Deep Vein Thrombosis
Original Editor - Jennifer Self
Top Contributors - Admin, Karen Wilson, Kim Jackson, Laura Ritchie, Scott Buxton, Shaimaa Eldib, Jennifer Self, Lucinda hampton, Ayesha Arabi, WikiSysop, Adam Vallely Farrell and Claire Knott
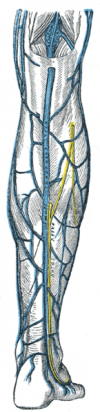
Clinically Relevant Anatomy[edit | edit source]
Deep Vein Thrombosis (DVT) is when one or more blood clots form in a deep vein of the body. The most common site for DVT is the lower limbs.[1] Proximal DVTs of the lower extremity (LE) involve the popliteal and/or thigh veins (femoral vein, external iliac vein, deep vein of the thigh), while distal DVTs encompass those that develop in the calf.
DVTs in the upper extremity (UE) are less common (4-10% of all cases).[2] The deep veins of the upper extremity include the jugular, brachiocephalic, subclavian, and axillary veins proximally and the brachial, ulnar, and radial veins distally. In the upper extremity, the subclavian, jugular and axillary veins are the primary vessels in which DVTs form.[2][3]
Pathological Process[edit | edit source]
Thrombi develop as a result of hypercoagulation and stasis around venous valve sinuses. The majority of deep vein thrombi start in the calf.[4] These clots are firm and are mostly made up of fibrin and red blood cells[1] (see the image of a DVT here). On autopsy, the majority are attached to venous walls.[1]
Within 72 hours, an estimated 50% of intra-operative calf DVTs resolve on their own.[4] About 1 in 6 of these extend into the proximal veins of the leg,[4] causing venous obstruction and damage to affected valves. A subset of proximal DVTs become mobile and progress to pulmonary embolism, a potentially fatal condition. Progression to pulmonary embolism is more common in LE than UE DVTs.[3]
The following video provides a visual representation of DVT pathology:
Risk Factors[edit | edit source]
Various risk factors play into the formation of DVTs. In adults, blood clotting disorders are associated with spontaneous formation.[1] Several other clinical factors augment patient risk as well:[1]
| Clinical Condition | Medical Interventions | Environment |
|---|---|---|
|
|
|
[*VTE= venous thromboembolism]
The UE has its own set of additional risk factors:[2][3]
- Intravenous catheters
- Pacemaker cables
- Anatomical anomalies (ex. shoulder girdle syndrome, clavicular fractures, Paget–von Schroetter syndrome)
Risk factors more prominent in children include sickle cell disease, severe infection, antiphospholipid syndromes and trauma.[5]
Clinical Presentation[edit | edit source]
The clinical presentation of individuals with DVT is inconsistent, as many patients are asymptomatic. Those with symptoms may demonstrate the following features in the affected extremity:[1]
- Discoloration
- Pain/discomfort
- Warmth
- Swelling
- Tenderness
Clinical Prediction Rule (CDR): Well's Criteria[edit | edit source]
Well's Criteria is the most commonly used tool to screen for DVT risk:[1]
| Clinical Variable | Score |
|---|---|
| Active cancer (treatment ongoing or within previous 6 months, or palliative) | +1 |
| Paralysis, paresis, or recent plaster immobilization of the lower extremities | +1 |
| Recently bedridden for > 3 days or major surgery within 4 weeks | +1 |
| Localized tenderness along the distribution of the deep venous system (Tenderness along the deep venous system is assessed by firm palpation in the center of the posterior calf, the popliteal space, and along the area of the femoral vein in the anterior thigh and groin) | +1 |
| Entire lower extremity swelling | +1 |
| Calf swelling > 3 cm when compared with the asymptomatic lower extremity (measured 10cm below the tibial tuberosity) | +1 |
| Pitting edema confined to the symptomatic lower extremity | +1 |
| Collateral superficial veins (non-varicose) | +1 |
| Alternative diagnosis as likely or greater than that of proximal DVT (More common alternative diagnoses include cellulitis, calf strain, Baker Cyst, or postoperative swelling) | -2 |
In the original scale, the total score for all items is tallied and the probability of the patients having a DVT are as follows: 0= low probability, 1-2 points= moderate probability,and ≥ 3 points= high probability.[6] The updated simplifies the scoring process into two categories: ≤ 2 points= DVT unlikely, ≥ 2 points= DVT likely.[7]
Well's Criteria is a valid tool for assessing DVT risk in outpatient[8][9] and trauma[10] patients. It is less useful for stratifying risk in cancer patients[9] and hospitalized patients as a whole.[11] It cannot be used to screen patients for upper extremity DVT.[2]
Clinical Tests/Examination[edit | edit source]
The clinical diagnosis of DVT is unreliable. However, in combination with valid screening tools, clinical examination can justify the need for diagnostic testing.
Observation and Palpation[edit | edit source]
Clinical observation and palpation should focus on identifying the signs and symptoms described in the "Clinical Presentation" section of this article.
Homan's Sign[edit | edit source]
Homan's Sign has been used as an indicator for lower extremity DVT since the 1940s.[12] The test is performed by forcefully dorsiflexing the ankle while the slightly knee flexed. Pain and tenderness in the calf is said to be indicative of lower extremity DVT. Despite its historical use, Homan's sign has no diagnostic value in the identification of LE DVT.[12]
Diagnostic Testing[edit | edit source]
Diagnostic testing is the only definitive way to diagnose DVT.[1]
D-Dimer Testing[edit | edit source]
A simple blood test of fibrin degradation. D-dimer levels in the blood are increased by any condition that produces fibrin; this testing has been found to be the most useful blood marker of fibrinolysis. The negative likelihood ratio is higher than 99%. This test is best used on outpatients with a low probability of proximal DVT, based on the use of the CDR by Wells & colleagues.[13]
Venous Ultrasound[edit | edit source]
Venous ultrasound is considered to be the first-choice diagnostic test for patients with symptomatic DVT in the moderate to high probability groups.[DVT clinical review] The test is a safe, non-invasive and inexpensive. Depending on availability, patient characteristics and the location of the suspected DVT, compression ultrasound, duplex ultrasound or color Doppler imaging may be used.[DVT clinical review] The sensitivity and specificity of compression ultrasonography averages 95% for detection of proximal DVT.[13]
Venography[edit | edit source]
This is considered the gold standard test for DVT.[DVT clinical review] The test is rarely used due to its invasive nature and availability of accurate, non-invasive options (D-dimer and venous ultrasound). The procedure involves an x-ray of the veins (venogram) taken after a special dye is injected into the bone marrow or veins.[13]
Management / Interventions[edit | edit source]
Primary Prevention[edit | edit source]
A combination of mechanical and pharmacological measures can be used to prevent DVT. Mechanical prophylaxis involves the use of graduated compression stockings (GCS), intermittent pneumatic compression (IPC) and venous foot pumps to improve blood flow in the deep veins of the leg. Common agents for pharmacological prophylaxis include Warfarin, subcutaneous unfractionated heparin (UFH) and low-molecular-weight heparins (LMWH).[UE DVT] DVT prevention is most effective when both methods are used simultaneously.[DVT clinical review] In medical and surgical patients ambulation and exercises involving ankle dorsiflexion are encouraged to further minimize venous stasis. [DVT clinical review]
Medical Treatment[edit | edit source]
Anticoagulation[edit | edit source]
Anticoagulation is the usual treatment for DVT. Patients are generally initiated on a brief course (i.e., less than a week) of heparin treatment.[14] If heparin is contraindicated, fondaparinux (FDX) or direct or anticoagulants (DOAC) [ex. Xarelto, dabigatran, apixaban] may be used.[1] Acute DVT treatment is followed by a maintenance course (typically 3-6 months) of warfarin or other Vitamin K inhibitors.[1][14] Variations in treatment may exist for patients with delayed removal of an intravenous catheter or an ongoing tumor disease in the case of UE DVT.[2]
Thrombolysis[edit | edit source]
Although rarely indicated, thrombolytic therapy is used to treat an extensive clot.[1] A meta-analysis of randomized controlled trials by the Cochrane Collaboration[15] shows improved outcomes with thrombolysis, although there may be an increase in serious bleeding complications.
Inferior Vena Cava (IVC) Filter[edit | edit source]
IVC filters may prevent pulmonary embolisation and is an option for patients with an absolute contraindication to anticoagulant treatment.[16] Most newer filters can be removed after placement.[1] Complications of this intervention include filter erosion, filter migration and obstruction of the inferior vena cava.[1]
Secondary Prevention[edit | edit source]
Early Mobilization[edit | edit source]
In conjunction with anti-coagulation, bed rest is commonly prescribed in the immediate days following the diagnosis of LE DVT. This practice is applied with the intent of preventing clot dislodgement and the incidence of PE. The theoretical basis behind this protocol has not been supported by the literature.[17][18] Early ambulation is associated with fewer incidences of new PE and decreased mortality.[18] and should be a priority once a patient is safe to do so (see the next secion on "Implications for Physical Therapy Practice" for guidelines on safe mobilization following known DVT).
Graduated Compression Stockings[edit | edit source]
The application of graduated compression stockings is recommended "beginning within 1 month of diagnosis of proximal DVT and continuing for a minimum of 1 year after diagnosis" to prevent DVT recurrence.[19]
Implications for Physical Therapy Practice[edit | edit source]
Physical therapists work with patients at risk for and with diagnosed DVT across the continuum of care. For this reason, the American Physical Therapy Association (APTA) has developed clinical practice guidelines (CPG)[20] to facilitate clinical decision making in the prevention and management of LE DVT in adults. The following table outlines the 5 responsibilities of physical therapists (PTs) with actionable recommendations:
| PT Responsibilities | Actionable Recommendations | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| (1) Prevention of VTE |
| ||||||||
| (2) Screening for LE DVT |
| ||||||||
| (3) Making prudent decisions regarding safe mobility in conjunction with the health care team |
| ||||||||
| (4) Prevention of long-term consequences of LE DVT |
| ||||||||
| (5) Patient education & shared decision making |
|
*NOTE: Execution of the above recommendations should be done in line with institution-specific policies. Hillegass et al[20] offer a decision making algorithm that may be helpful in the absence of or as a reference point for updating health care system protocols)
Differential Diagnosis[edit | edit source]
Below is a non-exhaustive list for the differential diagnosis of calf pain in patients with suspected LE DVT:[21][12]
- Pyomyositis
- Fibula shaft fracture
- Cellulitis
- Ruptured Baker's cyst
- Neurogenic leg pain
- Hematoma
- Rupture of Achilles Tendon
- Soleus muscle strain
- Acute posterior compartment syndrome
- Calf muscle cramps
Resources[edit | edit source]
Presentations[edit | edit source]
 |
Differential Diagnosis and VTE
This presentation, created by Carleen Jogodka as part of the Evidence In Motion OMPT Fellowship, discusses differential diagnosis for venous thromboembolism. |
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1lGTpA7S74wiuMUQ_tI6X1P9s02KQ2A3QIj_uTEdGv29exlk3C: Error parsing XML for RSS
Read 4 Credit[edit | edit source]
|
Would you like to earn certification to prove your knowledge on this topic? All you need to do is pass the quiz relating to this page in the Physiopedia member area.
|
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Kesieme E, Kesieme C, Jebbin N, Irekpita E, Dongo A. Deep vein thrombosis: a clinical review. J Blood Med 2011; 2:59–69.
- ↑ 2.0 2.1 2.2 2.3 2.4 Heil J, Miesbach W, Vogl T, Bechstein WO, Reinisch A. Deep vein thrombosis of the upper extremity: A systematic review. Dtsch Arztebl Int 2017; 114(14): 244–249
- ↑ 3.0 3.1 3.2 Joffe H, Kucher N, Tapson V, Goldhaber S. Upper-extremity deep vein thrombosis: a prospective registry of 593 patients. Circulation 2004; 110: 1605-1611
- ↑ 4.0 4.1 4.2 Kearon C. Natural history of venous thromboembolism. Seminars in Vascular Medicine 2001; 01(1): 027-038
- ↑ Gertziafas GT. Risk factors for venous embolism in children. Int Angiol 2004;2 3(3):195–205
- ↑ Wells PS, Hirsh J, Anderson DR, Lensing AW, Foster G, Kearon C, Weitz J, D'Ovidio R, Cogo A, Prandoni P. Accuracy of clinical assessment of deep-vein thrombosis. Lancet 1995; 345(8961):1326-1330
- ↑ Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, Kovacs G, Mitchell M, Lewandowski B, Kovacs MJ. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med 2003; 349:1227–1235
- ↑ Wells PS, Anderson DR, Bormanis J, Guy F, Mitchell M, Gray L, Clement C, Robinson KS, Lewandowski B. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet 1997; 350(9094):1795-1798
- ↑ 9.0 9.1 Geersing GJ, Zuithoff NPA, Kearon C, Anderson DR, Cate-Hoek T, Elf JL, Bates SM, Hoes AW, Kraaijenhagen RA, Oudega R, Schutgens RE, Stevens SM, Woller SC, Wells PS, Moons KG. Exclusion of deep vein thrombosis using the Wells rule in clinically important subgroups: individual patient data meta-analysis. BMJ 2014; 348:g1340
- ↑ Modi S, Deisler R, Gozel K, Reicks P, Irwin E, Brunsvold M, Banton K, Beilman GJ. Wells criteria for DVT is a reliable clinical tool to assess the risk of deep venous thrombosis in trauma patients. World J Emerg Surg. 2016; 11: 24
- ↑ Silveira PC, Ip IK, Goldhaber SZ, Piazza G, Benson CB, Khorasani R. Performance of Wells Score for Deep Vein Thrombosis in the Inpatient Setting. JAMA Intern Med 2015; 175(7):1112-7
- ↑ 12.0 12.1 12.2 Urbano F. Homans' Sign in the Diagnosis of Deep Venous Thrombosis. Hospital Physician 2001. 22-24
- ↑ 13.0 13.1 13.2 Riddle DL, Wells PS. Diagnosis of Lower-Extremity Deep Vein Thrombosis in Outpatients. Physical Therapy. 84 (8); 729-735.
- ↑ 14.0 14.1 Snow V, Qaseem A, Barry P, et al. (2007). "Management of venous thromboembolism: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians". Ann. Intern. Med. 146 (3): 204–10.
- ↑ Watson L, Armon M (2004). "Thrombolysis for acute deep vein thrombosis". Cochrane Database Syst Rev: CD002783
- ↑ Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, Laporte S, Faivre R, Charbonnier B, Barral F, Huet Y, Simonneau G (1998). "A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group". N Engl J Med 338 (7): 409–15.
- ↑ Aissaoui N, Martins E, Mouly S, Wever S, Meune C. A meta-analysis of bed rest versus early ambulation in the management of pulmonary embolism, deep vein thrombosis, or both. Int J Cardiol 2009;137:37–41
- ↑ 18.0 18.1 Kahn SR, Shrier I, Kearon C. Physical activity in patients with deep venous thrombosis: a systematic review. Thromb Res 2008; 122:763–773
- ↑ Snow V, Qaseem A, Barry P, et al. (2007). "Management of venous thromboembolism: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians". Ann. Intern. Med. 146 (3): 204–10.
- ↑ 20.0 20.1 Hillegass E, Puthoff M, Frese EM, Thigpen M, Sobush DC, Auten B. Role of Physical Therapists in the Management of Individuals at Risk for or Diagnosed With Venous Thromboembolism: Evidence-Based Clinical Practice Guideline. Phys Ther 2016; 96(2):143-66
- ↑ Dutton. Orthopaedic Examination, Evaluation, and Intervention. McGraw Hill; 2004. pg 261, 1338, 1367.