Developmental Disabilities in Early and Middle Childhood: Difference between revisions
m (Protected "The Social, Cognitive and Emotional Development of Children - Developmental Disabilities" ([Edit=Allow only autoconfirmed users] (indefinite) [Move=Allow only autoconfirmed users] (indefinite))) |
No edit summary |
||
| Line 4: | Line 4: | ||
<div class="noeditbox">This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}})</div> | <div class="noeditbox">This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}})</div> | ||
Introduction | == Introduction == | ||
"Developmental disabilities are a diverse group of severe chronic conditions that are due to mental and/or physical impairments. People with developmental disabilities have problems with major life activities such as language, mobility, learning, self-help, and independent living."<ref>Xcitesteps. What are developmental disabilities? Available from: http://www.xcitesteps.com/faqs/developmental-disabilities/ (accessed 9 August 2021).</ref> | |||
Developmental disabilities | Developmental disabilities (DDs) includes conditions such as:<ref name=":0">Prowse T. The Social, Cognitive and Emotional Development of Children - Developmental Disabilities Course. Physioplus, 2021.</ref> | ||
* Attention deficit hyperactivity disorder (ADHD) | |||
* Autism | |||
* Intellectual disability | |||
* Learning difficulties (including ADHD, developmental coordination disorder (DCD) / dyspraxia, auditory processing disorder) | |||
* Blindness | |||
* Cerebral palsy | |||
* Moderate to profound hearing loss | |||
* Seizures | |||
* Stuttering / stammering | |||
* Other developmental delay | |||
The prevalence of DDs is increasing. From 1997 to 2008 autism prevalence increased by 289.5 percent and ADHD increased by 33 percent.<ref>Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M et al. Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatrics. 2011;127(6):1034-42. </ref> The 2009-2017 National Health Interview Survey showed a 9.5 percent increase in the prevalence of DDs in children aged 3 to 17 years.<ref>Zablotsky B, Black LI, Maenner MJ, Schieve LA, Danielson ML, Bitsko RH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7076808/ Prevalence and trends of developmental disabilities among children in the United States: 2009-2017]. ''Pediatrics.'' 2019;144(4):e20190811.</ref> | |||
== Movement Difficulties == | |||
=== Hypermobility === | |||
==== Muscle Tone ==== | |||
Muscle tone is defined as: “the tension in the relaxed muscle” - GANGULY i.e. | |||
the amount of tension or resistance to stretch in a muscle. WEB | |||
==== Hypotonia ==== | |||
Hypotonia is defined as: “poor muscle tone resulting in floppiness. It is abnormally decreased resistance encountered with passive movement of the joint.” MADHOK | |||
There are different causes of hypotonia: WEB | |||
* Lower motor neuron disease (neurological, metabolic and genetic causes) | |||
* Infections (meningitis, polio) | |||
* Genetic (Down’s syndrome, Prader-Willi, Tay-Sachs, spinal muscular atrophy, Charcot-Marie-Tooth syndrome, Marfan syndrome and Ehlers-Danlos syndrome) | |||
* Metabolic (rickets) | |||
* Congenital hypothyroidism | |||
* Genetic acquired (muscular dystrophy) | |||
* Benign congenital hypotonia (BCH) | |||
** NB: BCH is a symptom, rather than a diagnosis. Diagnosis is made in the absence of other diagnoses (such as joint hypermobility, aspergers, autism, DCD). | |||
* Low connective tissue tone - this is considered better terminology to describe hypermobility or increased laxity in connective tissue | |||
* Joint hypermobility | |||
** This term is used when only the connective tissue in the joints is affected | |||
* Benign Joint Hypermobility Syndrome (BJHS) | |||
==== Benign Joint Hypermobility Syndrome ==== | |||
[[Benign Joint Hypermobility Syndrome|BJHS]] is a hereditary condition<ref>Neki NS, Chhabra A. [https://www.jmgims.co.in/article.asp?issn=0971-9903;year=2016;volume=21;issue=1;spage=12;epage=18;aulast=Neki Benign joint hypermobility syndrome]. Journal of Mahatma Gandhi Institute of Medical Sciences. 2016; 21(1):12-8.</ref> that causes musculoskeletal symptoms in hypermobile patients, without other rheumatological features being present. It appears to be caused by an abnormality in collagen or the ratio of collagen subtypes.<ref>Simpson MMR. Benign Joint Hypermobility Syndrome: Evaluation, Diagnosis, and Management. J Am Osteopath Assoc. 2006;106(9): 531–536.</ref> | |||
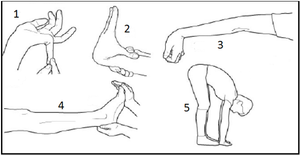
[[File:Beighton Score.png|thumb|Figure 1. Beighton score.]] | |||
Diagnosis is made based on a medical examination and use of the [[Beighton score]] (see Figure 1) | |||
Children with BJHS are susceptible to joint injury or dislocation, reduced stability, and a decreased ability to build muscle strength. They may tire easily, complain of pain or digestive issues, but symptoms are variable. They tend to be exacerbated during growth spurts, adolescence and hormone changes.<ref name=":0" /> | |||
==== The Good News ==== | |||
* Strengthening is beneficial<ref>Palmer S, Bailey S, Barker L, Barney L, Elliott A. The effectiveness of therapeutic exercise for joint hypermobility syndrome: a systematic review. Physiotherapy. 2014; 100(3): 220-7.</ref> | |||
* Swimming, pilates, climbing, horse riding can help (i.e. non-impact activities):<ref name=":0" /> | |||
** If children engage in high impact sports, they may require rest days (particularly if they are complaining of night pain after activity) | |||
* Specific movement programmes such as Physifun are beneficial<ref name=":0" /> | |||
NB: If BJHS children participate in ballet, gym or dancing, it is important that they avoid “locking out” their joints. Instead, teach them to have “soft knees”. Also watch for lordotic postures and tight hamstrings.<ref name=":0" /> | |||
== References == | |||
[[Category:Physioplus Content]] | |||
[[Category:Course Pages]] | |||
[[Category:Paediatrics]] | |||
Revision as of 11:23, 9 August 2021
Top Contributors - Jess Bell, Kim Jackson, Wanda van Niekerk, Naomi O'Reilly, Tarina van der Stockt, Rucha Gadgil and Cindy John-Chu
Introduction[edit | edit source]
"Developmental disabilities are a diverse group of severe chronic conditions that are due to mental and/or physical impairments. People with developmental disabilities have problems with major life activities such as language, mobility, learning, self-help, and independent living."[1]
Developmental disabilities (DDs) includes conditions such as:[2]
- Attention deficit hyperactivity disorder (ADHD)
- Autism
- Intellectual disability
- Learning difficulties (including ADHD, developmental coordination disorder (DCD) / dyspraxia, auditory processing disorder)
- Blindness
- Cerebral palsy
- Moderate to profound hearing loss
- Seizures
- Stuttering / stammering
- Other developmental delay
The prevalence of DDs is increasing. From 1997 to 2008 autism prevalence increased by 289.5 percent and ADHD increased by 33 percent.[3] The 2009-2017 National Health Interview Survey showed a 9.5 percent increase in the prevalence of DDs in children aged 3 to 17 years.[4]
Movement Difficulties[edit | edit source]
Hypermobility[edit | edit source]
Muscle Tone[edit | edit source]
Muscle tone is defined as: “the tension in the relaxed muscle” - GANGULY i.e.
the amount of tension or resistance to stretch in a muscle. WEB
Hypotonia[edit | edit source]
Hypotonia is defined as: “poor muscle tone resulting in floppiness. It is abnormally decreased resistance encountered with passive movement of the joint.” MADHOK
There are different causes of hypotonia: WEB
- Lower motor neuron disease (neurological, metabolic and genetic causes)
- Infections (meningitis, polio)
- Genetic (Down’s syndrome, Prader-Willi, Tay-Sachs, spinal muscular atrophy, Charcot-Marie-Tooth syndrome, Marfan syndrome and Ehlers-Danlos syndrome)
- Metabolic (rickets)
- Congenital hypothyroidism
- Genetic acquired (muscular dystrophy)
- Benign congenital hypotonia (BCH)
- NB: BCH is a symptom, rather than a diagnosis. Diagnosis is made in the absence of other diagnoses (such as joint hypermobility, aspergers, autism, DCD).
- Low connective tissue tone - this is considered better terminology to describe hypermobility or increased laxity in connective tissue
- Joint hypermobility
- This term is used when only the connective tissue in the joints is affected
- Benign Joint Hypermobility Syndrome (BJHS)
Benign Joint Hypermobility Syndrome[edit | edit source]
BJHS is a hereditary condition[5] that causes musculoskeletal symptoms in hypermobile patients, without other rheumatological features being present. It appears to be caused by an abnormality in collagen or the ratio of collagen subtypes.[6]
Diagnosis is made based on a medical examination and use of the Beighton score (see Figure 1)
Children with BJHS are susceptible to joint injury or dislocation, reduced stability, and a decreased ability to build muscle strength. They may tire easily, complain of pain or digestive issues, but symptoms are variable. They tend to be exacerbated during growth spurts, adolescence and hormone changes.[2]
The Good News[edit | edit source]
- Strengthening is beneficial[7]
- Swimming, pilates, climbing, horse riding can help (i.e. non-impact activities):[2]
- If children engage in high impact sports, they may require rest days (particularly if they are complaining of night pain after activity)
- Specific movement programmes such as Physifun are beneficial[2]
NB: If BJHS children participate in ballet, gym or dancing, it is important that they avoid “locking out” their joints. Instead, teach them to have “soft knees”. Also watch for lordotic postures and tight hamstrings.[2]
References[edit | edit source]
- ↑ Xcitesteps. What are developmental disabilities? Available from: http://www.xcitesteps.com/faqs/developmental-disabilities/ (accessed 9 August 2021).
- ↑ 2.0 2.1 2.2 2.3 2.4 Prowse T. The Social, Cognitive and Emotional Development of Children - Developmental Disabilities Course. Physioplus, 2021.
- ↑ Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M et al. Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatrics. 2011;127(6):1034-42.
- ↑ Zablotsky B, Black LI, Maenner MJ, Schieve LA, Danielson ML, Bitsko RH. Prevalence and trends of developmental disabilities among children in the United States: 2009-2017. Pediatrics. 2019;144(4):e20190811.
- ↑ Neki NS, Chhabra A. Benign joint hypermobility syndrome. Journal of Mahatma Gandhi Institute of Medical Sciences. 2016; 21(1):12-8.
- ↑ Simpson MMR. Benign Joint Hypermobility Syndrome: Evaluation, Diagnosis, and Management. J Am Osteopath Assoc. 2006;106(9): 531–536.
- ↑ Palmer S, Bailey S, Barker L, Barney L, Elliott A. The effectiveness of therapeutic exercise for joint hypermobility syndrome: a systematic review. Physiotherapy. 2014; 100(3): 220-7.