Elbow Examination: Difference between revisions
Kai A. Sigel (talk | contribs) (Added videos on neurological examination) |
(added Sports Medicine and Athlete Assessment_removed pubmed feed) |
||
| Line 6: | Line 6: | ||
== Subjective == | == Subjective == | ||
==== '''Clinical Presentation''' | ==== '''Clinical Presentation''' ==== | ||
[[Image:Bone ElbowAnatomy.jpg|right|200px]] | [[Image:Bone ElbowAnatomy.jpg|right|200px]] | ||
| Line 40: | Line 40: | ||
*SF-36: SF-36 is a generic health form. It is appropriate to address broad areas of health. For individuals with elbow dysfunction, the SF-36 is not a good tool to evaluate change in the clinic for patients with elbow disorders because it is not responsive and specific to the symptoms that the patient is reporting with. This measure can also be very time consuming and difficult to use.<ref name="number 1" /> | *SF-36: SF-36 is a generic health form. It is appropriate to address broad areas of health. For individuals with elbow dysfunction, the SF-36 is not a good tool to evaluate change in the clinic for patients with elbow disorders because it is not responsive and specific to the symptoms that the patient is reporting with. This measure can also be very time consuming and difficult to use.<ref name="number 1" /> | ||
==== '''Special Questions''' | ==== '''Special Questions''' ==== | ||
• Red and Yellow Flags- Conditions that may require referral to appropriate health care provider. | • Red and Yellow Flags- Conditions that may require referral to appropriate health care provider. | ||
| Line 64: | Line 64: | ||
<br> | <br> | ||
==== '''Investigations''' | ==== '''Investigations''' ==== | ||
[[Image:Elbow x-ray.PNG|thumb|right|300px|Normal articulations of the elbow from lateral and antero-posterior views]] | [[Image:Elbow x-ray.PNG|thumb|right|300px|Normal articulations of the elbow from lateral and antero-posterior views]] | ||
| Line 81: | Line 81: | ||
*Triangle Sign | *Triangle Sign | ||
=== Functional Tests | === Functional Tests === | ||
The goal in performing functional test is to obtain and quantify an asterisk sign to assess and reassess after intervention is performed. | The goal in performing functional test is to obtain and quantify an asterisk sign to assess and reassess after intervention is performed. | ||
| Line 100: | Line 100: | ||
[[Image:Anterior elbow.jpg|Illustration adapted from [Colman WW & Strauch RJ].]] [[Image:Lateral elbow.jpg|Image:Lateral_elbow.jpg]] [[Image:Medial elbow.jpg|Image:Medial_elbow.jpg]]<br> | [[Image:Anterior elbow.jpg|Illustration adapted from [Colman WW & Strauch RJ].]] [[Image:Lateral elbow.jpg|Image:Lateral_elbow.jpg]] [[Image:Medial elbow.jpg|Image:Medial_elbow.jpg]]<br> | ||
Image 2: Anterior Elbow<ref name="number 5"/> Image 3'':'' Lateral Elbow<ref name="number 5" /> Image 4: Medial Epicondyle<ref name="number 5" /> | Image 2: Anterior Elbow<ref name="number 5" /> Image 3'':'' Lateral Elbow<ref name="number 5" /> Image 4: Medial Epicondyle<ref name="number 5" /> | ||
Bicep tendon Marked Circle represents lateral epicondyle Dot represents medial epicondyle<br> | Bicep tendon Marked Circle represents lateral epicondyle Dot represents medial epicondyle<br> | ||
=== Neurologic Assessment | === Neurologic Assessment === | ||
*Reflexes: C5-C7 | *Reflexes: C5-C7 | ||
*Myotomes: C5-T1 | *Myotomes: C5-T1 | ||
| Line 117: | Line 117: | ||
=== Movement Testing === | === Movement Testing === | ||
{| width="40%" cellspacing="1" cellpadding="1" border="0" align="right | {| class="FCK__ShowTableBorders" width="40%" cellspacing="1" cellpadding="1" border="0" align="right" | ||
|- | |- | ||
| align="right" | | | align="right" | | ||
| Line 435: | Line 435: | ||
</w:LatentStyles> | </w:LatentStyles> | ||
</xml><![endif]--><!--[if gte mso 10]> | </xml><![endif]--><!--[if gte mso 10]> | ||
--><br> | |||
=== Special Tests (broken up by possible diagnosis) | === Special Tests (broken up by possible diagnosis) === | ||
[http://www.physio-pedia.com/index.php5?title=Cubital_Tunnel_Syndrome Cubital Tunnel Syndrome]: | [http://www.physio-pedia.com/index.php5?title=Cubital_Tunnel_Syndrome Cubital Tunnel Syndrome]: | ||
| Line 478: | Line 461: | ||
*Median nerve bias: Upper Limb Neurodynamic Test 1 | *Median nerve bias: Upper Limb Neurodynamic Test 1 | ||
*Radial nerve bias: Upper Limb Neurodynamic Test 2b | *Radial nerve bias: Upper Limb Neurodynamic Test 2b | ||
*Ulnar nerve bias: Upper Limb Neurodynamic Test 3<br> | *Ulnar nerve bias: Upper Limb Neurodynamic Test 3<br><div class="researchbox"> | ||
<div class="researchbox"> | |||
</div> | </div> | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Assessment]] [[Category:Elbow]] [[Category:Musculoskeletal/Orthopaedics]] [[Category:Temple_Student_Project]] [[Category:Videos]] [[Category:Upper_Limb_Assessment]] | [[Category:Assessment]] | ||
[[Category:Elbow]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Temple_Student_Project]] | |||
[[Category:Videos]] | |||
[[Category:Upper_Limb_Assessment]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Athlete Assessment]] | |||
Revision as of 20:47, 28 August 2018
Original Editor - Jason Brandi and Krista Dayton as part of the Temple University EBP Project
Lead Editors - Your name will be added here if you are a lead editor on this page.
Subjective[edit | edit source]
Clinical Presentation[edit | edit source]
Pain and symptoms localized in or around elbow. May present with neurological symptoms local or distant to elbow.
Subjective History[edit | edit source]
• Exact location of pain
• Timeline-When are the patients reported symptoms at their worst?
• Mechanism of the injury- In the case of a traumatic event, the mechanism of injury helps guide the diagnosis.[1] For atraumatic injuries, specific symptoms can be highly useful in determining a diagnosis.
For example: patient reported numbness and/or tingling in the 5th digit may suggest ulnar neuropathy.[1]
• Presence of numbness or tingling?
• Medications?
• Past Medical History
• Diagnostic Testing/Imaging?
• Region Specific Historical Question: These questions will help guide the examination. For example[2]:
Please refer to the User's Guide to the Musculoskeletal Examination for further information.2
1. Do your symptoms change (better or worse) with any movements of the neck or shoulder?
2. Does your elbow ever “slip out” or feel unstable?
3. Does the pain change with gripping activities?
4. Do you ever experience numbness of tingling in the hand?
5. Was the elbow hyper extended during the time of injury?
6. Do you relate the symptoms to a throwing activity?
• Environmental and Personal Factors
During the initial examination, environmental and personal factors should be addressed. These issues could affect healing and return of function after an elbow injury. Table 1 outlines these issues.[1]
| Table 1. Patient Factors that can affect healing and return of function after elbow injury |
| Diabetes • Immunosuppression • Infection • Multiple site injuries • Tobacco use • Excessive alcohol intake • Complications following injury or surgery(joint stiffness, heterotopic ossification, infection, joint instability) |
Self-Report Outcome Measures[edit | edit source]
- DASH (Quick Dash)
- Patient-Specific Functional Scale
- PREE and ASES: Patient-rated elbow evaluation (PREE)[1] and American Shoulder and Elbow Society evaluation(ASES)[3] are two similar scales that allow the patient to self-report their pain and disability related to their elbow pathology. The conceptual difference between the two scales is minimal and the correlation between the two scales usually exceeds 0.90.[1]
- P4: P4 is a 4-item pain intensity measure. The P4 asks patients to rate pain in the morning, afternoon, evening, and with activity over the past 2 days. The P4 can be particularly useful as the elbow is greatly impacted by movement and time of day.[1]
- SF-36: SF-36 is a generic health form. It is appropriate to address broad areas of health. For individuals with elbow dysfunction, the SF-36 is not a good tool to evaluate change in the clinic for patients with elbow disorders because it is not responsive and specific to the symptoms that the patient is reporting with. This measure can also be very time consuming and difficult to use.[1]
Special Questions[edit | edit source]
• Red and Yellow Flags- Conditions that may require referral to appropriate health care provider.
| Red Flags |
| •Infection/Inflammation •Malignancy •Fracture/Dislocation (Positive Elbow Extension Test) • Inflammatory Arthritides •Abnormal Vitals •Abnormal Vascular/Neurological Exam •Heterotopic Ossification (Post-Surgical Consideration) •Inappropriate progress from treatment made after surgery |
| Yellow Flags |
|
-Psychosocial factors |
Investigations[edit | edit source]
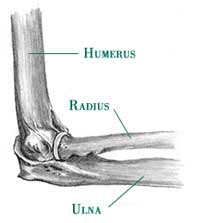
• Radiological Considerations
- The information from the history should be correlated with imaging findings of the elbow when available.[1]
Objective[edit | edit source]
Observation[edit | edit source]
- General posture of the upper quarter: Proximal factors should be considered which could predispose the patient to elbow symptoms.
- Thoracic and cervical spine including kyphosis and forward head
- Scapula
- Carrying angle: The carrying angle has a mean value of 10 degrees for men and 13 degrees for women.[4]
- Swelling/ecchymosis/deformities/muscle wasting
- Triangle Sign
Functional Tests[edit | edit source]
The goal in performing functional test is to obtain and quantify an asterisk sign to assess and reassess after intervention is performed.
- Determination of an asterisk sign-(What activity increases symptoms?)
- Pain-Free Grip Strength
- Push-off Test: The push off test can be used to quantify a person’s ability to bear weight through the upper extremity. This can help identify functional/occupational limitations. (ICC=0.31-0.97).[1]
- Functional Impairment Test-Hand, Neck, Shoulder Arm (FIT-HaNSA): Standardized physical test. Assesses gross activities of the upper extremity. Validation in elbow conditions has not yet been completed. [1]
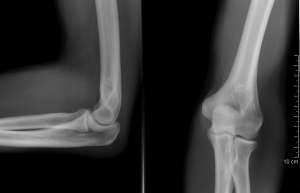
Palpation[edit | edit source]
- Medial/lateral epicondyle
- Olecranon and olecranon fossa
- Radial head
- Ulnar Collateral Ligament (UCL) of the elbow
- Soft tissue in upper arm and forearm/wrist for pain provocation, heat, swelling
Image 2: Anterior Elbow[4] Image 3: Lateral Elbow[4] Image 4: Medial Epicondyle[4]
Bicep tendon Marked Circle represents lateral epicondyle Dot represents medial epicondyle
Neurologic Assessment[edit | edit source]
- Reflexes: C5-C7
- Myotomes: C5-T1
| [5] | [6] |
- Dermatomes: C5-T1
Movement Testing[edit | edit source]
| [8] | [9] |
• Active Range Of Motion(AROM)/Passive Range Of Motion(PROM) with or without overpressure
o Elbow
Flexion
Extension
- Positive Elbow Extension Test may indicate fracture and referral.
Forearm pronation/supination
o Wrist
Flexion
Extension
o Cervical, Shoulder and Elbow Range of Motion with or without overpressure
Posterior-anterior glide assessment on cervical/thoracic spine for distal symptoms reproduction as well.
• Resistive testing
o Elbow flexion/extension
o Forearm pronation/supination
o Wrist flexion/extension
o Pain-free grip strength
o Thumb
o Fingers
• Accessory motion testing
o Humeroulnar traction
o Humeroradial traction
o Proximal/distal radioulnar Anterior/Posterior and Posterior/Anterior glides
Special Tests (broken up by possible diagnosis)[edit | edit source]
- Elbow Flexion Test
- Tinel's Sign
- Ulnar Nerve Compression Test
- Passive elbow extension, pronation, wrist flexion (Mill's Test)
- Resisted wrist extension with radial deviation (Cozen's Test)
- Resisted middle finger extension (Maudley's Test)
Ligamentous Tests:
- Median nerve bias: Upper Limb Neurodynamic Test 1
- Radial nerve bias: Upper Limb Neurodynamic Test 2b
- Ulnar nerve bias: Upper Limb Neurodynamic Test 3
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 MacDermid JC, Michlovitz SL. Examination of the elbow: linking diagnosis, prognosis, and outcomes as a framework for maximizing therapy interventions. J Hand Ther. 2006; 19(2):82-97.
- ↑ Flynn TW, Cleland JA, Whitman JM. User’s Guide to the Musculoskeletal Examination: Fundamentals for the Evidence Based Clinician. Evidence in Motion, 2008.
- ↑ King GJ, Richards RR, Zuckerman JD, et al. A standardized method for assessment of elbow function. Research Commitee, American Shoulder and Elbow Surgeons. J Shoulder Elbow Surg. 1999; 8:351–4.
- ↑ 4.0 4.1 4.2 4.3 Colman WW, Strauch RJ. Physical examination of the elbow. Orthop Clin North Am. 1999; 30(1):15-20.
- ↑ Physiotutors. Myotomes Upper Limb | Peripheral Neurological Examination. Available from: https://www.youtube.com/watch?v=kPuQPqBMGj0
- ↑ Physiotutors. Dermatomes Upper Limb | Peripheral Neurological Examination. Available from: https://www.youtube.com/watch?v=VlPpdRTGH-o
- ↑ Physiotutors. Upper Limb Deep Tendon Reflexes | Peripheral Neurological Examination. Available from: https://www.youtube.com/watch?v=FZsexSwddc0
- ↑ Physiotutors. Active Range of Motion: Elbow. Available from: https://www.youtube.com/watch?v=PNWRcx6ZYKg
- ↑ Physiotutors. Passive Range of Motion: Elbow. Available from: https://www.youtube.com/watch?v=qMISSAfZ4tc
- ↑ Physiotutors. Resisted Isometric Testing: Elbow. Available from: https://www.youtube.com/watch?v=BwUrosRGhzw
- ↑ Physiotutors. Joint Play: Elbow. Available from: https://www.youtube.com/watch?v=GxyxvcIEE-E
![Illustration adapted from [Colman WW & Strauch RJ].](/images/3/35/Anterior_elbow.jpg)