Effective Communication Techniques
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Elaine McDermott, Frank Ryan, Robyn Holton, Shawn Swartz, Kim Jackson, Lauren Lopez, Admin, 127.0.0.1, Zeeshan Hussain Mundh, Noel McLoughlin, Simisola Ajeyalemi, Jess Bell, Rucha Gadgil and Aimee Tow
Introduction[edit | edit source]
Resource Aims[edit | edit source]
Effective Communication Techniques in a healthcare setting has been developed on the bases that physiotherapists are in a unique position as part of a multidisciplinary team in that they can have substantially more contact time with patients than other members of the team. This means the physiotherapist is more appropriately positioned to develop a deeper patient-therapist relationship and in doing so educate and empower the patient of their physical condition and management.
Communication is an important tool in a healthcare setting that when used effectively can educate, empower and de-threaten common health issues patients present with in practice. However, if it is used ineffectively it can have detrimental effects creating fear, confusion and anxiety in patients as well as encouraging resistance to lifestyle changes and healthy behaviours.
It can be overwhelming for newly qualified or student physiotherapists as they must deal with such a broad range of conditions as well as differences in patient personalities, beliefs and motivation. This resource pack uses specific physical conditions as examples, however the communication strategies can be adapted and applied effectively across the broad range of physical conditions dealt with by physiotherapists.
This resource tool is in no way comprehensive and does not aim to cover every physical and mental condition dealt with by physiotherapists. For this reason, this tool is limited to communication around physical conditions and does not include information on communicating with mental issues or learning problems. It is a guide with suggested examples which can be adapted and applied to different situations with regards explaining and treating physical conditions. Included are further readings, reflection sections and relevant continuous professional development recommended to encourage the reader to actively engage with and consolidate their learning.
Audience[edit | edit source]
The Resource is aimed at student/ recently qualified physiotherapists. However, this should not be exclusive as other healthcare professionals, academics or individuals with an interest in the topic may extract relevant and useful information.
Learning Outcomes[edit | edit source]
Learning Outcomes:
- Understand the importance of effective communication and identify pathways which communication may be influenced.
- Identify the patients positive and negative emotional triggers and evaluate the impact on physical presentation
- Analyse the prevailing language/metaphors that exist within healthcare and assess their impact on the bio-psyco-social model of pain.
- Understand how assessment and explanation of disorders/pain needs to vary for different patients and select an appropriate communication technique with which to carry this out.
- Identify effective communication methods that may be helpful when explaining a diagnosis/treatment to a patient.
- Reflect upon one's own practice of communication techniques and identify areas requiring improvement
Importance of Good Communication[edit | edit source]
Introduction[edit | edit source]
Communication is an interactive process which involves the constructing and sharing of information, ideas and meaning through the use of a common system of symbols, signs and behaviours (CSP quality assurance standards). It includes the sharing of information, advice and ideas with a range of people, using;
- verbal
- non-verbal
- written and
- e-based
These can be modified to meet the patients preferences and needs.
Skilled and appropriate communication is the foundation of effective practice and is a key professional competence (See CSP core competency for communication and AHP standards of proficiency) which is highly valued by physiotherapy recipients (Parry, 2009). Effective communication requires consideration of the context, the nature of the information to be communicated and engagement with technology, particularly the effective and efficient use of Information and Communication Technology (CSP quality assurance standards [See fig 1.2).
Numerous studies have confirmed the importance of communication between physiotherapist and patient and interventions to enhance practice - some of which will be discussed throughout this learning resource.
Communication Pathways to improve health outcomes[edit | edit source]
To understand why communication may lead to better improved health outcomes researchers have identified pathways through which communication influences health and well being and can be simplified in figure 1.3 as proposed by Street (2009).
Direct Pathways[edit | edit source]
Talk may be therapeutic, meaning, a physiotherapist who validates the patients perspective or expresses empathy may help a patient experience improved psychological well being. Leading to the patient experiencing fewer negative emotions (e.g. fear and anxiety) and more positive ones (e.g., hope, optimism and self-worth) (Fogarty,1999; Ong, 2000; Schofield, 2003).
Non-verbal behaviours such as touch or tone of voice may directly enhance well-being by lessening anxiety or providing comfort (Henricson 2008, Knowlton 2006, Weve 2004 )
Indirect Pathways[edit | edit source]
In most cases, communication affects health through a more indirect or mediated route through proximal outcomes of the interaction, such as;
- satisfaction with care
- motivation to adhere
- trust in the clinician and system
- self efficacy in self care
- clinician – patient agreement and
- shared understanding
This could affect health or that could contribute to the intermediate outcomes (e.g., adherence, self-management skills, social support that lead to better health (see Figure 2) (stewart 1995). A physiotherapists clear explanation and expression of support could lead to greater patient trust and understanding of treatment options. This in turn may facilitate patient adherence to recommended therapy, which in turn improves the particular health outcome. Increased patient participation in the consultation could help the physiotherapist better understand the patient’s needs and preferences as well as discover possible misconceptions the patient may have about treatment options. The physiotherapist can then have the opportunity to communicate risk information in a way that the patient understands. This could lead to mutually agreed upon, higher quality decisions that best match the patients circumstances.
An article by Street et al (2009) explores these pathways to further broaden your knowledge. A link to this article can be found in ‘Further Reading’ section below.
Further Reading[edit | edit source]
Communication during Examination and Assessment[edit | edit source]
How Communication can impact the patient[edit | edit source]
The Macey Model of Doctor-patient Communication is a communication skills model that illustrates fundamental processes applicable to every meeting between physician and patient, and represents a complete set of core skills (see fig. 1.4). Although this tool was developed for doctors, the model provides an overall framework for systematically teaching vital communication elements.
The medical interview, particularly the subjective assessment, will determine the quantity, quality and accuracy of data that the physiotherapist will elicit. In turn, this will affect both the approach to the problem and the consequent care of the patient (Macey 2004). Ensuring that we communicate effectively will directly influence the patients behaviour and well being for
- Satisfaction with care
- Adherence to treatment plans
- Recall and understanding of the information given
- Coping with the diagnosis
- Quality of life and even state of health
(Ong et al 1995).
Table 1 briefly describes how communication may influence physical and psychological health of the patient.
Patient Learning Styles[edit | edit source]
Miscommunication between patients and physiotherapists is often documented when it comes to diagnosis explanation and treatment advice (Gill & Maynard, 2006, Donovan 1991) . Patients will describe symptoms in “lay” terms while physiotherapists often return feedback based on biomedical symptoms and processes of the condition using medical terms without taking into account the gap in the level of knowledge on the subject between the patient and themselves (Gill & Maynard, 2006, Donovan 1991). Research believes that this may be because physiotherapist’s often forget to take into account the difference in literacy levels between themselves and their patient, or they don’t know how to describe a condition outside of the medical model they have been taught during training. (Sullivan et al, 2001).
Studies show that literacy levels in some countries can be as low as age 10, (Weiss et al 1995). According to the Organisation for Economic Co-operation and Development, the UK is now ranked 22nd in a study of 24 EU countries in terms of literacy with a national literacy age of 10 years old.
In addition to this English is not everyone’s first language. According to the 2011 UK census 92% of residents acknowledged English as their first language and of the 8% remaining (3.3 million people), only 79% claimed they could speak English well or very well (National Office of Statistics 2011).
Both of these factors may cause difficulty and confusion when trying to speak to a patient about their diagnosis and to make an informed decision around treatment options
What is Learning[edit | edit source]
By getting a better understanding of patient’s learning styles and acknowledging the difference between lay and medical terminology, we can provide effective education which, in return, may increase the compliance and cooperation of patients. (Donavon, 1991).
Before educating the patient it is crucial that the following aspects are assessed:
- Patients needs
- Patients concerns
- Patients motivation and readiness to learn
- Patients preferences
- Patients support network
- Patients barriers and limitations to learning (mental health status, learning difficulties)
(Stromberg, 2005)
Patient behaviour is determined by several factors such as family and work commitments (Stromberg, 2005). Patients will often weigh up these factors and consider various options before settling on the choice most suitable to their personality and lifestyle (Stromberg, 2005).
Learning is defined as a process in which knowledge is created through the transformation of experience (Cassidy, 2004; Hauer et al, 2005). Individuals use learning to manage and adapt to everyday situations, giving rise to different types of learning styles (Cassidy, 2004; Hauer et al, 2005) .Through various research and studies, learning styles have been organised and categorized into levels, suggesting an individual’s capacity for flexible and adaptive model learning (Cassidy, 2004; Hauer et al, 2005). These levels are ranked in descending order of stability and are listed as:
- Personality traits
- Information processing
- Social interaction
- Instructional preference
(Cassidy, 2004; Hauer et al, 2005)
For instructional preference. Russel (2003) put together the below table which identifies three types of learning styles: Visual, Auditory & Kinesthetic .
The most common learning theory model in application is Kolb’s four stages of experiential model (1984), which, as the names suggest is based around four stages. The ideology is that individual’s transition from phase to phase in their learning process (Cassidy, 2004; Hauer et al, 2005). Very little research is available on the application of these teaching models to a healthcare setting perspective.
Figure 3: Kolb’s four stages of experiential model.
- Concrete experience: The patient learns of their diagnosis for the first time from the physio or they could have some previous knowledge or experience of the condition, possibly from news articles or friends or family members with experience or knowledge of the condition. This stage helps the patient to grasp what their diagnosis and prognosis is.
- Reflection on experience: The patient will go away and review and reflect on the experience and their understanding of their diagnosis.
- Abstract conceptualisation: The patient learns from the experience of their treatment and diagnosis.
- Experimental experience: The patient will plan and adapt to the arising situation and try out what has been learned in terms of education and treatment.
(Spencer, 2003)
Explaining Diagnosis[edit | edit source]
Breaking "Bad" News[edit | edit source]
Use of Metaphors in explaining diagnosis[edit | edit source]
“The medical profession has for a long time largely neglected the influence that language itself has in shaping and conceptualising medical practice” (cite)
Why is this? Over the past 3 decades there has been a growing body of evidence that has looked at the role of metaphors in healthcare(Loftus 2011). Historically metaphors were thought of being misleading and potentially counter productive for cognitive reconceptualising(Sontag 1978). Contemporary literature is much more welcoming of metaphors, especially within pain management. Now the research debate has shifted toward how metaphors should be applied in clinical practice rather than if metaphors are true or not. (Loftus 2011; & Stewart 2014)
We know that each and every patient that is seen comes with a very individual set of life experiences and different ways of shaping understanding of their “impairments" (Loftus 2011). Language and more specifically metaphors can aid in this process to promote advancement of a more meaningful understanding of diagnoses, avoidance of persistent pain, and self management strategies.(Loftus 2011) Despite these potential benefits, physiotherapists need to be aware of the chance of misinterpretations some patients might take from these metaphors.
In the busy environment of clinical practice(rephrase), physiotherapists can’t loose sight of the real people at the heart of the healthcare system(Stewart 2014). Due to the often complex idiosyncratic nature of bio-psycho-social pain, physiotherapists often use metaphors to try and create an “unique” reconceptualisation of what is really going on with the patients body.( Sullivan, 1995)
If we examine metaphors separate from the healthcare environment we know that metaphors can facilitate new ways of visualising the world and how we act within it. As a child we are always using our imagination or past experiences to create meaning of new experiences we face on a everyday basis. Physiotherapists must aid the patient to find meaning in the dialogue of personal, cultural, and physical experiences that have made up their lives(Gifford 1997).
Now if we integrate pain for example into this situation we can argue that pain is essentially an interpretation by that individual, it can be said that the only way to adequately understand pain is through metaphor itself(Stewart 2014). Ideally a set of metaphors that address the neurobiological contexts as well as the sociocultural contexts of their lives without looking at them dualistically but instead cohesively(Loftus 2011).
Commonly used Metaphors in practice[edit | edit source]
Over the years the use of metaphors have been looked at by many different research papers and some that are continually being used in practice produce poor patient outcomes. Below we will look at a few of the common metaphors being used across healthcare and analyse how they may benefit or be harmful to the patient.
The Body is a Machine[edit | edit source]
- This often implies that the patients are handing over their bodies to a health professional to locate the damage and administer treatment to repair the damage. Much like a car garage.
- Encourages us to think in a Dualistic way (BIOMEDICAL VS. BIO-PSYCHO-SOCIAL) , although if we recognise that social interaction, self interpretation and meaning are important; we must look for more adequate metaphors.
(Loftus 2011)
Medicine is War/ Military Metaphors[edit | edit source]
- Can imply that the patients are being passive and the doctors are warriors.
- Allows patients and clinicians to think that the patient has failed rather than the treatment.
- These metaphors can also lead some clinicians to think of themselves as a poor “soldier” and decrease confidence.
- Military metaphors can direct pain reconceptualisation away from bio-psycho-social evidence and think the war can be won with biomedical means of treatment.
(Loftus 2011;Louw 2011;Stewart 2014)
Brain as a Computer[edit | edit source]
This metaphor can sometimes help patients understand some of the complexities of neurobiology, but downplays the idiosyncratic and adaptive properties of the CNS.
(Stewart 2014)
Journey Metaphor[edit | edit source]
Some other metaphors paint a more adequate picture for patients and have been successful in practice, especially for patients with consistent pain.
Contrary to military metaphors, journey metaphors have destinations but in journeys there isn’t just one way to get to that destination. Patients and clinicians have the ability to adjust and try out different avenues . It has been proposed by Reisfield & Wilson (2004) that journey metaphors offer “different roads to travel, various avenues to explore and always there are exits to take.”
Journey metaphors rightfully shift the focus away from failure or success and focus on personalised adaptive exploration (Hartley 2012).
Advice and Cautions[edit | edit source]
As mentioned before there should be certain caution’s and encouraging tips to think about when delivering metaphors in clinical practice.
“When should we use and not use metaphors?”
Well that all depends on who is seeking medical help and how the metaphors are going to be used. There isn’t one metaphor that is good or bad, one metaphor might work great with one patient and be harmful or insignificant to another patient (Loftus 2011). This is when clinicians must open our toolkit and take out their clinical appraisal skills. Therapists must look at
“What patient has the condition, not what condition does the patient have?”
Physiotherapists must be aware of the potential of imposing our own bias on our patients, this is precisely why communication should be looked at in a dialogical manner.(Stewart 2014 & Loftus 2011)
“It takes two to tango”.
Through a dialogical approach to assessment we can better understand our patients and through that subjective information co-construct more meaningful metaphors (Loftus 2011). “Thacker & Mosley have argued that clinician dominant questioning can negate the critical need for the patients to have their psychological, social and philosophical stories heard.”( Yelling 2011)
Its important that we as clinicians understand and appreciate both the power and subtlety that language can possess (Loftus 2011). The debate shouldn’t be looking at what metaphor is the truest in all senses, this is irrelevant because metaphors aren’t true or false they are useful or not in various contexts.(Loftus 2011).
Communication when addressing persistent pain complaints[edit | edit source]
Introduction[edit | edit source]
What is Pain?[edit | edit source]
Every Chronic Pain was once Acute[edit | edit source]
Neuroscience Education[edit | edit source]
Explaining Pain: How to do it in under 10 minutes[edit | edit source]
Clinical Example: Osteoarthritis[edit | edit source]
When explaining a condition such as osteoarthritis to a patient we must consider what their viewpoint of the condition must be. Osteoarthritis is a condition of cartilage degeneration, subchondral bone stiffening and active new bone formation (Heuts et al, 2004).
Osteoarthritis is a complex sensory and emotional experience. An individual’s psychological characteristics and immediate psychological contest in which pain is experienced both influence their perception of pain (Hunter 2008).
Research has utilised qualitative methods and focus groups to establish the patient’s point of view. A common theme that is emerging is that patients are sometimes dissatisfied with the overall level of understanding, help and information that is given to them by healthcare professionals (Hill et al 2011). Patients also expressed concern that there was a lack of understanding by healthcare professionals as to the impact that osteoarthritis can have on an individual’s life (Hill et al 2011).
As physiotherapists, we must be aware of current and alternative treatments for OA (hydrotherapy, acupuncture etc) as contradictory information being given to the patient from different sources may lead to confusion as to what exactly they should be doing (Hill et al 2011).
Somers et al (2009) highlights that patients may adopt certain attitudes towards pain; Patients who are pain catastrophizing tend to focus on and magnify their pain sensations. This group of patients tend to feel helpless in the face of pain. Patients who adopt this stance report higher levels of pain, have higher levels of psychological and physical disability.
The second stance is patients who have pain related fear. They have a fear of physical activity as a result of feeling vulnerable to pain during activity. This group are more likely to engage in avoidance behaviours such as avoiding movement (Somers et al, 2009)
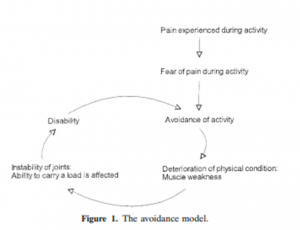
We as physiotherapists must remember that OA patients with a fear of engaging in painful movements may be hesitant to engage in physical activity. This can contribute to a vicious cycle of a more restricted and a physically inactive lifestyle which will lead to increased pain and disability (Somers et al 2009).
Hendry et al (2006) conducted qualitative research on primary care patients with OA. They found that personal experience, aetiology of arthritis and motivational factors all influenced compliance rates towards physical activity. Some patients believed that their joint problems were a direct result of heavy physical activity (Hill et al 2011). This is where we as clinicians must be aware that patients may present questions such as;
‘why should we exercise when our knees hurt?’
In the same study patients were asking
‘if it is wear and tear on the bone, is it helping to do all this exercise, walking and that?’
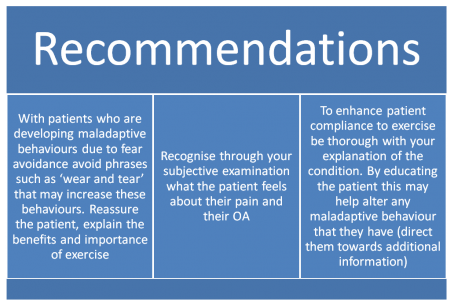
As physiotherapists we must be careful with our choice of words, phrases such as ‘wear and tear’ may be misinterpreted by some patients and lead to further maladaptive behaviour. Grive et al (2010) established that an ongoing concern of musculoskeletal professionals is that the use of this ‘wear and tear’ explanation often leads to decreased physical activity to avoid further ‘wearing of the joint’.
A unique approach adopted by a number of patients in the same study by Grive et al (2010) was the ‘use it or lose it’ approach. This simply put was use the joint or lose your functional ability. As physiotherapists we could utilise a similar approach to get our patients to comply with the physical exercise that we have prescribed as an intervention. Through effective communication we can increase a patient’s self efficacy and reduce their level of physical disability (Hunter 2008). Patients with higher self efficacy for pain control had higher thresholds for pain stimuli (hunter 2008). Can we as physiotherapists use this to our advantage to increase patient’s compliance to exercise?
Exercise has been shown to have a positive effect on functional ability in patients with OA (Heuts et al, 2004). We as physiotherapists must consider the role of pain related fear in patients with OA and investigate different treatment approaches to combat this behaviour (Heuts et al, 2004).
Scopaz et al (2009) suggests psychological factors such as anxiety, fear and depression may also be related to physical function in patients with OA of the knee.
Further to this, a model of fear avoidance suggests that patients can either be adaptive and non-adaptive in their approach to their pain and functional ability (Scopaz et al, 2009).
This model indicates that anxiety + fear avoidance beliefs are significant predictors of self report physical function in patients with knee OA (Scopaz et al, 2009).
Following on from this, we may also consider the avoidance model presented by Dekker et al (1993)
This model indicates that a decreased muscle strength as a result of activity avoidance leads to activity limitations (Holla et al, 2012).
Recommendations[edit | edit source]
'What can us as physiotherapists do to combat these beliefs that may be instilled in patients?'
Sensitive Issues: Obesity[edit | edit source]
Introduction[edit | edit source]
The issue with "Calling it as it is"[edit | edit source]
Motivational Interviewing[edit | edit source]
Introduction[edit | edit source]
Theoretical Bases[edit | edit source]
Principles of MI[edit | edit source]
MI Techniques[edit | edit source]
Summary[edit | edit source]
How to best Implement MI[edit | edit source]
Useful Questions[edit | edit source]
Step 1: Practice using a Guiding Style[edit | edit source]
Step 2: Develop Useful Strategies[edit | edit source]
Agenda Setting: Deciding What to Change[edit | edit source]
Pro's & Con's: Deciding Why the Change[edit | edit source]
Assess Importance and Confidence[edit | edit source]
Exchange Information[edit | edit source]
Setting Goals[edit | edit source]
Step 3: Skillfully respond to and change patients language[edit | edit source]
Challenges faced by PT's when using MI[edit | edit source]
Examples in Practice[edit | edit source]
References[edit | edit source]
References will automatically be added here, see adding references tutorial.