|
|
| (23 intermediate revisions by 8 users not shown) |
| Line 1: |
Line 1: |
| <div class="editorbox"> '''Original Editor '''- [[User:Elizabeth Cachia|Elizabeth Cachia]], [[User:Shelly Dineen|Shelly Dineen]], [[User:James Egan|James Egan]], [[User:Alex James|Alex James]], [[User:Joe Nelmes|Joe Nelmes]] and [[User:David Serafini|David Serafini]] as part of the [[Current_and_Emerging_Roles_in_Physiotherapy_Practice|Queen Margaret University Project]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | | <div class="editorbox"> '''Original Editor '''- [[User:Elizabeth Cachia|Elizabeth Cachia]], [[User:Shelly Dineen|Shelly Dineen]], [[User:James Egan|James Egan]], [[User:Alex James|Alex James]], [[User:Joe Nelmes|Joe Nelmes]] and [[User:David Serafini|David Serafini]] as part of the [[Current_and_Emerging_Roles_in_Physiotherapy_Practice|Queen Margaret University Project]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> |
|
| |
|
| <div class="noeditbox">
| | |
| This article is currently under review and may not be up to date. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}})
| |
| </div>
| |
|
| |
|
| == Introduction== | | == Introduction== |
| Down Syndrome (DS) is a chromosomal alteration<ref name=":32">National Down Syndrome Society. What is down syndrome. London: NDSS. https://www.ndss.org/about-down-syndrome/down-syndrome/ (accessed 09 March 2022).</ref>. Chromosomes are structures found in every cell of the body that contain genetic material and are responsible for determining anything ranging from your eye colour to your height<ref name=":33">National Human Genome Research Institute. Chromosome. Available from <nowiki>https://www.genome.gov/genetics-glossary/Chromosome</nowiki> (accessed 9 March 2022).</ref>. Typically, each cell has 23 pairs of chromosomes, with half coming from each parent <ref name=":33" />. Down syndrome, however, occurs when chromosome 21 has a full or partial extra copy in some, or all, of that individual’s cells<ref name=":32" />. This triple copy is sometimes called trisomy 21<ref name=":32" /> . The altered number of chromosomes leads to common physical features in the DS population, such as: | | Down Syndrome (DS) is a genetic, chromosomal condition.<ref name=":32">National Down Syndrome Society. What is down syndrome. London: NDSS. https://www.ndss.org/about-down-syndrome/down-syndrome/ (accessed 09 March 2022).</ref> Chromosomes are structures found in every cell of the body that contain genetic material and are responsible for determining anything ranging from eye colour to height.<ref name=":33">National Human Genome Research Institute. Chromosome. Available from <nowiki>https://www.genome.gov/genetics-glossary/Chromosome</nowiki> (accessed 9 March 2022).</ref> Typically, each cell has 23 pairs of chromosomes.<ref name=":33" /> However, in individuals with Down syndrome, there is a full or partial extra copy of chromosome 21 in some, or all, cells.<ref name=":32" /> |
| | |
| [[File:DS features.jpg|center|frameless|460x460px|<ref>Kami T. Signs of Down Syndrome. 2008. [Picture]. www.womens-health-advice.com/photos/down-syndrome.html (accessed18 March 2018).</ref>]]
| |
| | |
| The following video “Ted Talk” presented by Karen Gaffney, a person with Down Syndrome, explores numerous contemporary thoughts surrounding DS and challenges society's preconceptions of people with DS.
| |
| {{#ev: youtube| HwxjoBQdn0s}}
| |
|
| |
|
| === Epidemiology === | | === Epidemiology === |
| DS is the most commonly occurring chromosomal variance noted worldwide, with 1 in 1000 births resulting in a child with DS<ref name=":32" /> <ref name=":34" />. In the UK alone, there are approximately 40,000 people living with Down Syndrome, and 750 new born with DS each year <ref name=":34">Learning Disability Today. Spotlight on: Down Syndrome. Available from https://www.learningdisabilitytoday.co.uk/spotlight-on-downs-syndrome (accessed 09 March 2022).</ref>. Birth rates are expected to stay the same, but the total population of persons with DS is expected to rise in the coming years. This is mainly due to medical advancements which have increased life expectancy from age 9 in 1929, to 60 years of age today <ref>Zhu J, Hasle H, Correa A, Schendel D, Friedmant J, Olsen J, Ramussen S. Survival among people with down syndrome. Genetics in Medicine 2013;15:64-69. <nowiki>https://www.nature.com/articles/gim201293</nowiki> (accessed 12 March 2018). </ref>. With this increase in the number and age of this population, there will be a larger demand on health services, such as physiotherapy, and increased challenges for families to overcome. | | DS is the most commonly occurring chromosomal variance noted worldwide, with 1 in 1000 births resulting in a child with DS.<ref name=":32" /> <ref name=":34" /><ref>Windsperger K, Hoehl S. [https://www.frontiersin.org/articles/10.3389/fpsyt.2021.749046/full Development of Down Syndrome Research Over the Last Decades–What Healthcare and Education Professionals Need to Know]. Frontiers in Psychiatry. 2021 Dec 14;12:749046.</ref> In the UK alone, there are approximately 40,000 people living with Down Syndrome, and 750 are born each year with DS <ref name=":34">Learning Disability Today. Spotlight on: Down Syndrome. Available from https://www.learningdisabilitytoday.co.uk/spotlight-on-downs-syndrome (accessed 09 March 2022).</ref>. Birth rates are expected to stay the same, but the total population of persons with DS is expected to rise in the coming years. This is mainly due to medical advancements which have increased life expectancy from age 9 in 1929,<ref>Carr J, Collins S. [https://onlinelibrary.wiley.com/doi/10.1111/jar.12438 50 years with Down syndrome: A longitudinal study]. J Appl Res Intellect Disabil. 2018 Sep;31(5):743-750. </ref> to 60 years of age today.<ref>Zhu J, Hasle H, Correa A, Schendel D, Friedmant J, Olsen J, Ramussen S. Survival among people with down syndrome. Genetics in Medicine 2013;15:64-69. <nowiki>https://www.nature.com/articles/gim201293</nowiki> (accessed 12 March 2018). </ref> With this increase in the number and age of this population, there will be a larger demand on health services, such as physiotherapy, and increased challenges for families to overcome. |
| | |
| Additionally, persons with DS already report having problems gaining access to health care <ref>Allerton L, Emerson E. British adults with chronic health conditions or impairments face significant barriers to accessing health services. Public Health 2012;126:920-927. https://www.ncbi.nlm.nih.gov/pubmed/22959282 (accessed 13 March 2018).</ref> with the main barrier being a lack of knowledge about available services <ref>National Health Service. Promoting access to healthcare for people with a learning disability. www.jpaget.nhs.uk/media/186386/promoting_access_to_healtcare_for_people_with_learning_disabilities_a_guide_for_frontline_staff.pdf (accessed 14 March 2018).</ref>. Furthermore, parents of persons with DS also commonly express feeling stressed and uncertain about surrounding care of their child and state that they desire more help from physical activity specialists regarding both education and available interventions <ref>Menear, K. Parents perceptions of health and physical activity needs of children with Down syndrome. Down Syndrome Research 2007;12:60-68. <nowiki>https://library.down-syndrome.org/en-gb/research-practice/12/1/parents-perceptions-health-physical-activity-needs-down-syndrome/</nowiki> (accessed 12 April 2018).</ref>.
| |
| == Signs and Symptoms == | | == Signs and Symptoms == |
| Though there are many similarities across the DS population, there is great variation in the syndrome. There are three types of DS, each with its own set of challenges and individual variation. The three types of DS are Trisomy 21 (95%), Translocation (3%-4%) and Mosaicism (1%)<ref>Pueschel SM, editor. A parent's guide to Down syndrome: Toward a brighter future. Brookes Pub; 2001.</ref>. Further information on the differences between categories can be found <u>'''[http://dsaco.net/three-types/ here]'''</u><ref>Down Syndrome Limerick. Different types of down syndrome. https://www.downsyndromelimerick.ie/services/new-parents/types-of-down-syndrome (accessed 17 March 2018).</ref>. Whichever the type, persons with DS typically have poorer overall health at a young age and exhibit a greater loss of health, mobility, and increased secondary complications as they age when compared to their non-DS counterparts <ref>British Institute of Learning Disabilities. Supporting older people with learning disabilities. <nowiki>https://www.ndti.org.uk/uploads/files/9354_Supporting_Older_People_ST3.pdf</nowiki> (accessed 18 March 2018).</ref><ref>Cruzado D, Vargas, A. Improving adherence physical activity with a smartphone application based on adults with intellectual disabilities. BMC Public Health. 2013;13:1173. <nowiki>https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-1173</nowiki> (accessed 11 March 2018).</ref>. As a result, persons with DS and their families frequently access a range of health services, including physiotherapy. Although DS itself is not a medical condition but is simply a common variation in the human form, there are many medical conditions that people with DS frequently experience. These include: | | Though there are many similarities across the DS population, there is great variation in the syndrome. There are three types of DS: Trisomy 21 (95%), Translocation (3%-4%) and Mosaicism (1%).<ref>Pueschel SM, editor. A parent's guide to Down syndrome: Toward a brighter future. Brookes Pub; 2001.</ref> Whichever the type, persons with DS typically have poorer overall health at a young age and exhibit a greater loss of health, mobility, and increased secondary complications as they age compared to their non-DS counterparts.<ref>British Institute of Learning Disabilities. Supporting older people with learning disabilities. <nowiki>https://www.ndti.org.uk/uploads/files/9354_Supporting_Older_People_ST3.pdf</nowiki> (accessed 18 March 2018).</ref><ref>Cruzado D, Vargas, A. Improving adherence physical activity with a smartphone application based on adults with intellectual disabilities. BMC Public Health. 2013;13:1173. <nowiki>https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-1173</nowiki> (accessed 11 March 2018).</ref> As a result, persons with DS and their families frequently access a range of health services, including physiotherapy. |
| [[File:Medical conditions.png|right|frameless|292x292px]]
| |
| * Learning difficulties
| |
| * Poor cardiac health
| |
| * Thyroid dysfunction
| |
| * Diabetes
| |
| * Obesity
| |
| * Digestive problems
| |
| * Low bone density
| |
| * Hearing and Vision loss
| |
| * Dementia and Alzheimer’s disease
| |
| * Depression
| |
| * Leukaemia <ref>Mazeurek D, Wyka J. Down syndrome: genetic and nutritional aspects of accompanying disorders. Roczniki Panstwowego Zakladu Higieny 2015;66:189-194. https://www.ncbi.nlm.nih.gov/pubmed/26400113 (accessed 17 March 2018). </ref><ref name=":1">National Human Genome Research Institute. Learning about Down syndrome. https://www.genome.gov/19517824/learning-about-down-syndrome/ (accessed 16 March 2018). </ref><ref name=":2">Sacks B, Buckley S. What do we know about the movement abilities of children with down syndrome. Down Syndrome News and Updates 2003;2:131-141. https://library.down-syndrome.org/en-gb/news-update/02/4/movement-abilities-down-syndrome/ (accessed18 March 2018).</ref>
| |
| | |
| == Developmental Milestones ==
| |
| | |
| From the time a child is born, they are growing and learning. Each person develops at a different pace. However, some skills are expected to be mastered by a specific age. These are called [[Child Development|developmental milestones]]. Milestones can be physical achievements, language-related, or social accomplishments. As physiotherapists, we typically focus on motor skills <ref name=":2" />.
| |
|
| |
|
| The ability to move is essential to human life and development. All children begin developing a wide range of movement skills, or motor skills, starting at birth. These motor skills are wide-ranging and often broken down into the sub-sections below:[[File:DS Motor Skills.png|center|frameless|623x623px]]
| | === Physical Characteristics === |
|
| |
|
| Motor skills are key for physical function, but also impact cognitive development.
| | * Growth failure |
| * Reaching and grasping allows a child to explore the characteristics of objects in his or her physical world. | | * Hypotonia |
| * Sitting promotes the use of arms and hands for playing. | | * Ligamentous laxity |
| * Walking allows a child to explore the world more effectively than crawling. | | * Flat posterior aspect of the head |
| * Independent movement increases opportunities for social interaction which promotes language learning <ref name=":0">National Down Syndrome Society. Down syndrome fact sheet. www.ndss.org/wp-content/uploads/2017/08/NDSS-Fact-Sheet-Language-Guide-2015.pdf (accessed 14 March 2018).</ref><ref name=":3">Layton T. Developmental Scale for Children with Down Syndrome. North Carolina: Extraordinary Learning Foundation. www.dsacc.org/downloads/parents/downsyndromedevelopmentalscale.pdf (accessed 20 March 2018). </ref>. | | * Broad flat face |
| | * Slanting eyes |
| | * Epicanthic eyefold |
| | * Short nose |
| | * Small and arched palate |
| | * Big wrinkled tongue |
| | * Dental anomalies |
| | * Short and broad hands |
| | * Special skin ridge patterns |
| | * Unilateral/bilateral absence of one rib |
| | * Congenital heart disease |
| | * Intestinal blockage |
| | * Enlarged colon |
| | * Umbilical hernia |
| | * Pelvis anomalies |
| | * Diminished muscle tone |
| | * Big toes widely spread |
|
| |
|
| === Developmental Milestones in Children with Down Syndrome === | | === Medical conditions === |
| Persons with DS will generally achieve all the same basic motor skills necessary for everyday living and personal independence, however, it may be at a later age and with less refinement compared to those without DS <ref>Kim H, Kim S, Kim J, Jeon H, Jung D. Motor and cognitive developmental profiles in children with down syndrome. Annals of Rehabilitation Medicine 2017;41:97-103. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5344833/ (accessed 21 March 2018). </ref>. Some adjusted milestones for DS are available below:[[File:Milestones DS.jpg|center|frameless|692x692px|<ref>National Down Syndrome Society. Down Syndrome Developmental Milestones. 2009. [Picture]. https://www.ndss.org/resources/early-intervention/ (accessed 12 March 2018).</ref>]]
| | DS is not a medical condition, but a common variation in the human form. There are, however, many medical conditions that people with DS frequently experience. These include: |
| | [[File:Medical conditions.png|thumb|224x224px]] |
|
| |
|
| For more in-depth developmental milestone charts, please see [http://www.healthforallchildren.com/wp-content/uploads/2013/04/A5-Downs-Instrucs-chartsfull-copy.pdf '''here''']<ref>Down Syndrome Medical Interest Group. PCHR insert for babies born with Down syndrome. Nottingham: Down Syndrome Medical Interest Group. www.healthforallchildren.com/wp-content/uploads/2013/04/A5-Downs-Instrucs-chartsfull-copy.pdf (accessed 21 March 2018). </ref>, a more in-depth description of milestones and a form for recording and tracking progress can be found [http://www.dsacc.org/downloads/parents/downsyndromedevelopmentalscale.pdf '''here''']<ref name=":3" />. While these milestones are generally agreed upon, studies targeting developmental milestones tend to only examine a small number of people. This makes the information less representative of the entire DS population. Researchers also commonly compare people with DS to their non-DS counterparts of the same age. This is an invalid comparison, and it would be more correct to compare children with DS to non-DS individuals of the same mental age. Despite these limitations, the above-listed milestones are widely used and considered accurate <ref>Frank K, Esbensen A. Fine motor and selfcare milestones for individuals with down syndrome using a retrospective chart review. Journal of Theoretical Social Psychology. 2015;89:719-729. https://onlinelibrary.wiley.com/doi/abs/10.1111/jir.12176 (accessed 20 March 2018). </ref>.
| | * learning difficulties |
| | * poor cardiac health |
| | * [[Thyroid Gland|thyroid]] dysfunction |
| | * [[diabetes]] |
| | * [[obesity]] |
| | * digestive problems |
| | * low bone density |
| | * hearing and vision loss |
| | * [[dementia]] and [[Alzheimer's Disease|Alzheimer's]] Disease |
| | * [[depression]] |
| | * [[Leukemia|leukaemia]] <sup></sup> |
|
| |
|
| == Balance and Down Syndrome ==
| | * |
| It is common for children with DS to be delayed in reaching common milestones such as sitting independently, standing and walking. One of the contributing factors to the delay of these specific milestones is poor balance. It is well known that persons with DS are often considered floppy, clumsy, uncoordinated and have awkward movement patterns due to balance issues. These balance challenges often follow the child into the teen years and sometimes into adulthood <ref>Georgescu M, Cernea M, Balan V. Postural control in down syndrome subjects. The European Proceedings of Social and Behavioural Sciences. www.futureacademy.org.uk/files/images/upload/ICPESK%202015%2035_333.pdf (accessed 17 March 2018).</ref>. While impaired balance is difficult on its own, it may also impact the development of other motor abilities and cognitive development. Being able to maintain balance allows for exploration, social interaction and overall freedom <ref name=":4">Malak R, Kostiukow A, Wasielewska A, Mojs E, Samborski W. Delays in motor development in children with down syndrome. Medical Science Monitor 2015;21:1904-1910. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4500597/ (accessed18 March 2018).</ref>.
| |
| === Factors Contributing to Poor Balance ===
| |
| * Ligament Laxity: Persons with DS have elastic/loose joints, allowing for a large range of movement. Although this doesn't sound like a problem it can lead to joints being less stable, difficult to control and may affect balance. | |
| * Low Muscle Tone: A common symptom of DS is a ‘floppy’ appearance of limbs, with little activity in the muscles at rest, impacting stationary balance. 'Floppiness' does improve over time but can influence balance greatly in the early years.
| |
| * Slow Reaction Times/Speed of Movement: Persons with DS often are slower to react and move than their non-DS peers. This means that even if the person feels unsteady, it will take a longer time to react to this feeling, and once it is understood, the corrective movement will also be delayed. Both of these aspects make balance challenging.
| |
| * Differences in Brain Size: Persons with DS typically have smaller cerebellums, which is a part of the brain that contributes to the control of balance. The small size impacts its function, limiting balance reflexes, and causing blurry vision when completing tasks at high speed. Other parts of the brain are also smaller, creating issues with voluntary activities, walking technique and coordination.
| |
| * Poor Postural Control: Typically the posture of a person with DS is slouched - hunched over, with a rounded neck. This prevents the head and body from sitting over the pelvis. Posture is impacted by inaccurate messages being sent to the brain from the body’s sensory system. This leaves people with DS less capable of adapting or making anticipatory adjustments to changing environments <ref name=":4" /><ref>Costa A. An assessment of optokinetic nystagmus in persons with down syndrome. Experimental Brain Research 2011;8:110-121. https://www.sciencedaily.com/releases/2011/08/110824142850.htm (accessed17 March 2018).</ref><ref>Saied B, Hassan D, Reza B. Postural stability in children with down syndrome. Medicina Sportiva 2014;1:2299-2304. https://search.proquest.com/docview/1510494760/fulltextPDF/6606B032D8C04A9EPQ/1?accountid=12269 (accessed19 March 2018).</ref>.
| |
|
| |
|
| == Strength and Down Syndrome == | | == Developmental Milestones and Down Syndrome == |
| Another contributing factor to delayed milestones and common challenge with DS is decreased strength.
| | Children with [[Down Syndrome (Trisomy 21)|Down Syndrome]] (DS) will generally achieve the same basic motor skills necessary for everyday living and personal independence. However, it may be at a later age and with less refinement compared to those without DS.<ref>Kim H, Kim S, Kim J, Jeon H, Jung D. Motor and cognitive developmental profiles in children with down syndrome. Annals of Rehabilitation Medicine 2017;41:97-103. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5344833/ (accessed 21 March 2018).</ref> Some adjusted milestones for DS are listed in the table below:[[File:Milestones DS.jpg|center|frameless|692x692px|link=https://www.physio-pedia.com/File:Milestones_DS.jpg]]It is common for children with DS to be delayed in reaching common milestones such as sitting independently, standing and walking. '''One of the contributing factors to the delay of these specific milestones is poor balance'''. Balance challenges often follow a child into their teen years and sometimes into adulthood.<ref>Georgescu M, Cernea M, Balan V. Postural control in down syndrome subjects. The European Proceedings of Social and Behavioural Sciences. www.futureacademy.org.uk/files/images/upload/ICPESK%202015%2035_333.pdf (accessed 17 March 2018).</ref> Impaired balance may also impact the development of other motor abilities and cognitive development. Being able to maintain balance allows for exploration, social interaction and overall freedom.<ref name=":4">Malak R, Kostiukow A, Wasielewska A, Mojs E, Samborski W. Delays in motor development in children with down syndrome. Medical Science Monitor 2015;21:1904-1910. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4500597/ (accessed18 March 2018).</ref> |
|
| |
|
| During childhood, children with DS do not experience the same amount of muscle growth or strength increase as their peers without DS <ref>Cowley P, Ploutz-Snyder L, Baynard T, Heffernan K, Jae S, Hsu S. Physical fitness predicts functional tasks in individuals with Down syndrome. Med Sci Sports Exercise 2010;42:388-393.</ref>. This is in part due to the decreased amount of physical activity experienced by people with DS but is also caused by unknown genetic reasons that research is still investigating. Regardless of the reason, persons with DS consistently fall behind in strength categories when compared to their peers without DS, individuals with DS typically exhibiting 40-50% less strength <ref>Mercer V, Stemmons V, Cynthia L. Hip abductor and knee extensor muscle strength of children with and without Down’s syndrome. Phys Ther 2001;1318-26.</ref>.
| | Some causes of balance difficulties are: |
| | * ligament laxity |
| | * low muscle tone |
| | * slow reaction times/speed of movement |
| | * differences in brain size: a smaller cerebellum impacts function, limits balance reflexes, and causes blurry vision when completing tasks at high speed. Other parts of the brain can also smaller, creating issues with voluntary activities, walking technique and coordination. |
| | * poor postural control<ref name=":4" /><ref>Costa A. An assessment of optokinetic nystagmus in persons with down syndrome. Experimental Brain Research 2011;8:110-121. https://www.sciencedaily.com/releases/2011/08/110824142850.htm (accessed17 March 2018).</ref><ref>Saied B, Hassan D, Reza B. Postural stability in children with down syndrome. Medicina Sportiva 2014;1:2299-2304. https://search.proquest.com/docview/1510494760/fulltextPDF/6606B032D8C04A9EPQ/1?accountid=12269 (accessed19 March 2018).</ref> |
| | '''Another contributing factor to delayed milestones and a common challenge for individuals with DS is decreased strength'''. |
|
| |
|
| === Factors Affecting Strength ===
| | During childhood, children with DS do not experience the same amount of muscle growth or strength increase as their peers without DS.<ref>Cowley P, Ploutz-Snyder L, Baynard T, Heffernan K, Jae S, Hsu S. Physical fitness predicts functional tasks in individuals with Down syndrome. Med Sci Sports Exercise 2010;42:388-393.</ref> Individuals with DS typically have 40-50% less strength.<ref>Mercer V, Stemmons V, Cynthia L. Hip abductor and knee extensor muscle strength of children with and without Down’s syndrome. Phys Ther 2001;1318-26.</ref> Decreased strength can impact activities of daily living, such as walking upstairs, getting out of a seat etc, but it can also lead to: |
| Decreased strength can have a large impact on the lives of persons with DS. Not only can it lead to complication of activities of daily living, making walking up the stairs, getting out of a seat and other seemingly simple tasks, major obstacles, but it can also lead to other problems. Some of these are listed below:
| | * increased wear and tear on joints |
| [[File:DS Flexing3.jpg|right|frameless|236x236px|<ref>Down Syndrome Society. Boy with Down syndrome Flexing. 2017. [Picture].</ref>]]
| | * higher risk of falls |
| * Increased wear and tear on joints
| | * elevated level of fatigue |
| * Contributes to reduced balance due to weakness of the stability muscles
| | * delayed developmental milestones |
| * Higher risk of falls
| | * increased risk of osteoporosis<ref name=":0">Merrick J, Ezra E, Josef B, Endel D, Steinberg D, Wientroub S. Musculoskeletal problems in Down syndrome. Israeli J Pediatr Orthop 2000;9:185-192.</ref> |
| * Elevated level of fatigue
| | It can also contribute to reduced balance due to weakness of the stability muscles.<ref name=":0" /> |
| * Delayed developmental milestones
| |
| * Increased risk of osteoporosis <ref>Merrick J, Ezra E, Josef B, Endel D, Steinberg D, Wientroub S. Musculoskeletal problems in Down syndrome. Israeli J Pediatr Orthop 2000;9:185-192.</ref>
| |
| == Reduced Levels of Physical Activity ==
| |
| The research on physical activity levels in people with Down syndrome is conflicting. However, most research does find people with Down syndrome live highly sedentary lives in which they do not achieve the recommended guidelines for physical activity levels <ref name=":5">Esposito PE, MacDonald M, Hornyak JE, Ulrich DA. Physical activity patterns of youth with Down syndrome. Intellectual and developmental disabilities 2012 Apr;50(2):109-19.</ref><ref>Phillips AC, Holland AJ. Assessment of objectively measured physical activity levels in individuals with intellectual disabilities with and without Down's syndrome. PLoS One 2011 Dec 21;6(12):e28618.</ref>. The daily recommended levels of physical activity for children is at least 60 minutes of moderate to vigorous-intensity activity, and for adults the recommended levels is at least 150 minutes of moderate aerobic activity each week, including at least two strength session in the week <ref name=":6">WHO | Physical Activity and Adults [Internet]. Who.int. 2011 [cited 9 April 2018]. Available from: <nowiki>http://www.who.int/dietphysicalactivity/factsheet_adults/en/</nowiki></ref><ref name=":12">WHO | Physical activity and young people [Internet]. Who.int. 2011 [cited 9 April 2018]. Available from: <nowiki>http://www.who.int/dietphysicalactivity/factsheet_young_people/en/</nowiki></ref>. Although people with Down syndrome may have decreased capacity for exercise compared to their peers without DS, the guidelines clearly state that children with DS should still meet the recommended guidelines or do as much physical activity as they can manage <ref name=":9">Shields N, Blee F. Physical activity for children with Down syndrome. 2012.</ref>.
| |
| | |
| Furthermore, as people with DS age, their physical activity levels fall even further behind their peers without DS <ref name=":5" /><ref>Shields N, Dodd KJ, Abblitt C. Do children with Down syndrome perform sufficient physical activity to maintain good health? A pilot study. Adapted Physical Activity Quarterly. 2009 Oct;26(4):307-20.</ref><ref name=":11">Buckley S. Increasing opportunities for physical activity. Down Syndrome Research and Practice 2007;12:18-19.</ref>. This trend demonstrates that reduced activity levels are a lifelong issue for children with DS that must be addressed.
| |
| === Barriers to Physical Activity ===
| |
| Most individuals with Down’s Syndrome have to overcome social and environmental barriers to access physical activity. People with DS face many obstacles with the main barriers being lack of money, transportation, access to programs and support from family and carers. It is a common thought that people with DS are too fragile to participate in exercise. <ref name=":13">Barr M, Shields N. Identifying the barriers and facilitators to participation in physical activity for children with Down syndrome. Journal of Intellectual Disability Research. 2011 Nov 1;55(11):1020-33.</ref>.
| |
| | |
| Poor strength and balance are limitations to both cardiovascular and resistance exercise, however, this needs to be addressed as many individuals with DS are now being classed as obese. Individuals with Down syndrome have been found to have substantially higher rates of obesity compared to the general population <ref>Rimmer JH, Yamaki K, Davis BM, Wang E, Vogel LC. Peer reviewed: Obesity and overweight prevalence among adolescents with disabilities. Preventing chronic disease. 2011 Mar;8(2).</ref>. Often occurring early on in childhood, obesity was found to remain stable from childhood into adulthood, with slight increases after puberty <ref>Basil JS, Santoro SL, Martin LJ, Healy KW, Chini BA, Saal HM. Retrospective study of obesity in children with Down syndrome. The Journal of pediatrics. 2016 Jun 1;173:143-8.</ref>. Obesity is now recognized as a major health risk for people with Down syndrome <ref>Bull MJ. Health supervision for children with Down syndrome. 2011.</ref>.
| |
| | |
| The causes of obesity in the Down syndrome population can be divided into physiological causes and behavioural causes. Physiological causes may include conditions such as hypothyroidism, decreased metabolic rate, increased leptin levels (a hormone which helps regulate hunger), short stature and low levels of lean body mass <ref name=":7">Artioli T. Understanding Obesity in Down’s Syndrome Children. Journal of Obesity and Metabolism. 2017 1: 101.</ref>. Behavioural tendencies such as negative thinking and inattention behaviour may become barriers that prevent vital dietary and lifestyle changes to occur <ref name=":7" />.
| |
| | |
| [[File:Shelly Obesity Picture.png|center|frameless|519x519px]]
| |
| | |
| Physical inactivity also increases the chance for the development of other health problems such as diabetes, increased blood pressure, dyslipidaemia, early markers of cardiovascular disease, musculoskeletal disorders, breathing difficulties with worsening of sleep apnea and psychological effects including reduced quality of life <ref name=":6" /><ref name=":7" />. | |
| | |
| Aerobic fitness in both youth and adults with Down syndrome is reduced compared to their peers without DS <ref>Mendonca GV, Pereira FD, Fernhall BO. Reduced exercise capacity in persons with Down syndrome: cause, effect, and management. Therapeutics and clinical risk management. 2010;6:601.</ref><ref name=":8">Baynard T, Pitetti KH, Guerra M, Unnithan VB, Fernhall B. Age-related changes in aerobic capacity in individuals with mental retardation: a 20-yr review. Medicine and science in sports and exercise. 2008 Nov;40(11):1984-9.</ref>. Studies find that adolescents and young adults with DS have comparable aerobic fitness to non-DS older adults (60years +) with heart disease <ref name=":8" />. They also have lessened aerobic abilities, reduced muscular strength and reduced bone mineral density levels by 26% compared to their peers without DS <ref>Angelopoulou N, Matziari C, Tsimaras A, Sakadamis V, Mandroukas K. Bone mineral density nd muscle strength in young men with mental retardation. Calcified Tissue International 2000;66:176-180.</ref>.
| |
| | |
| === Benefits of Physical Activity ===
| |
| Overall, strong evidence suggests that regular physical activity can lead to numerous health benefits. Participating in physical activity has a positive impact on people’s health. Benefits include improved cardiovascular, metabolic, musculoskeletal and psychosocial health profiles in people with and without DS <ref>Rowland T. Physical activity, fitness, and children. Physical activity and health. 2007:259-70.</ref>.
| |
| [[File:Shelly Physical Activity2.png|center|frameless|708x708px]]
| |
| | |
| The fact that many children with DS reach Developmental Milestones later than their peers may be a contributing factor to lower levels of physical activity during infancy.<ref name=":10">Pitetti H, Baynard T, Agiovlasitis S. Children and adolescents with Down syndrome, physical fitness and physical activity. Journal of Sport and health Science 2013;2:47-57.</ref> Onset of independent walking in children with Down syndrome occurs roughly 1 year later in comparison to children with typical development <ref>Ulrich BD, Ulrich DA. Spontaneous leg movements of infants with Down syndrome and nondisabled infants. Child development. 1995 Dec 1;66(6):1844-55.</ref>. Earlier walking onset has been observed in infants with Down syndrome who performed greater amounts of high-intensity activity at 1 year of age <ref>Lloyd M, Burghardt A, Ulrich DA, Angulo-Barroso R. Physical activity and walking onset in infants with Down syndrome. Adapted Physical Activity Quarterly. 2010 Jan;27(1):1-6.</ref>. Changes to physical activity levels in infants with Down syndrome has been suggested to encourage motor development, validating the importance of early physiotherapy intervention <ref name=":10" />.
| |
| | |
| Some health benefits of increased physical activity levels in persons with DS are:
| |
| [[File:PA pyramid.jpg|right|frameless|324x324px|<ref>LifeSpan .Physical Activity Pyramid. 2015. [Picture].</ref>]]
| |
| * Decreased body fat percentage | |
| * Decreased body weight | |
| * Improved cardiovascular fitness | |
| * Improved muscle strength | |
| * Decreased depression
| |
| * Reduced risk of osteoporosis<ref name=":22">Ulrich DA, Burghardt AR, Lloyd M, Tiernan C, Hornyak JE. Physical activity benefits of learning to ride a two-wheel bicycle for children with Down syndrome: a randomized trial. Physical therapy. 2011 Oct 1;91(10):1463-77.</ref><ref>Rimmer JH, Heller T, Wang E, Valerio I. Improvements in physical fitness in adults with Down syndrome. American Journal on Mental Retardation. 2004 Mar;109(2):165-74.</ref><ref>Seron BB, Modesto EL, Stanganelli LC, Carvalho EM, Greguol M. Effects of aerobic and resistance training on the cardiorespiratory fitness of young people with Down Syndrome. Revista Brasileira de Cineantropometria & Desempenho Humano. 2017 Aug;19(4):385-94.</ref><ref name=":15">Heller T, Hsieh K, Rimmer JH. Attitudinal and psychosocial outcomes of a fitness and health education program on adults with Down syndrome. American Journal on Mental Retardation. 2004 Mar;109(2):175-85.</ref>
| |
| In addition to the health benefits listed above, physical activity is important for people with DS because it:
| |
| * Promotes the development of physical and social skills.
| |
| * Establishes a regular routine around being physically active, leading to better habits in the future.
| |
| * Increases life satisfaction.
| |
| * Prevents secondary conditions associated with DS including diabetes, osteoporosis and dementia <ref>Shields N. Getting Active: What Does it Mean for Children With Down Syndrome?. 2016.</ref>.
| |
| From the evidence, it is clear that physical activity is integral to a person with Down syndrome’s health, fitness and wellbeing <ref name=":9" />. If you feel unsure about what kind of activities to encourage your child to take part in, or would like to know what kind of physical activity groups are out there, then hopefully this next section will provide you with some useful information!
| |
|
| |
|
| | ''Optionally, learn more about [[Down Syndrome Developmental Milestones and Physical Activity]] on this page.'' |
| == Sensation == | | == Sensation == |
| In addition to the other challenges facing people with DS, they can also experience sensory issues <ref name=":17">BruniI M.. Fine motor skills for children with Down syndrome. 2nd ed. Bethesda: Woodbine House Inc., 2006.</ref>. Being unable to process sensory information from the environment can be both frustrating and challenging, often leading to inappropriate behaviour as a response <ref name=":29">Lashno M. Sensory integration: observations of children with Down syndrome and Autistic spectrum disorders. Disability Solutions 1999;3:31-35.</ref>. As humans, we use sensory information to gain experience, learn and interact with the world. When sensory feedback is limited, it can impact progress in other areas such as motor development <ref name=":17" />. Sensory difficulties can impact a child’s behaviour and the way they interact with people and objects around them <ref name=":29" />. | | In addition to the other challenges facing people with DS, they can also experience sensory issues.<ref name=":17">BruniI M.. Fine motor skills for children with Down syndrome. 2nd ed. Bethesda: Woodbine House Inc., 2006.</ref> Being unable to process sensory information from the environment (i.e. sensory integration) can be both frustrating and challenging, and often leads to inappropriate behaviour as a response.<ref name=":29">Lashno M. Sensory integration: observations of children with Down syndrome and Autistic spectrum disorders. Disability Solutions 1999;3:31-35.</ref> When sensory feedback is limited, it can impact progress in other areas such as motor development.<ref name=":17" /> Sensory difficulties can impact a child’s behaviour and the way they interact with people and objects around them.<ref name=":29" /> |
| [[File:Elizabeth Stick Men.jpg|center|frameless|615x615px|<ref>Scott R. Do you know me. 2015. [Picture]. <nowiki>https://psychprofessionals.com.au/sensory-processing-problem/</nowiki> (accessed 12 April 2018).</ref>]] | | [[File:Elizabeth Stick Men.jpg|center|frameless|615x615px|<ref>Scott R. Do you know me. 2015. [Picture]. <nowiki>https://psychprofessionals.com.au/sensory-processing-problem/</nowiki> (accessed 12 April 2018).</ref>]] |
|
| |
| === What is Sensory Integration? ===
| |
| Information from the environment is processed by our brain and can be interpreted by senses such as sound, touch and movement. The brain then organises this information before directing the body’s response; this is known as sensory integration. Typically, we are able to manage all this continuous processing without really having to think about it. People with Down syndrome aren’t always as able to sort through information, and they can quickly become overloaded and sensitive to stimuli. This is called being hyperresponsive and occurs when the brain ‘short-circuits’. Alternatively, the person could become immune to stimuli, or hyporesponsive, which occurs where the brain fails to register input <ref name=":18">Lashno M. Mixed signals: understanding and treating you child’s sensory processing issues. Baltimore: Woodbine House Inc, 2010. </ref>. It’s important to understand that people can’t always be neatly categorised into one or the other and crossover does occur.
| |
|
| |
| [[File:Elizabeth Senses2.jpg|center|frameless|407x407px|<ref>Smith-Myles B. Seven Senses. 2000. [Picture].http://blog.birdhousehq.com/sensory-integration-dysfunction-101/ (accessed 15 April 2018).</ref>]]
| |
|
| |
| ==== Hyperresponsive Behaviour ====
| |
| Most people enjoy a light touch from a loved one, whether a pat on the hand or a hair ruffle and a positive response is usually expected, particularly from children. However, some people with Down syndrome can register this as dangerous and may scream or pull away. This may seem like an over-reaction to me or you perhaps but is an appropriate response according to the brain of an individual with DS. You could compare it to us walking down a scary street at night where our bodies would be on full alert. If we spent every day in this heightened state of awareness, exploring the environment may become difficult and our reaction to certain scenarios may changes. Without this exploration, it becomes challenging to learn new skills <ref name=":18" />.
| |
|
| |
| ==== Hyporesponsive Behaviour ====
| |
| An individual whose brain fails to register input usually bombards the sensory system, typically by constantly touching objects. Pain is not felt in a ‘typical’ manner, by crying or touching the site of pain. Instead, the person may bump into the same object over and over. This may also lead to falling repeatedly. If we were in a pitch-black room and told to find a way out, we would call on our other senses – touch and sound for example. People who are hyposensitive are continuously using their brain in this intense way in order to make sense of their environment <ref name=":18" />.
| |
|
| |
|
| == Mental Health and Emotional Wellbeing == | | == Mental Health and Emotional Wellbeing == |
| It is not uncommon for individuals with Down syndrome to experience challenges with emotional behaviours and mental health. Children with Down syndrome may have difficulties with communication skills, problem-solving abilities, inattentiveness and hyperactive behaviours. Adolescents may be susceptible to social withdrawal, reduced coping skills, depression, anxiety, obsessive-compulsive behaviours and sleep difficulties. Adults with DS may have similar experiences as adolescents, with further complications of dementia later in life <ref>Van Germeren-Oosterom H, Fekkes M, Buitendijk S, Mohangoo A, Bruil J, Van Wouwe J. Development, problem behaviour, and quality of life in a population based sample of eight-year-old children with Down syndrome. Plos One 2011;6:7. </ref>. Listed below are different mental health conditions. | | It is not uncommon for individuals with DS to experience challenges with emotional behaviours and mental health. Children with DS may have difficulties with communication skills, problem-solving abilities, inattentiveness and hyperactive behaviours. Adolescents may be susceptible to social withdrawal, reduced coping skills, [[depression]], anxiety, obsessive-compulsive behaviours and [[Sleep Apnea|sleep difficulties]]. Adults with DS may have similar experiences as adolescents, with further complications of [[dementia]] and [[Alzheimer's Disease|Alzheimer's]] later in life <ref>Van Germeren-Oosterom H, Fekkes M, Buitendijk S, Mohangoo A, Bruil J, Van Wouwe J. Development, problem behaviour, and quality of life in a population based sample of eight-year-old children with Down syndrome. Plos One 2011;6:7. </ref>. |
| | == Physiotherapy Management and the Role of the Multidisciplinary Team == |
| | All members of the multidisciplinary team can play a major role in supporting individuals with DS by adopting a holistic approach to their diverse needs.<ref>CSP. What is physiotherapy. 2018. www.csp.org.uk/your-health/what-physiotherapy (accessed 14 April 2018).</ref> |
|
| |
|
| === Depression ===
| | Physiotherapists provide tailored interventions to improve physical abilities, strength, and balance, while occupational therapists focus on enhancing daily living skills, fine motor control, and sensory processing. Speech and language therapists help individuals with DS develop effective communication skills and address feeding and swallowing challenges. Psychologists support emotional and cognitive well-being, helping individuals and their families cope with challenges and develop strategies for long-term success. |
| Adolescents and adults, and sometimes children with Down syndrome may display depressive symptoms such as sadness, severe social withdrawal, or avoidance of activities that were previously enjoyable. These behaviours tend to be associated with an event that may seem like a normal life occurrence but is perceived as great stress to someone with Down syndrome. Such events may include the loss of a household pet, a friend or a sibling who moves away, an illness in the family, or the extended absence of a teacher. Individuals with Down syndrome can be particularly sensitive to changes in their environment and if they do not cope appropriately, this may cause significant psychological distress <ref name=":19">National Down Syndrome Society. Mental health issues and Down syndrome. <nowiki>https://www.ndss.org/resources/mental-health-issues-syndrome/</nowiki> (accessed 30 March 2018).</ref>. Challenges may arise including withdrawal from social and physical activities, which may prolong important development in these areas and impact the quality of life. There are a variety of treatment options for depression, including counselling, identifying coping methods for stressful events, medications, and participation in exercise and enjoyable activities <ref name=":16">National Down Syndrome Association. For families and carers: depression. <nowiki>https://www.downs-syndrome.org.uk/for-families-and-carers/health-and-well-being/depression-2/</nowiki> (accessed 02 April 2018).</ref>.
| |
| === Anxiety ===
| |
| Anxiety in a person with Down syndrome may be displayed by behaviours such as restlessness, panic, fidgeting or excessive worrying. Anxiety is often stimulated by the transition to a new or unfamiliar situation or environment. For example, going from home to a different environment such as school, a disruption of a daily routine, or anticipation of a new event <ref>Evans D, Canavera K, Kleinpeter F, Maccubbin E, Taga K. The fears, phobias and anxieties of children with autism spectrum disorders and Down syndrome: comparisons with developmentally and chronologically age matched children. Child Psychiatry and Human Development 2005;36:3-26.</ref>. This may prove to be a challenge when introducing new activities to individuals with DS so it is important to plan ahead and incorporate new activities gradually into the routine.
| |
| === Routinised and Compulsive-like Behaviours ===
| |
| Children and adults with Down syndrome have a tendency to follow familiar routines that may appear to be repetitive, compulsive or ritualistic <ref name=":0" />. They may require situations to be ‘just right’ or want to participate in the same activities over and over. These behaviours are often performed to avoid feelings of anxiety <ref>Glenn S, Cunningham C, Nananidou A, Prasher V, Glenholmes P. Routinised and compulsive-like behaviours in individuals with Down syndrome. Journal of Intellectual Disability Research 2015;59:1061-1070.</ref>. It is important to introduce physical and social activities early in life so they become part of an everyday routine. This can have a positive impact on achieving developmental milestones.
| |
|
| |
|
| === Hyperactive and Inattentive Behaviours ===
| | Effective physiotherapy management of DS typically involves a combination of sensory integration therapy, neurodevelopment treatment, perceptual-motor therapy and traditional strength and conditioning programmes.<ref name=":20">Down Syndrome Association. For Families and Carers. https://www.downs-syndrome.org.uk/for-families-and-carers/ (accessed 6 April 2018).</ref> Physiotherapists educate individuals and their families and provide input on health promotion and long-term condition management.<ref>CSP. Learning disabilities physiotherapy. Associated of Chartered Physiotherapists for People with Learning Disabilities. www.acppld.csp.org.uk/learning-disabilities-physiotherapy (accessed13 March 2018).</ref> Interventions are based on the individual’s physical and intellectual needs, as well as his or her personal strengths and limitations.<ref name=":1">National Human Genome Research Institute. Learning about Down syndrome. https://www.genome.gov/19517824/learning-about-down-syndrome/ (accessed 16 March 2018). </ref> Below are some examples of interventions for children with Down syndrome. |
| Children with Down syndrome may appear to be easily distracted, impulsive, frequently restless and they may have difficulty maintaining attention on tasks. This behaviour may persist into adulthood, however, it tends to diminish with age <ref>Selikowitz M. Down syndrome the facts. 2nd ed. Oxford: Oxford University Press, 1997. </ref>. It often causes a barrier to participation in physical activities due to non-compliance and creates the need for increased supervision <ref name=":13" />. There are medications which are said to reduce these behaviours, however, they often trigger adverse side effects. It may be beneficial to channel hyperactive energy into participating in activities that the child enjoys, or encourage an activity that provides a calming effect.
| |
| | |
| == Alzheimer's ==
| |
| Another challenge the brain can face for those with Down syndrome is Alzheimer’s which is the most common cause of dementia. These two terms, Dementia and Alzheimer’s, are commonly used interchangeably but are in fact different diseases. Dementia typically involves symptoms including memory loss, difficulties with thinking, problem-solving and/or language and these occur due to damage to the brain such as that caused by Alzheimer’s. Down syndrome is not the same as Alzheimer’s nor does it guarantee the development of Alzheimer’s! Current estimates state that roughly 50% of people with Down syndrome will develop dementia due to Alzheimer’s as they age and symptoms only begin to show in the individuals 50s or 60s <ref>National Institute on Ageing. Alzheimer’s disease in people with Down syndrome. <nowiki>https://www.nia.nih.gov/health/alzheimers-disease-people-down-syndrome</nowiki> accessed 23 March 2018).</ref>.
| |
| | |
| There has been a lot of research on the link between Down syndrome and Alzheimer’s. Alzheimer’s is a physical disease of the brain caused by a build-up of a protein which forms plaques or tangles. As mentioned earlier people with DS have an extra copy of chromosome 21 which carries a certain gene. This gene produces a protein called amyloid precursor protein (APP) which leads to the aforementioned plaques/tangles in many persons with DS <ref name=":19" />. These plaques/tangles can cause a loss of connections between brain cells, leading to a loss in brain tissue. People with Alzheimer’s also have reduced amounts of certain chemicals in their brain which help to transmit signals in the brain, leading to less effective signal transmitting.
| |
| | |
| Some common symptoms of Alzheimer’s:
| |
| * Short-term memory loss
| |
| * Reduced interest in activities
| |
| * Social withdrawal
| |
| * Confusion and disorientation
| |
| * Increase in wandering
| |
| * Increased problems in unfamiliar places
| |
| == Physiotherapy Management ==
| |
| Physiotherapy can play a major role in the management of children with DS; through movement and exercise, manual therapy, and education physiotherapists can empower people to take charge of their own health and participate in their treatment. The aim of treatment is to assist people to live as independently as possible <ref>CSP. What is physiotherapy. 2018. www.csp.org.uk/your-health/what-physiotherapy (accessed 14 April 2018).</ref>.
| |
| | |
| Not everyone with DS requires physiotherapy and as with most things in life, it depends on the individual's needs. Although there is no standard treatment plan, effective physiotherapy management of Down syndrome typically involves a combination of sensory integration therapy, neurodevelopment treatment, perceptual-motor therapy and traditional strength and conditioning programs <ref name=":20">Down Syndrome Association. For Families and Carers. https://www.downs-syndrome.org.uk/for-families-and-carers/ (accessed 6 April 2018).</ref>.
| |
| | |
| Traditional therapies for conditions involving difficulties with movements can be repetitive and lack variety <ref name=":23">Wuang YP, Chiang CS, Su CY, Wang C. Effectiveness of virtual reality using Wii gaming technology in children with Down syndrome. Res Dev Disabil 2011;32:312-321.</ref>. People with Down syndrome often have a reduced attention span, which makes engaging in any therapy challenging, especially when dealing with children <ref>Lott I, Dierssen M. Cognitive deficits and associated neurological complications in individuals with Down syndrome. Lancet Neurol. 2010;9:623-633.</ref>. By consistently exposing children to different textures, sounds, environments and movements, physiotherapists can make treatment more interesting and inclusive.
| |
| | |
| Physiotherapists are commonly consulted to educate individuals and their families as well as provide input on health promotion and long-term condition management <ref>CSP. Learning disabilities physiotherapy. Associated of Chartered Physiotherapists for People with Learning Disabilities. www.acppld.csp.org.uk/learning-disabilities-physiotherapy (accessed13 March 2018).</ref>. As many treatments often require on-going maintenance, physiotherapists should encourage family members to support and implement home treatment plans in an attempt to encourage self-management <ref>Middleton J, Kitchen S. Factors affecting the involvement of day centre staff in the delivery of physiotherapy to adults with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities 2008:21:227-235. www.onlinelibrary.wiley.com/doi/10.1111/j.1468-3148.2007.00396.x/epdf (accessed 11 March 2018).</ref>. Due to the variation in all people and across Down syndrome cases, no one physiotherapy intervention can be prescribed. Interventions are based on the individual’s physical and intellectual needs, as well as his or her personal strengths and limitations <ref name=":1" />. Some of the common issues that physiotherapists will address are: | |
| * Delayed developmental milestones
| |
| * Balance issues
| |
| * Decreased strength
| |
| * Reduced levels of physical activity
| |
| * Issues with sensation
| |
| * Reduced mental health and emotional well-being
| |
| * High chance of Alzheimer’s disease
| |
| Choosing the right intervention based on the problems experienced and the individual child is essential to improve the outcome of treatment. Below are some examples of effective interventions for children with Down syndrome.
| |
| | |
| === Tummy Time ===
| |
| Infancy is the ideal time to start encouraging movement and motor skills. These skills promote interaction between the child and the environment which will improve cognition, language, social skills and independence. Due to the already high risk of developmental delays in infants with DS, this is an especially important area of focus <ref name=":28">Wentz R. The impact of an early and intense prone positioning program in infants with and without Down syndrome. The University of Michigan 2016. https://deepblue.lib.umich.edu/bitstream/handle/2027.42/133421/erinengw_1.pdf?sequence=1&isAllowed=y (accessed 22 March 2018).</ref>.
| |
| | |
| Tummy Time is a simple physiotherapeutic intervention used for infants with DS. Parents are encouraged to position the child on his tummy in various positions for extended periods of time. Lying in this position has been found to be extremely beneficial, as it affords infants the chance to develop strength, balance and motor skills against gravity. When this technique is practiced, the infant often achieves motor milestones, such as rolling, sitting and crawling, and improved balance earlier in life. Infants who do not experience enough time on their belly have decreased ability to support their own head at 2 months of age and have further delayed developmental milestones <ref>Wentz E. Importance of initiating a tummy time intervention early in infants with down syndrome. Paediatric Physical Therapy 2017;29:68-75. <nowiki>https://journals.lww.com/pedpt/Fulltext/2017/01000/Importance_of_Initiating_a__Tummy_Time_.20.aspx?WT.mc_id=HPxADx20100319xMP</nowiki> (accessed viewed 18 March 2018).</ref>. Some of the possible positions are pictured and described below:
| |
| [[File:Tummy time 3.png|center|frameless|791x791px|<ref>Wentz E. Tummy Time Positions. 2017. [Picture]. <nowiki>https://journals.lww.com/pedpt/Fulltext/2017/01000/Importance_of_Initiating_a__Tummy_Time_.20.aspx?WT.mc_id=HPxADx20100319xMP</nowiki> (accessed viewed 18 March 2018).</ref>]]
| |
| Tummy Time in children without DS has been proven to be a positive contributor to mastering developmental milestones. This intervention has only recently been investigated specifically for children with DS. There are only a few research studies available, but results have been consistently positive. Tummy time should be started as early as possible in infants with DS. When a child with DS begins this intervention within the first ten weeks of life, levels of motor development similar to that of half the children without DS are experienced. This technique is easily started at birth and can be performed by parents or caregivers. It is the foundation to motor skill mastery in the first year of life and increases balance, strength and skill attainment as the child grows <ref name=":28" />.
| |
| | |
| Further information on tummy time positions is available '''[http://dsdaytoday.blogspot.co.uk/2011/03/tummy-time.html here]'''<ref>Durkin A. Tummy Time. www.dsdaytoday.blogspot.co.uk/2011/03/tummy-time.html (accessed 6 April 2018).</ref>.
| |
| | |
| === Neurodevelopmental Treatment (NDT) ===
| |
| NDT is an approach which focuses on the quality of movement and coordination rather than individual muscle group function <ref name=":24">Velickovic TD, PERAT MV. Basic principles of the neurodevelopmental treatment. Medicina 2005;42:112-120.</ref>. Therefore, NDT is most effective as an early intervention, before poor compensatory patterns of movement become habitual. As physiotherapists, we can use our hands both to prevent abnormal movement patterns and to facilitate more natural ones. This hands-on approach is achieved by the physiotherapist having several ‘key points of control’, including the head, shoulders, trunk and/or pelvis to guide and alter movement <ref name=":24" />. NDT is usually appropriate for people with DS as they often present with limbs and muscles that may not be as well-controlled and may be floppier than desired <ref name=":23" />.
| |
| | |
| Although NDT will be different for every individual, a video with some examples of what a more hands-on therapy approach can look like is seen below.
| |
| | |
| {{#ev:youtube|xDUvmhaYr98}}
| |
| | |
| === Sensory Integration Therapy (SIT) ===
| |
| People with Down syndrome often struggle to process information from the environment including things like smell, touch and movement. This is known as sensory integration dysfunction. SIT aims to change how the brain interprets the environment through the very aspects in which they struggle, touch, movement and balance <ref name=":21">Smith J, Weaver L, Fristad M. A systematic review of sensory integration training interventions for children with Down syndrome. Sage Journals 2015;5:10-14.</ref>. The video below explains these systems and why they are important in everyday life!
| |
| | |
| {{#ev:youtube|1_Iuj8dr9oY}}
| |
| | |
| SIT involves a wide range of activities and equipment such as weighted vests, brushes, swings, balls, homemade obstacle courses <ref>Zimmer M, Desch L. Sensory integration therapies for children with developmental and behavioural disorders. Paediatrics 2012;129:1186-1189. <nowiki>https://www.ncbi.nlm.nih.gov/pubmed/22641765</nowiki> (accessed 7 April 2018).</ref> and even game consoles such as the Wii<ref name=":23" />. These items are all used to provide some form of sensory stimulation. This interactive therapy has been shown to increase focus, reduce disruptive behaviours and improve high functioning tasks such as reading, writing and speech <ref name=":21" />.
| |
| | |
| If SIT is identified as a modality it may be beneficial to work alongside an occupational therapist (OT) . OTs are concerned with how people manage to do meaningful activities and can help by providing equipment which ultimately aims to promote independence.
| |
| | |
| Traditionally seen as more of an ‘OT thing’ understanding of how sensory-based issues can impact motor performance can enhance our practice as physiotherapists, particularly when working with children. There is now a physiotherapy special interest group which offers peer support and shared learning for physiotherapists wanting to gain more experience in, and to promote the role of physiotherapy in SIT <ref>Sensory integration education. About us. 2013. <nowiki>https://www.sensoryintegration.org.uk/About-us</nowiki> (accessed19 April 2018).</ref>.
| |
| | |
| === Perceptual-Motor Therapy (PMT) ===
| |
| PMT incorporates activities which help to explore balance, coordination and body awareness and is not skills-based. So, rather than being taught a certain skill, individuals are provided with an environment in which to explore and determine what their bodies can do <ref name=":30">Stein D. Behaviour and Down syndrome: a practical guide for parents. Boston: Children’s Hospital Boston, 2002.</ref>. See video below:
| |
| | |
| {{#ev:youtube|222WIhX4dV0}}
| |
| | |
| === Two-Wheeled Bicycle Training ===
| |
| Two-Wheeled Bicycle riding helps to improve physical activity, is enjoyable and can lead to increased socialization. The skill of bicycle riding can be learned at a young age or later in life <ref name=":5" />. Studies have shown that people with Down Syndrome often have reduced physical activity levels <ref name=":10" />, along with reduced sports participation. Assisted two-wheeled bicycle riding has been shown to reduce sedentary time and increase time participating in moderate to vigorous activity <ref name=":22" />. As well, this skill has the potential to increase independence and autonomy, whilst helping to diminish their fears surrounding falling from a bike and getting hurt <ref name=":22" />. If you are searching for an activity for your family to do together, that has the potential to improve your child’s quality of life <ref>Ringenbach S, Holzapfel G, Mulvey A, Jimenez A, Benson S, Richter M. The effects of assisted cycling therapy and voluntary cycling on reaction time and measures of executive function in adolescents with Down syndrome. JIDR 2016;60:1073-1080.</ref>, then assisted two-wheeled bicycle riding could be a great activity to try out!
| |
| | |
| === Therapeutic Horseback Riding (Hippotherapy) ===
| |
| This is an activity that promotes friendship, fun and progresses confidence with movement skills. Therapeutic horseback riding is a strategy that uses a horse’s motion to promote the training of muscle and balance skills required for everyday life activities <ref name=":25">Giagazoglou P, Arabatzi F, Dipla K, Liga, M, Kellis E. Effect of a hippotherapy intervention program on static balance and strength in adolescents with intellectual disabilities. Res Dev Disabil 2012;33:2265-2270.</ref>. While horse riding, the child will experience movements of the trunk, pelvis and hips, similar to those that would take place during normal walking <ref>Winchester P, Kendall L, Peters H, Sears N, WINKLEY T. The effect of therapeutic horseback riding on gross motor function and gait speed in children who are developmentally delayed. Physical and Occupational Therapy in Pediatrics 2002;22:37-50.</ref>. Adapting to the horse’s rhythmic movements in different directions further enhances muscle contraction, postural control, weight shifting, and planning of movement patterns <ref name=":26">Champagne D, Dugas C. Improving gross motor function and postural control with hippotherapy in children with Down syndrome: case reports. Physiotherapy Theory Practice 2010;26:564-571.</ref>.
| |
| | |
| The overall benefits of therapeutic horseback riding include advances in balance, muscle strength and coordination, trunk control, postural stability, and weight-bearing abilities <ref name=":25" />. Learning new movement strategies through horse riding can also progress skills such as walking, running and jumping <ref name=":26" />. For more information, please see the video below
| |
| | |
| {{#ev:youtube|PsZLwXSUGUQ}}
| |
| | |
| === Treadmill Training ===
| |
| <blockquote>"The key is if we can get them to walk earlier and better then they can explore their environment earlier and when you start to explore, you learn about the world around you" <ref name=":27">Ulrich DA, Ulrich BD, Angulo-Kinzler RM, Yun J. Treadmill training of infants with Down syndrome: evidence-based developmental outcomes. Pediatrics. 2001;108(5):85.</ref></blockquote>
| |
| | |
| Infants with typical development learn to walk independently at about 12 months of age. Babies with Down syndrome typically learn to take independent steps at 24-28 months. These are averages, and averages and developmental milestones often feel like a ticking clock to race against. It is important to reassure parents not to worry if their child is late reaching milestones, and reinforce that each person develops at his or her own pace.
| |
| | |
| Helping children to walk is of importance as it allows interaction with the world and it is often a stepping stone to the development of other social, motor and cognitive skills. Walking allows children to engage in other enjoyable tasks, and the endurance achieved in doing so allows them to be active for longer periods of time! More skilled walking is less tiring for children and could allow for more energy to take on the rest of the day.
| |
| | |
| Research carried out in recent years has suggested that regular walking on a treadmill can significantly improve standing and walking ability in children with DS. Put simply, different research groups have used treadmill training, with varying degrees of speed, time length and frequency and concluded that it is a beneficial intervention for development as well as physical activity <ref name=":27" />.
| |
| | |
| Have a look at the children’s development in the video below
| |
| | |
| {{#ev:youtube|03_ZFLPRlEE}}
| |
| | |
| What’s great about treadmill training is that physiotherapists can prescribe it to be carried out in a family's home. This allows parents and carers to include walking practice around the family’s busy schedule and to suit the child. In addition, it promotes their involvement in their child’s development.
| |
| === Physiotherapy Interventions Developmental Milestones ===
| |
| Physical characteristics of the child with DS such as low muscle tone, loose joints and decreased strength may influence the speed of mastery or alter the form of the developmental milestone. Persons with DS generally naturally overcome these challenges through perseverance <ref name=":0" />.
| |
| | |
| The goal of physiotherapy is not to ‘speed up’ the rate of development. It is simply to facilitate the development of optimal movement patterns. Depending upon capabilities and adaptations made, physical compensations such as pain or inefficient walking patterns may occur. of a physiotherapist is to provide the building blocks to develop a solid physical foundation for movement and exercise that your family member can build on for life.
| |
| [[File:Building Blocks 3.jpg|center|frameless|493x493px]]
| |
| Physiotherapy sessions focusing on developmental milestones should be specifically tailored to each child’s current level of development. It is important to observe the child’s abilities and determine what skills should be learned next. As each person is different, skills should be taught in the way the child learns best. It is important that tasks are broken into smaller parts and practiced using different methods based on individual learning styles and physical make up.
| |
| | |
| ==== Encouraging the Family to Get Involved ====
| |
| It is important to get family members involved with treatment. Practice at home is essential for mastery, and engaging family participation is key. You can teach the family to:
| |
| | |
| * Use their child’s interests to encourage new skill development
| |
| * Build on already mastered skills
| |
| * Focus on what their child is willing to learn
| |
| * Practice often
| |
| * '''Be patient'''
| |
| === Physiotherapy Interventions for Balance ===
| |
| There are a wide range of physiotherapy interventions that can help improve balance. Some of them have been used for many years, while others are still developing and being introduced. Some common traditional physiotherapy interventions to improve balance in persons with DS are:[[File:Yoga DS.jpg|right|frameless|490x490px|<ref>Clique Images. Yoga for Girls with Down syndrome. 2015. [Picture]. <nowiki>https://www.stocksy.com/1490017/yoga-for-girls-with-down-syndrome</nowiki> (accessed 21 March 2018).</ref>]]
| |
| * Stability Exercise (examples available '''[https://www.nhs.uk/Livewell/fitness/Pages/balance-exercises-for-older-people.aspx here]'''<ref>NHS. Balance Exercises. https://www.nhs.uk/Livewell/fitness/Pages/balance-exercises-for-older-people.aspx (accessed 20 March 2018).</ref>)
| |
| * Corrective positioning (examples available '''[https://www.youtube.com/watch?v=T6Mmv0-ShHU here]'''<ref>Down Syndrome Awareness. Our beautiful son with Down syndrome at Physical Therapy [Video]. 2011. https://www.youtube.com/watch?v=T6Mmv0-ShHU<nowiki/>(accessed 15 March 2018).</ref>)
| |
| * Stair climbing
| |
| * Yoga
| |
| * Hydrotherapy <ref>Gupta S, Rao B, Kumaran S. Effect of strength and balance training in children with down syndrome: a randomized control trial. Clinical Rehabilitation 2011;25:425-432. www.journals.sagepub.com/doi/pdf/10.1177/0269215510382929 (accessed 19 March 2018). </ref><ref name=":4" />
| |
| Some new emerging physiotherapy interventions being used to improve balance are:
| |
| * Hippotherapy
| |
| * Treadmill training
| |
| * Two-wheel bicycle training
| |
| * Tummy Time
| |
| * Perceptual-motor therapy
| |
| * Sensory integration training
| |
| ==== Encouraging the Family to Get Involved ====
| |
| # Practice Makes Perfect: As with everything in life, practice will improve performance. While it often takes more practice to improve performance of balance in a child with DS, it is possible to increase both speed and accuracy of movement.
| |
| # Encourage Independent Movement: When a person actively initiates a movement, the brain learns how to control the area being moved. This improves coordination and task performance.
| |
| # Follow Individual Interests: A child is more likely to eagerly participate if the activity is one that is enjoyed. Try encouraging the family to incorporate balance training into sports and games.
| |
| # The Earlier the Better: Starting balance practice early in a child’s life will allow for a greater amount of learning time and increase muscle strength at a young age.
| |
| # It’s Never Too Late: Though it is harder to correct learned bad habits, practice at any time is helpful. It is never too late to start.
| |
| # Individuals with DS are more commonly visual learners. This means that they learn better by watching others or copying what they can see rather than responding to verbal instruction. Copy cat is a great game to help a family teach their child new tasks <ref>Welsh TN, Elliot D. The processing speed of visual and verbal movement information by adults with and without Down syndrome. Adapted Physical Activity Quarterly 2001;18:156-167.</ref>
| |
| === Physiotherapy Interventions for Strength ===
| |
| Physiotherapy has been quite successful in strength interventions with persons who have DS. There are many techniques that can be used and resources which can be explored. Some of the most common methods to increase strength are:
| |
| {| class="wikitable"
| |
| !'''<u>Method</u>'''
| |
| !'''<u>Description</u>'''
| |
| |-
| |
| |'''Endurance training'''
| |
| |Large groups of muscles working at moderate intensity for a more extended period
| |
| |-
| |
| |'''Weight training'''
| |
| |Small groups of muscles working at high intensity for a short period of time
| |
| |-
| |
| |'''Specific muscle training'''
| |
| |Targeting specific weak muscles<ref>Rimmer J, Heller T, Wang E, Valerio I. Improvements in physical fitness in adults with Down syndrome. Am J Ment Retard. 2004;109:165-174</ref>
| |
| |}
| |
| Each of these techniques has been shown to equally increase exercise capacity, health and quality of life in individuals with DS <ref>Spruit M, Gosselink R, Trooster T. Resistance vs endurance training in patients with COPD and peripheral muscle weakness. Eur Respir J 2002;19:1072-1078.</ref>. While these general workout types work well to increase strength, physiotherapists can also offer more specific exercises based on your child’s needs. Below are evolving exercise ideas you can discuss with your physiotherapist or read more about later in the wiki:
| |
| * Tummy time | | * Tummy time |
| * Treadmill training | | * [[Bobath Approach|Neurodevelopmental treatment (NDT)]] |
| * Falls prevention exercises <ref>Croce R, Pitetti K, Horvat M. Peak Torque, average power, and hamstrings/quadriceps ratios in nondisabled adults and adults with mental retardation. Arch Phys Med Rehabil 1996;77:369-372.</ref>
| | * Sensory integration therapy (SIT) |
| | | * Perceptual-motor therapy (PMT) |
| ==== Encouraging the Family to Get Involved ====
| |
| In order to achieve good results, it is important to advise the family on specific exercises, and correct technique. Increasing compliance to exercise will have positive benefits and can help with improving strength and development:
| |
| * Start early: Encourage the family to introduce strength training from a young age, this may help avoid later complications
| |
| * Encourage family members to do exercises with the child.
| |
| * Encourage other types of activities that can build strength such as sports
| |
| * Incorporate strength training into things a child enjoys <ref>Lewis C, Fragala-Pinkham M. Effects of aerobic conditioning and strength training on a child with Down syndrome: a case study. Pediatric Physical Therapy 2005;17:30-36.</ref>.
| |
| | |
| === Physiotherapy and Physical Activity ===
| |
| Physiotherapists can play a role in encouraging preventative health promotion with their patients who have DS. According to the World Health Organisation <ref>World Health Organisation. Global recommendations on physical activity for health. 2017. www.who.int/dietphysicalactivity/factsheet_recommendations/en/ (accessed 28 March 2018).</ref>, the recommended daily physical activity requirements for children is at least 60 minutes of moderate to vigorous intensity daily physical activity. Your physiotherapist can help recommend specific activities suitable for your child and direct you to resources in your area!
| |
| | |
| {| class="wikitable"
| |
| !
| |
| !Moderate Activity
| |
| !Vigorous Activity:
| |
| |-
| |
| |Aim
| |
| |Increase heart rate and breathing. May cause a light sweat
| |
| |Make the heart and lungs work harder than moderate intensity activity
| |
| |-
| |
| |Example
| |
| |
| |
| * Brisk Walking
| |
| * Active Play
| |
| * Slow Bicycling
| |
| * Water aerobics
| |
| * Slow Dancing <ref name=":12" />
| |
| |
| |
| * Swimming
| |
| * Tennis
| |
| * Running
| |
| * Fast Bicycling
| |
| * Faster Dancing
| |
| * Hiking
| |
| |}
| |
| Evidence is also growing to support other fun and creative physiotherapy interventions for your child to be physically active including:
| |
| * Treadmill Training
| |
| * Two-Wheeled Bicycle Riding
| |
| * Therapeutic Horseback Riding (Hippotherapy)
| |
| Structured accessible programs that make adaptations for children with DS have been identified as key to facilitating participation in physical activity <ref name=":13" />. As well, it has been recommended that introducing diverse and interesting physical activity programmes which avoid over-complicated tasks, may be more enjoyable for people with DS <ref>Merzbach V, Gordon D. The benefits of exercise to a Down’s Syndrome population [Internet]. Intellectualdisability.info. 2015 [cited 8 April 2018]. Available from: <nowiki>http://www.intellectualdisability.info/physical-health/articles/the-benefits-of-exercise-to-a-downs-syndrome-population</nowiki></ref>.
| |
| | |
| It is important to be aware of the percentage of people with Down Syndrome, reported between 8-63%<ref>Hankinson, T., Anderson, R., 2010. Craniovertebral Junction Abnormalities in Down Syndrome. ''Neurosurgery'', 66(3), pp.A32-A38.</ref>, who have structural abnormalities in the upper cervical spine known as [[Craniocervical Instability in Down Syndrome|Craniocervical instability]] (CCI; see page for details). This is an umbrella term that encompasses Atlanto Axial Instability (AAI) and Occipital-axial instability (OAI). Mostly, CCI is asymptomatic but there is potential for severe neurological damage if the cervical spine impinges onto the spinal cord. Due to this possibility, precaution must be taken when advising exercise to people with Down Syndrome with AAI to mitigate risk of injury: including restricting certain high-risk sporting activity (including, but not limited to: gymnastics, contact sport, diving and trampolining)<ref>Committee on Sports Medicine and Fitness, 1995. Atlantoaxial instability in Down syndrome: subject review. ''Pediatrics'', ''96''(1), pp.151-154.</ref>. Although extremely rare, it is essential that all individuals involved in the person’s activity and care are aware of the signs of symptomatic CCI (such as progressive myelopathy) and seek emergency medical intervention if suspected.<ref>Cohen, W.I., 2006, August. Current dilemmas in Down syndrome clinical care: Celiac disease, thyroid disorders, and atlanto‐axial instability. In ''American Journal of Medical Genetics Part C: Seminars in Medical Genetics'' (Vol. 142, No. 3, pp. 141-148). Hoboken: Wiley Subscription Services, Inc., A Wiley Company.</ref>
| |
| | |
| ==== Encouraging the Family to Get Involved ====
| |
| One of the most important facilitators identified for improving physical activity participation levels of people with Down syndrome is the support and motivation they receive from their family and carers <ref name=":13" />. Some parents who were interviewed felt their child was more likely to be active when the physical activity was enjoyable and included being with friends or their siblings <ref name=":11" /><ref name=":14">Menear K. Parents’ perceptions of health and physical activity needs of children with Down syndrome. Down Syndrome Research and Practice. 2007 Jul 30;12(1):60-8.</ref>. Introducing physical activities into a child’s routine will increase familiarity and facilitate increased levels of participation <ref>Mahy J, Shields N, Taylor NF, Dodd KJ. Identifying facilitators and barriers to physical activity for adults with Down syndrome. Journal of Intellectual Disability Research. 2010 Sep 1;54(9):795-805.</ref>. Encouraging the family to keep an activity or exercise log and organising a routine check as well as providing positive feedback, has previously been a suggested as a helpful method to increase motivation towards physical activity participation <ref name=":14" />.
| |
| | |
| Other tips to help encourage children to be physically active include:
| |
| * Choose an activity that the child will enjoy or wants to do.
| |
| * Encourage childhood games that are traditional and active such as hopscotch, hide and seek or obstacle courses.
| |
| * Use simple ways to get children to be more physically active in daily life such as walking to school, taking the stairs instead of the lift or walking the family dog.
| |
| * Keep things simple; running, jumping, dancing are great physical activities to build a child’s fitness and there are no-cost requirements! Encourage parents to join in and get fit too!
| |
| * Give your child lots of positive and encouraging feedback. <ref name=":9" />.
| |
| === Physiotherapy Interventions for Sensory Problems ===
| |
| Physiotherapists have recently become more involved in the treatment of sensory issues. While this field is still growing, there are a few areas in which physiotherapy has been successful:
| |
| * Advice on desensitisation and calming procedures
| |
| * Provision of sensory-specific activities
| |
| * Creation of sensory and behavioural strategies
| |
| * Sensory integration therapy (SIT) - which will be discussed in depth later in the wiki | |
| ==== Encouraging the Family to Get Involved ====
| |
| Here are some ideas for incorporating therapy into everyday activities:
| |
| * When brushing teeth at night, try using a vibrating toothbrush to increase tolerance of stimuli.
| |
| * Before doing errands, such as taking their child to the hairdressers, try giving them some chewy sweets for the different texture.
| |
| * Encourage children to participate during meal prep or baking; perhaps by mixing ingredients of different textures or carrying pots and pans of different sizes.
| |
| * Encourage the family to involve their child in grocery chores; may allow the child to push the trolley at the grocery and help with packing and putting food away.
| |
| * Drinking through a straw, a weighted lap blanket or a big squishy seat cushion can all expose children to different sensory experiences while eating.
| |
| * With bathing, encourage parents to try out different brushes, cloths and soaps. Using crazy soap or shaving foam to draw on the wall is an excellent activity. After bath time wrapping a child tightly in a towel and apply pressure is another way to promote sensory activities. A hug works well, if tolerated! | |
| * Suggest playtime games like the ‘sandwich game’ – lie the child in between two pillows so they are effectively the sandwich filling and apply pressure on top to their liking. Any home-made obstacle courses involving jumping, crawling, hopping etc. are usually fun and will be beneficial <ref>Star Institute. Home activities for sensory processing disorders. <nowiki>https://www.spdstar.org/basic/home-activities</nowiki> (accessed 23 March 2018).</ref>.
| |
| Another idea is to create a ‘sensory corner’ which can be effective in reducing stress and produce a safe zone for some children. It can provide stimulation for a hyporesponsive person or create a comfortable retreat for a hyperresponsive person. Making a sensory corner is easy! Just block off a corner of a room and use soft furnishings with different textures. For example, use different carpets and pillows. Often a large beanbag or weighted blanket can provide deep pressure that can have a calming effect. Objects like lava lamps, or aquariums may be visually relaxing. Music or a sensory box filled with various objects that differ in texture and weight can be useful. Each person is unique. An example of a sensory room and sensory box are depicted below: [[File:Sensory Games.jpg|center|frameless|652x652px]]
| |
| | |
| === Physiotherapy Interventions for Mental Health and Well-being ===
| |
| Physical activity has demonstrated excellent benefits for the mental well-being of individuals with Down syndrome. The benefits include greater life satisfaction, reduced risk of depression, increased self-esteem, and improved social and behavioural skills <ref name=":15" /><ref name=":13" />. Any activity that promotes social interaction and friendship will further enhance mental and emotional well-being. Some recommended interventions are:
| |
| * Therapeutic Horseback Riding (Hippotherapy)
| |
| * Two-wheeled bicycle training | | * Two-wheeled bicycle training |
| * Sensory integration training | | * [[Hippotherapy|Therapeutic horseback riding (hippotherapy)]] |
| * Perceptual-motor therapy
| | * Treadmill training |
| * Hydrotherapy
| | * [[Balance Training|Balance training]] |
| * Yoga
| | * [[Strength Training|Strength training]] |
| | | * [[Physical Activity|Physical activity]] |
| ==== Encouraging the Family to Get Involved ====
| |
| * Work with the family to develop a behaviour treatment plan.
| |
| * Encourage the family to take opportunities to interact with others! While most people learn the majority of their social skills in school and work, people with Down syndrome need to “make every contact count”. Whether it is in therapy, school, work or at home, the opportunity to learn is everywhere!
| |
| * Support groups and therapies are a fantastic way of hitting two bases at once; therapy and socialising.
| |
| * Encourage families to develop a routine and stick to it. Try using visual schedules! This method uses pictures or books to help prepare for upcoming events such as beginning a new school year, going to a friend’s party or moving into a new house.
| |
| * Plan for difficult situations. Try using social stories!
| |
| * Where possible encourage the family to promote positive interactions and reduce the negative ones. Make time for fun every day!
| |
| * Explain the importance of encouraging positive behaviours and positive attitudes <ref name=":0" /><ref name=":16" /><ref name=":30" />
| |
| Below is an example of a visual schedule. [[File:Mental Health Pic 1.png|center|frameless|633x633px]]
| |
| | |
| === Physiotherapy Interventions and Alzheimer's ===
| |
| There is no specific physiotherapy treatment for Alzheimer’s, but there are some measures that can be taken to assist in controlling this disease. Physiotherapists can:
| |
| * Promote physical activity to delay the onset of Alzheimer’s | |
| * Encourage continued activities of daily living to prevent motor changes associated with Alzheimer’s | |
| * Assist families in planning for caring for their family member with DS and Alzheimer’s
| |
| * Refer families to specialty services for Alzheimer’s <ref>Barnhart R, Connolly B. Agining and Down syndrome: implications for physical therapy. Physical Therapy 2007;87:1399-1406. <nowiki>https://academic.oup.com/ptj/article/87/10/1399/2742283</nowiki> (accessed 28 March 2018).</ref>
| |
| Another aspect in which physiotherapists have recently been involved is Alzheimer’s screening programs for persons with DS. Since Alzheimer’s is so commonly associated with DS, physiotherapists along with other health professionals have begun running yearly screening clinics. These involve simple interviews and routine health checks to identify people at risk of developing Alzheimer’s. This is a great way to keep on top of this possible problem <ref>Backer C, Jervis N. A screening programme for adults with Down syndrome. Nursing Times 2007;10. <nowiki>https://www.nursingtimes.net/a-screening-programme-for-adults-with-downs-syndrome/199994.article</nowiki> (accessed 5 April 2018).</ref>.
| |
| | |
| ==== Encouraging the Family to Get Involved ====
| |
| While there is nothing that can be done to prevent the development of Alzheimer’s, the best defence is awareness. Changes in a person's actions, memory or communication can be signs that something may be wrong.
| |
| | |
| Encourging yearly DS screening clinics will help people to monitor changes and get an early warning should they be at risk of developing the disease. Encourage the family to read up on Alzheimer’s and create a possible plan in advance may minimize future stress.
| |
| | |
| Advise clients about the websites for the [https://www.ndss.org/resources/alzheimers/ National Down syndrome Society] and [https://www.alz.org/dementia/down-syndrome-alzheimers-symptoms.asp The Alzheimer’s Association], they may find them helpful.
| |
| == Other Challenges Associated With Down Syndrome ==
| |
| | |
| === Reduced Social Interaction ===
| |
| | |
| Although not a Physiotherapy issue as such, it’s worth mentioning that the social lives of persons with Down syndrome can be very different from others. Managing many of the physiotherapy issues mentioned above requires time and effort spent in therapy and carrying out home practice. As a result, persons with DS often find themselves meeting and interacting with their peers less often than non-DS persons. This is something to consider as meeting others is important for developing social and life skills.[[File:Social Skills.jpg|right|frameless|369x369px|<ref>Blue Hippo Group .Plan Ahead. 2015. [Picture].</ref>]]
| |
| Social skills which can differ in people with DS include:
| |
| * Social understanding and empathy
| |
| * Friendship making
| |
| * Play and leisure skills
| |
| * Personal and social independence
| |
| * Socially appropriate behaviour <ref name=":31">Social Development Ireland. Social Development. 2017. <nowiki>https://downsyndrome.ie/social-development-behaviour/</nowiki> (accessed 25 March 2018).</ref>
| |
| These are important skills that need to be addressed. A few suggestions to help parents improve these aspects of a child’s life are listed below:
| |
| * Start from an early age and encourage socialisation
| |
| * Encourage independence in all aspects of life
| |
| * Teach social skills in small steps, with consistent messages
| |
| * Sign their child up for sports teams, other activities they enjoy
| |
| * Encourage parents to talk with teachers and monitor their child's progress
| |
| * Join playgroups with other children with and without DS
| |
| * Provide examples of acceptable social behaviour when watching TV or movies <ref name=":31" />
| |
| | |
| === Transition From Child to Adult Services ===
| |
| Becoming an adult can be confusing and difficult for everyone, especially for people with caring needs or intellectual disabilities (ID). When a person with DS gets older they are transferred from children’s services to adult care. The exact age may change depending on the service or area you are located in. This transition is often accompanied by a change in physiotherapist, services available and a disruption to routine. It is often a stressful time and has historically been an issue for service users. In an attempt to correct this, several pieces of legislation have been set out by the UK government.
| |
| | |
| The Road Ahead Project was commissioned by the Social Care Institute for Excellence (SCIE) in order to explore what information people with DS and their parents might need during the transition <ref>SCIE. The Road Ahead. <nowiki>https://www.scie.org.uk/publications/tra/index.asp</nowiki> .(accessed 30 March 2018).</ref>. The most common pieces of information families wanted to know were:
| |
| # Parental roles within the transition process including their rights and entitlements
| |
| # The local situation – support and resources available
| |
| # The young person’s rights and responsibilities as an adult including information on self-advocacy, empowerment and keeping safe
| |
| # All possible options available
| |
| The Education Act <ref>Her Majesty’s Stationery Office. Education Act and associated Code of Practice. London: HMSO, 1993.</ref> states that at the time of transition, healthcare professionals have several responsibilities;
| |
| * Provision of written advice including details about services likely to be required in the near future once they have left child services
| |
| * Discussion of transfer to adult services with the individual, their family and GP
| |
| * Facilitation of any necessary referrals
| |
| * Attend individual’s annual review meetings from year 9 onwards
| |
| | |
| Despite numerous government legislations and guidance, research strongly says that there continues to be a marked variation in the arrangements available for the transition from child to adult services <ref>Slopper P, Beecham J, Clarke S, Franklin A, Moran N, Cusworth L. Models of multi-agency services for transition to audit services for disabled young people and those with complex health needs: impacts and cost. University of York: Social policy research unit. <nowiki>https://kar.kent.ac.uk/32459/2/transitions%5B1%5D.pdf</nowiki> (accessed 30 March 2018).</ref>. In order to combat this, some further steps have been taken.
| |
| | |
| ==== Collaboration ====
| |
| * Increased collaboration between Child and Adolescent Mental Health Services (CAMHS) and adult intellectual disability services. | |
| | |
| ==== More Training for Staff ====
| |
| * Better education for staff in both adult and child services
| |
| * Improved knowledge of legal changes associated with becoming an adult
| |
| * Expanded awareness regarding available referral options
| |
| | |
| ==== Better Integration Between Services ====
| |
| * Different services are unique in their structures and philosophies – if there was more integration between services and increased awareness of each other’s role, a more uniform and continuous service could be provided <ref>Singh P, Paul M, Ford T, Kramer T, Weaver T, Mclaren S, Hovish K, Islam Z, Belling R, White S. Process, outcome and experience of transition from child to adult mental healthcare: multiperspective study. The British Journal of Psychiatry 2010;197:305-312.</ref>.
| |
| | |
| ==== How Can You Make the Transition Easier? ====
| |
| [[File:Plan ahead.jpg|right|frameless|275x275px|<ref>Blue Hippo Group .Plan Ahead. 2015. [Picture].</ref>]] | |
| While the transition between services relies heavily on geography and physiotherapy services there are a few ways to make this transition easier:
| |
| * Make a plan with the family in advance.
| |
| * Give information on adult services prior to transitioning.
| |
| * Set a date for the transition to occur.
| |
| * Offer to conduct a joint session between new and old services to ease the transition for service providers and the patient and their family.
| |
| * Include the client and their family in the transition decisions <ref>Viner R. Transition from paediatric to adult care. Bridging the gaps or passing the buck. British Medical Journal 1999;81:3. www.adc.bmj.com/content/81/3/271 (accessed 14 March 2018).</ref>.
| |
|
| |
|
| ==== Remember! ====
| | As many treatments often require on-going maintenance, the team should encourage family members to support and implement home treatment plans in an attempt to encourage self-management.<ref>Middleton J, Kitchen S. Factors affecting the involvement of day centre staff in the delivery of physiotherapy to adults with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities 2008:21:227-235. www.onlinelibrary.wiley.com/doi/10.1111/j.1468-3148.2007.00396.x/epdf (accessed 11 March 2018).</ref> By fostering strong communication among the team members and families, the multidisciplinary rehabilitation team can make a lasting impact on the lives of individuals with DS, helping them achieve their full potential and lead more independent lives. |
| Down syndrome can be challenging not only for the individual, but also for the family. It is common for family members of persons with DS to:[[File:Self care.jpg|right|frameless|228x228px|Equality Institute. Self Care. 2014. [Picture].]]
| |
| * Feel increased levels of stress
| |
| * Experience lower levels of well being
| |
| * Exhibit mild depressive symptoms
| |
| * Have decreased confidence in raising their child
| |
| * Think about their child’s social acceptability
| |
| * Worry about their marriage or their other children <ref>Cuskelly M, Cram P, Ruper M. Families of children with down syndrome: what we know and what we need to know. Down Syndrome Research and Practice 2008. <nowiki>https://library.down-syndrome.org/en-gb/research-practice/online/2008/families-down-syndrome-what-need/</nowiki> (accessed 25 March 2018).</ref>
| |
| Much research has been done on family dynamics and though results are often unclear, recent investigation is revealing that the increased levels of stress and decreased levels of well-being are evident in parents with a child who has DS for a variety of reasons. Demanding parenting roles, concerns over their family member’s social acceptability and decreased confidence in parenting skills are just a few contributors to high-stress levels in parents of persons with DS <ref>Most D, Fidler D, Booth C, Kelly J. Stress trajectories in mothers of young children with Down syndrome. Journal of Intellectual Disability Research 2006;50:501-514. <nowiki>https://www.ncbi.nlm.nih.gov/pubmed/16774635</nowiki> (accessed 24 March 2018). </ref>.
| |
|
| |
|
| For this reason, it is important that you remind family members to take time to focus on themselves. Taking time for themselves may improve both their personal mental health and their families’ overall well being. Though these small things may seem insignificant they can have a dramatic effect on how they feel and the cohesiveness of their family unit <ref>Cram P, Warfield M, Shonkoff J, Krauss M. Children with disabilities: A longitudinal study of child development and parent well-being. Monographs of the Society for Research in Child Development 2001;66:266. <nowiki>https://www.ncbi.nlm.nih.gov/pubmed/11677873</nowiki> (accessed 26 March 2018). </ref>.
| | == Resources == |
| | The following “Ted Talk” presented by Karen Gaffney, a person with Down Syndrome, explores numerous contemporary thoughts surrounding DS and challenges society's preconceptions of people with DS.{{#ev: youtube| HwxjoBQdn0s}} |
| == References == | | == References == |
|
| |
|
| Line 453: |
Line 106: |
| [[Category:Queen_Margaret_University_Project]] | | [[Category:Queen_Margaret_University_Project]] |
| [[Category:Paediatrics]] | | [[Category:Paediatrics]] |
| | [[Category:Down Syndrome - Trisomy 21]] |
| [[Category:Paediatrics - Conditions]] | | [[Category:Paediatrics - Conditions]] |
| [[Category:Non Communicable Diseases]] | | [[Category:Non Communicable Diseases]] |
| [[Category:Conditions]] | | [[Category:Conditions]] |
| [[Category:Genetic Disorders]] | | [[Category:Genetic Disorders]] |
| | [[Category:Course Pages]] |

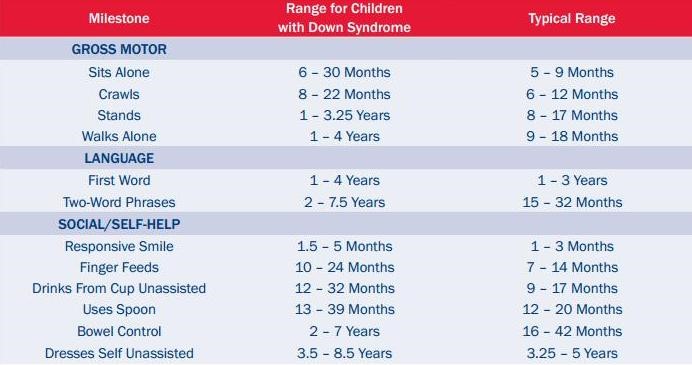
![[20]](/images/c/c6/Elizabeth_Stick_Men.jpg)






