Description | ||
! scope="col" | | ! scope="col" |Capacity | ||
! | !Minimum Length of Stay | ||
|- | |- | ||
| | |Type 1 Mobile | ||
|Mobile Outpatient Units | |||
Teams to access smallest communities in remote areas | |||
| >50 patients per day | |||
|2 Weeks | |||
|- | |||
| | |Type 1 Fixed | ||
|Outpatient facilities with or without tented structure | |||
|>100 patients pre day | |||
|2 Weeks | |||
|- | |||
|Type 2 | |||
|Inpatient Facilities with Surgery | |||
|> 100 outpatients | |||
20 inpatients | |||
| | |||
7 major operations or | |||
15 minor operations a day | |||
|3 Weeks | |||
|- | |||
|Type 3 | |||
|Referral Leave Care, | |||
Inpatient Facilities | |||
Surgery | |||
| | |||
High Dependency | |||
|> 100 outpatients | |||
40 inpatients, including; | |||
4–6 intensive care beds | |||
15 major operation per day | |||
30 minor operations per day | |||
|4 - 6 Weeks | |||
|- | |||
|Specialised Care Team | |||
|Teams that can join local facilities or EMTs to provide supplementary specialist care | |||
|Variable | |||
|Variable | |||
|} | |} | ||
Revision as of 02:15, 2 March 2022
Original Editors - Naomi O' Reilly
Top Contributors - Naomi O'Reilly, Kim Jackson, Rishika Babburu and Tarina van der Stockt
Introduction[edit | edit source]
Emergency Medical Teams (EMT), now considered a vital aspect of the global health workforce, are teams of health professionals (doctors, nurses, physiotherapists, occupational therapists, psychologists, paramedics, etc.) that provide direct clinical care to people affected by disasters and conflicts, and support local health systems. Any team of health professionals now coming from another country to practice health care in disaster or conflict setting need to arrive as part of a team, which must be qualified, trained, and bring equipment and supplies to deliver an effective response rather than imposing a burden on the national system. EMTs must strive for self-sufficiency, providing a quality of care that is appropriate for the context, with credentials that meet a minimum acceptable standard. Traditionally, these teams have been focused on the management of trauma and surgical care, but the response to the Ebola outbreak demonstrated the value in other contexts, such as epidemics and complex emergencies.[1]
EMT response can be both National and International from Governments (civil protection and military), Non-governmental Organisations (NGOs), International Humanitarian Networks (International Red Cross and Red Crescent Movement, Médecins sans Frontières), United Nations Contracted teams and Private-for-Profit Sector.
EMT Initiative[edit | edit source]
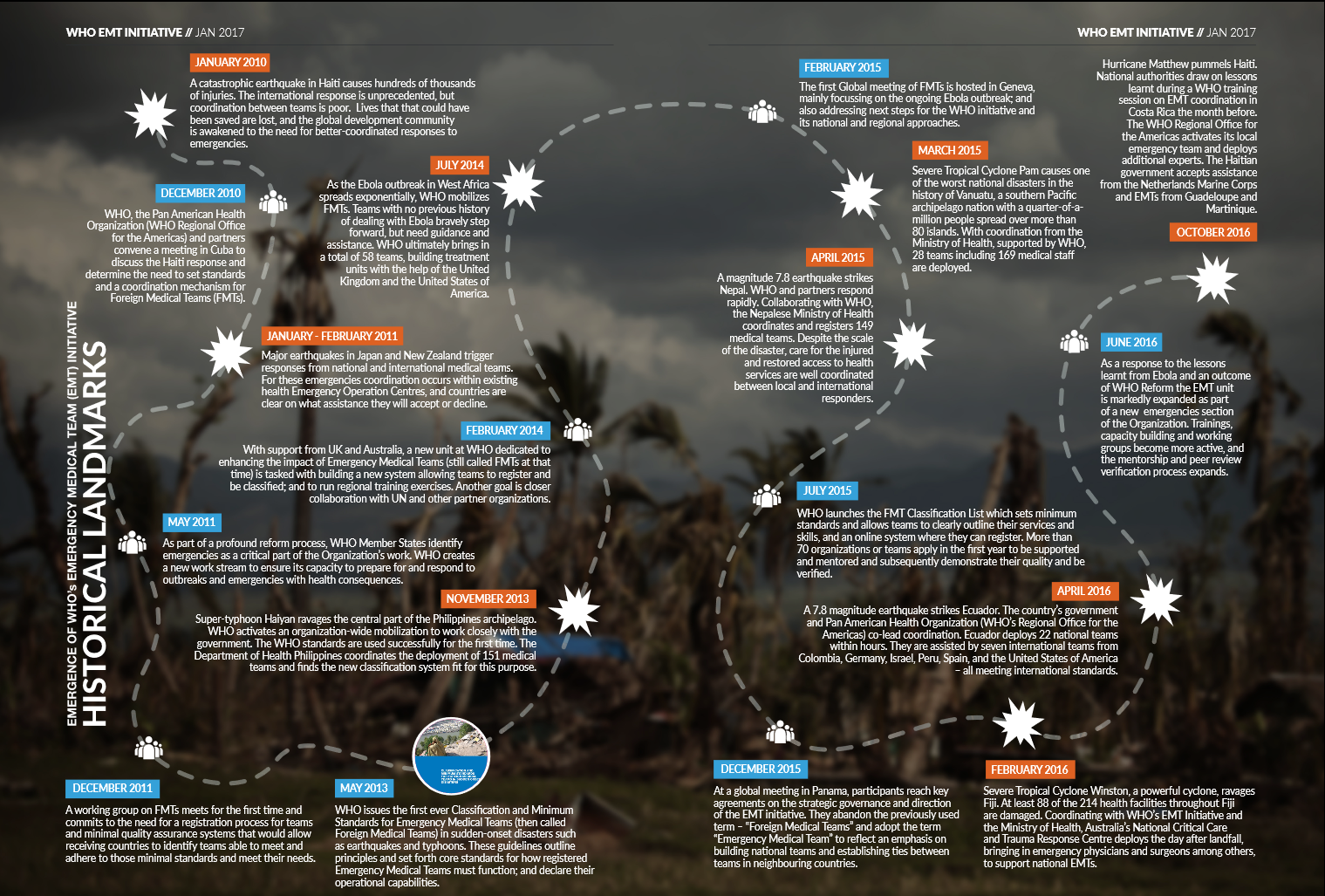
Significant lessons were learned about Foreign Medical Teams / Field Hospitals in the aftermath of Sudden-Onset Disasters following the catastrophic Haiti Earthquake in 2010 promoting collaboration of experts convened by the Pan American Health Organisation (PAHO) to initiate the development of principles, criteria and standards for foreign medical teams. This work formed the basis for the Classification and Minimum Standards for Foreign Medical Teams in Sudden Onset Disasters launched in May 2013 [2], that were first used successfully to mobilse and coordinate deployment of 151 medical teams by the Philippines Department of Health following Typhoon Haiyan in the Central Philippines Archipelago in November 2013. This further led to the development of the EMT Initiative, in alignment with the International Health Regulations (2005), which requires Member States to develop certain minimum public health capacities to “detect, assess, notify and report events” and to “respond promptly and effectively to public health risks and public health emergencies of international concern”.[3] This was further strengthen with the development of establishment of the Emergency Medical Teams Strategic Advisory Group (SAG) following EMT Global Meeting in Panama in December 2015.
Implemented through the World Health Organisation Global Secretariat and its three Regional Secretariats for Africa, Americas, South-East Asia, Europe, Eastern Mediterranean and Western Pacific, a key focus of the EMT Initiative is the development of national teams, that can be deployed in the shortest time possible, with utilisation of international teams key role to supplement and support local teams. The purpose of the EMT initiative is to improve the timeliness and quality of health services provided by national and international Emergency Medical Teams and enhance the capacity of national health systems in leading the activation and coordination of this response in the immediate aftermath of a disaster, outbreak and/or other emergency, with public health expertise and logistics support either included in the team or separately as specific public health or logistics rapid response teams. [4] The EMT Initiative also requires that all teams and their members are:
- licensed to practice in their home country;
- specialists in their field and have suitable malpractice insurance; and
- registered (and obtain licensing) with national authority and lead international agency.
EMT Classification[edit | edit source]
Launched in 2016 the EMT Global Classification Process, outlined in the World Health Organisation Classification and Minimum Standards for Emergency Medical Teams is an external peer review evaluation mechanism that assesses EMT compliance against internationally agreed guiding principles and core and technical standards, to improve quality of care and professionalism during EMT deployments. This benefits the populations served by ensuring EMTs arrive in a timely manner, are well trained and most importantly integrated within local health systems. With national health systems increasingly adopting the EMT Minimum Standards and Principles, Governments can be assured of a predictable and timely response by self-sufficient teams with well-trained health personnel.[3]
The process involves submission of an expression of interest by EMTs to join the World Health Organisation Global EMT List, followed by a mentor supported external peer-review process to support the team towards meeting the international minimum standards and achieve quality assurance. To date, 26 teams have been classified with over 70 teams now working towards classification.
| Type | Description | Capacity | Minimum Length of Stay |
|---|---|---|---|
| Type 1 Mobile | Mobile Outpatient Units
Teams to access smallest communities in remote areas |
>50 patients per day | 2 Weeks |
| Type 1 Fixed | Outpatient facilities with or without tented structure | >100 patients pre day | 2 Weeks |
| Type 2 | Inpatient Facilities with Surgery | > 100 outpatients
20 inpatients 7 major operations or 15 minor operations a day |
3 Weeks |
| Type 3 | Referral Leave Care,
Inpatient Facilities Surgery High Dependency |
> 100 outpatients
40 inpatients, including; 4–6 intensive care beds 15 major operation per day 30 minor operations per day |
4 - 6 Weeks |
| Specialised Care Team | Teams that can join local facilities or EMTs to provide supplementary specialist care | Variable | Variable |
EMT Minimal Technical Standards Rehabilitation[edit | edit source]
Add your content to this page here!
Resources[edit | edit source]
Classification and Minimum Standards for Foreign Medical Teams in Sudden Onset Disasters
Minimum Technical Standards and Recommendations for Rehabilitation: Emergency Medical Teams
References [edit | edit source]
- ↑ World Health Organization (WHO). Minimum Technical Standards and Recommendations for Rehabilitation–Emergency Medical Teams.
- ↑ World Health Organization. Classification and Minimum Standards for Foreign Medical Teams in Sudden Onset Disasters. 2013
- ↑ 3.0 3.1 3.2 World Health Organization. Classification and Minimum Standards for Emergency Medical Teams. 2021 Cite error: Invalid
<ref>tag; name ":0" defined multiple times with different content - ↑ World Health Organisation. Emergency Medical Teams Initiative. Available from: https://extranet.who.int/emt/ (accessed 28 February 2022).