Costochondritis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<br>1 Search Strategy<br>2 Definition/Description<br>3 Clinically Relevant Anatomy<br>4 Epidemiology /Etiology<br>5 Characteristics/Clinical Presentation<br>6 Differential Diagnosis<br>7 Diagnostic Procedures<br>8 Outcome Measures<br>9 Examination<br>10 Medical Management<br>11 Physical Therapy Management<br>12 Key Research<br>13 Resources<br>14 Clinical Bottom Line<br>15 Recent Related Research (from Pubmed)<br>16 References | <br>1 Search Strategy<br>2 Definition/Description<br>3 Clinically Relevant Anatomy<br>4 Epidemiology /Etiology<br>5 Characteristics/Clinical Presentation<br>6 Differential Diagnosis<br>7 Diagnostic Procedures<br>8 Outcome Measures<br>9 Examination<br>10 Medical Management | ||
<div><br>11 Physical Therapy Management<br>12 Key Research<br>13 Resources<br>14 Clinical Bottom Line<br>15 Recent Related Research (from Pubmed)<br>16 References </div> | |||
<br> | <br> | ||
| Line 17: | Line 17: | ||
<br> | <br> | ||
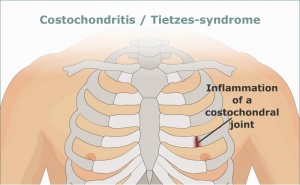
<u>• 2 Definition/Description</u><br>Costochondritis is a painfull chronical inflammation of the cartilago of one or more costae at<br>the transition between sternum and costae.[1][2][3] Only when a swelling occurs underneath sternum and/or a reddening of the skin at the painfull spot, it's called Tietze's syndrome[4][5][6][7]. This disease causes severe pain when coughing and deep breathing. The Tietze's syndrome is not life-threatening or contagious but it is a fastidious and painfull disease.[4][3] Costochondritis[6] and the Tietze's syndrome are often confused but in fact they are two different diseases. [8]<br> <br>Costochondritis usually affects the third, fourth and fifth costochondral joint and occurs more often in women. Whereas Tietze’s syndrome most commonly affects one joint, in particularly the second or third costal cartilage and both sexes are affected equally [9]. Both diseases can start either acute or progressively at any age | <u>• 2 Definition/Description</u><br>Costochondritis is a painfull chronical inflammation of the cartilago of one or more costae at<br>the transition between sternum and costae.[1][2][3] Only when a swelling occurs underneath sternum and/or a reddening of the skin at the painfull spot, it's called Tietze's syndrome[4][5][6][7]. This disease causes severe pain when coughing and deep breathing. The Tietze's syndrome is not life-threatening or contagious but it is a fastidious and painfull disease.[4][3] Costochondritis[6] and the Tietze's syndrome are often confused but in fact they are two different diseases. [8]<br> <br>Costochondritis usually affects the third, fourth and fifth costochondral joint and occurs more often in women. Whereas Tietze’s syndrome most commonly affects one joint, in particularly the second or third costal cartilage and both sexes are affected equally [9]. Both diseases can start either acute or progressively at any age. | ||
[[Image:Costochrondritis.jpg|border|right|300x200px]]<br><u>• 3 Clinically Relevant Anatomy</u> | |||
The diagnosis of costochondritis relies on patient history and physical examination findings; therefore, understanding of the chest anatomy is important. Ribs consist of bone and cartilage, with cartilage serving as an elastic bridge between the bony portion of the rib and the sternum. Anteriorly, the costal cartilage of the first rib connects with the manubrium via a rigid fusion of bone and cartilage. The next seven pairs of ribs articulate with the sternum via cartilage at synovial-lined joints. Ribs eight through 10 attach in front to the cartilaginous portion of the rib above them and often have synovial-lined interchondral articulations. The lowest two ribs do not articulate with any structure anteriorly.2,1The ribs move with respiration and with truncal motion or movement of the upper extremities. The innervation of the thoracic wall is supplied mostly by the intercostal nerves. Impingement of these nerves by movement of the overlying rib or cartilage can cause pain.2 The shoulder girdle muscles develop in the lower cervical region and carry this innervation with them as they move to attach to the chest wall. Thus, cervical or shoulder problems may refer pain to the chest wall. | The diagnosis of costochondritis relies on patient history and physical examination findings; therefore, understanding of the chest anatomy is important. Ribs consist of bone and cartilage, with cartilage serving as an elastic bridge between the bony portion of the rib and the sternum. Anteriorly, the costal cartilage of the first rib connects with the manubrium via a rigid fusion of bone and cartilage. The next seven pairs of ribs articulate with the sternum via cartilage at synovial-lined joints. Ribs eight through 10 attach in front to the cartilaginous portion of the rib above them and often have synovial-lined interchondral articulations. The lowest two ribs do not articulate with any structure anteriorly.2,1The ribs move with respiration and with truncal motion or movement of the upper extremities. The innervation of the thoracic wall is supplied mostly by the intercostal nerves. Impingement of these nerves by movement of the overlying rib or cartilage can cause pain.2 The shoulder girdle muscles develop in the lower cervical region and carry this innervation with them as they move to attach to the chest wall. Thus, cervical or shoulder problems may refer pain to the chest wall. | ||
<br> | <br> | ||
Revision as of 19:40, 1 September 2015
1 Search Strategy
2 Definition/Description
3 Clinically Relevant Anatomy
4 Epidemiology /Etiology
5 Characteristics/Clinical Presentation
6 Differential Diagnosis
7 Diagnostic Procedures
8 Outcome Measures
9 Examination
10 Medical Management
11 Physical Therapy Management
12 Key Research
13 Resources
14 Clinical Bottom Line
15 Recent Related Research (from Pubmed)
16 References
• 1 Search Strategy
Pubmed
Web of knowledge
Search criteria : costochondritis/treatment/outcome/tietze/
• 2 Definition/Description
Costochondritis is a painfull chronical inflammation of the cartilago of one or more costae at
the transition between sternum and costae.[1][2][3] Only when a swelling occurs underneath sternum and/or a reddening of the skin at the painfull spot, it's called Tietze's syndrome[4][5][6][7]. This disease causes severe pain when coughing and deep breathing. The Tietze's syndrome is not life-threatening or contagious but it is a fastidious and painfull disease.[4][3] Costochondritis[6] and the Tietze's syndrome are often confused but in fact they are two different diseases. [8]
Costochondritis usually affects the third, fourth and fifth costochondral joint and occurs more often in women. Whereas Tietze’s syndrome most commonly affects one joint, in particularly the second or third costal cartilage and both sexes are affected equally [9]. Both diseases can start either acute or progressively at any age.
• 3 Clinically Relevant Anatomy
The diagnosis of costochondritis relies on patient history and physical examination findings; therefore, understanding of the chest anatomy is important. Ribs consist of bone and cartilage, with cartilage serving as an elastic bridge between the bony portion of the rib and the sternum. Anteriorly, the costal cartilage of the first rib connects with the manubrium via a rigid fusion of bone and cartilage. The next seven pairs of ribs articulate with the sternum via cartilage at synovial-lined joints. Ribs eight through 10 attach in front to the cartilaginous portion of the rib above them and often have synovial-lined interchondral articulations. The lowest two ribs do not articulate with any structure anteriorly.2,1The ribs move with respiration and with truncal motion or movement of the upper extremities. The innervation of the thoracic wall is supplied mostly by the intercostal nerves. Impingement of these nerves by movement of the overlying rib or cartilage can cause pain.2 The shoulder girdle muscles develop in the lower cervical region and carry this innervation with them as they move to attach to the chest wall. Thus, cervical or shoulder problems may refer pain to the chest wall.
• 4 Epidemiology /Etiology
Costochondritis can affect children as well as adults. A study of chest pain in an outpatient adolescent clinic found that 31 percent of adolescents had musculoskeletal causes, with costochondritis accounting for 14 percent of adolescent patients with chest pain.5 In this series, no definite cause of chest pain was found in 39 percent of cases.5 In a prospective series of children three to 15 years of age presenting to an emergency department or cardiac clinic with chest pain, chest wall pain was the most common diagnosis, with respiratory and psychogenic conditions the next most common diagnoses.8
Costochondritis is a common diagnosis in adults with acute chest pain. It is present in 13 to 36 percent of these patients, depending on the study and the patient setting.4,7,24 In a prospective study of adult patients presenting to an emergency department with chest pain, 30 percent had costochondritis. A prospective study of episodes of care for chest pain in a primary care office network found musculoskeletal causes in 20 percent of episodes of care, with costochondritis responsible for 13 percent.9 These data are similar to a study of patients with noncardiac chest pain that found reproducible chest wall tenderness (although not specifically defined as costochondritis) in 16 percent of patients.4 A European study found a higher prevalence of musculoskeletal diagnoses in patients with chest pain presenting in primary care settings compared with hospital settings (20 versus 6 percent, respectively).10
• 5 Characteristics/Clinical Presentation
The cartilage connects sternum with costae and clavicula, and makes the movement of the thorax possible while breathing. [1][3] The inflammation of the cartilage of one or more costae causes a red, warm swelling of the cartilage. This will be both visible and palpable.[3][7]There is pain with a varying intensity in the chest wall and this pain aggravated by movements of the torso, deep breathing, coughing and exertion. [7][8][4][1] Pain occurring during the palpation of the painful spot suggests costochondritis but the pain could also have a cardiac origin [8] [4] tumor [4] [3] [1]. From the pain of inflammation, the normal movement in joints is disrupted, the movements of the shoulder crepitates and pain may occur. [1][3][4] Complaints occur gradually and can disappear spontaneously after some days but it may take years to disappear. [1][10] Even after a spontaneously healing, the complaints can return on the same place or another spot around the costae. [1][7]
Clinically, the syndrome is characterized by inflammation of the costal cartilage .It is associated with gradual or rapid onset of pain and swelling of the upper costal cartilage of the costochondral junction. Pain is intensified by cough, sneezing and chest movements [12). There are no systemic symptoms or adenopathy (13)
• 6 Differential Diagnosis
Costochondritis also known as costosternal syndrome, parasternal chondrodynia, or anterior chest wall syndrome. In the medical world costochondritis is often confused with Tietze syndrome, a similar but rarer disorder involving swelling of a single costal cartilage, usually of the second rib.14
The symptoms and signs of Tietze’s syndrome may occur in all arthropathies involving the anterior chest wall, particularly in seronegative spondylarthropathy and rheumatoid arthritis luckily these are distinguished easily by their other clinical features. Other sometimes mistaken for Tietze’s syndrome skeletal causes are xiphoidalgia and slipping rib syndrome. Besides these pathologies, there are many other diseases to consider in the differential diagnosis, such as multiple myeloma, primitive neoplasms of the bone and soft tissues, chondrosarcoma of the chondrocostal joints, breast and lung tumors with extension to the costal cartilage, as well as metastases of breast, kidney, and prostate neoplasms [11]. Consequently malignancy should always be kept in mind in the differential diagnosis of Tietze’s syndrome. The use of the appropriate other investigations such as electrocardiography [[12] [3], CT-scan [13] [5], MRI [5] [12] [14]… is necessary.
• 7 Diagnostic Procedures
Patients with fever, chest wall swelling, cough or other respiratory issues should first have a chest examination. With computer tomography (CT) can delineate a pathology in costal cartilages and rule out underlying pathologies like tumors. CT is only reserved for cases where is high suspicion of neoplastic processes or infections. Nuclear scanning with Technetium 99 scitigraphy is not usefull for identifying costochrondritis. There is also one case report who have found sings of inflammation on gallium or bone scanning.15
Patients older than 35 years old who have a history with coronary artery disease, and patients with cardio pulmonary symptoms should have electrocardiography and possibly chest radiography. Further testing should be considered for ruling out a cardiac cause if clinically indicated by age or risk status.15
Routine laboratory testing is not necessary in patients with suspected costochrondritis unless there the diagnosis is uncertain or when there are signs of inflammation.
• 8 Outcome Measures
VAS :The use of the VAS can be used to asses pain before and after the treatment,During rest and during inhale/exhale exercise. .another case study examined the cervical spine mobility.17,18
Patient-specifiv functional scale ( PSFS) : specific questionnaires for costochondritis have not yet been assembled in the literature, but the PSFS has been stated to be a valid, reproducable, and responsive outcome measure for patients with neck pain, back pain, and upper quarter complaints19
The Global rating of change (GROC): To measure the patient’s subjective rate of improvement, the GROC has been stated to be reliable .19
• 9 Examination
Patients with Costochondritis will show chest pain that is reproducable by palpation of the affected area, mostly rib 2 to 5.and in most patients several ribs are affected.Other aggrevations are couching or exercise.It occurs often after a recent illness with coughing or a heavy exercise.most of the times it is unilateral.15
-palpation: palpation should be performed with 1 digit, on the naterior, posterior and lateral side of the chest, the clavicula,the cervical and thoracic spine. When on the affected area reveals a reproducable pain this might suggest Costochondritis but it cannot entirely conclude it.15
In a small number of patients the cardiac pain is due to cardiac causes.in 3-6% of the patients with pain to palpation a myocard infarction has occurred.patients older then 35 and with a history of cardiac problems have a higher risk.they should reveive a ecg and chest radiography.15
• 10 Medical Management
The first line treatment for peripheral enthesitis are local corticosteroid injections when only a few entheses are involved. When there is an inadequately respons to local corticosteroid injections by patients with multiple peripheral enthesitis , oral NSAIDs should be used. There is no evidence for the efficacy of sulfasalazine and methotrexate for the treatment of peripheral enthestis. The optimal treatment of costochrondritis has not been established.
• 11 Physical Therapy Management
The treatment of Tietze’s syndrome is not yet perfect. It is not known weather the disease is dealt definitly or not.[3] For now, trustworthy clinical studies on the treatment of Tietze's syndrome are lacking [8][4][6].
There are no randomized controlled trials or even quasiexperimental trials testing different interventions. Only case reports, case series, retrospective studies and expert opinion are available for both conservative and pharmaceutical interventions.
Treatment is usually directed at pain relief with acetaminophen, nonsteroidal anti-inflammatory drugs when safe and appropriate, or other analgesics. Applying heat with compresses or heating pads can help, particularly in the case of muscle overuse. Minimizing activities that provoke the symptoms (e.g., reducing the frequency or intensity of exercise or work activities) or using cough suppressants may also help relieve symptoms15 (Level of evidence:5)
The use of high-velocity, low-amplitude manipulation applied to the associated hypokinetic costovertebral, costotransverse, and intervertebral zygapophyseal thoracic joints improves the pain level, as well as instrument-assisted soft tissue mobilization using the Graston technique26 (Level of evidence:4)
Recommendations for the management of Costochondritis:*
- Reassure the patient by explaining the benign nature of the condition. what should he/she say? [8] [4]
- Correction of muscle imbalances through cervical and thoracic region, including
pectoralis muscles.
- Reinforcement of correction via postural re-education and exercise can decrease loads placed on the joints of the anterior chest wall.17 (Level of evidence 4)
Patients need a good balance between exercise and rest.[8][10][7][6]
- Conservative treatment involving use of nonsteroidal anti-inflammatory drugs (NSAIDs) or analgesics, as necessary.23
- Mobilize spine and ribs to avoid rigidity of the thorax and to reduce complaints. [10][3]
- Teach the patient breathing exercises [3]
- Cough suppressants may be beneficial if cough is an aggravating factor.23
- Learn the patient to cope with pain. [8][6]
- Exercise for shoulder and back can be provocative, therefore only when the complaints have disappeared, they can be applied
[3]
* No strong recommendation were made for the physical therapy management of Costochondritis. The evidence supporting these interventions demonstrated only a small or moderate effect size.
• 12 Key Evidence
ANNE M. PROULX. Costochondritis: Diagnosis and Treatment. Am Fam.Physician. 2009 Sep 15; 80(6):617-620.15
• 13 Resources
http://www.ncbi.nlm.nih.gov/pubmed/22787240
http://www.ncbi.nlm.nih.gov/pubmed/19827277
http://www.ncbi.nlm.nih.gov/pubmed/17360222
• 14 Clinical Bottom Line Missing information
There is too few high level evidence concerning the physical treatment of costochondritis, the recommended therapy consist out of analgetics and muscular training ,as well as decreasing the prococative activities.Most ofthe patients will have their pain resolvd within a year..However ,a lot of the study’s are outdated, we recommend to achieve newer ,more recent information about the treatmentof costochondritis
• 15 Recent Related Research (from Pubmed)
Ayloo A1, Cvengros T, Marella S.Evaluation and treatment of musculoskeletal chest pain. Prim Care. 2013 Dec;40(4):863-87, viii. doi: 10.1016/j.pop.2013.08.007.
Gandhi V1, Costello J.
Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 3: The use of corticosteroids in the management of costochondritis. Emerg Med J. 2012 Aug;29(8):686. doi: 10.1136/emermed-2012-201590.4.
Grindstaff TL1, Beazell JR, Saliba EN, Ingersoll CD.
Treatment of a female collegiate rower with costochondritis: a case report. J Man Manip Ther. 2010 Jun;18(2):64-8. doi: 10.1179/106698110X12640740712653.
• 16 References
1. Bickley LS, Szilagyi PG. Bates' Guide to Physical Examination and History Taking. 8th ed Philadelphia, Pa: Lippincott Williams & Wilkins. 2003. (level 5)
2. Saltzman DA, Schmitz ML, Smith SD, Wagner CW, Jackson RJ, Harp S. The slipping rib syndrome in children. Paediatr Anaesth. 2001;11(6):740-743. (level 3A)
3. Fam AG. Approach to musculoskeletal chest wall pain. Prim Care. 1988;15(4):767-782. (level 2B)
4. Wise CM, Semble EL, Dalton CB. Musculoskeletal chest wall syndromes in patients with noncardiac chest pain: a study of 100 patients. Arch Phys Med Rehabil. 1992;73(2):147-149. (level 4)
5. Pantell RH, Goodman BW Jr. Adolescent chest pain: a prospective study. Pediatrics. 1983;71(6):881-887. (level 2B)
6. Costochondritis. Stedman's Online Medical Dictionary. http://www.stedmans.com/section.cfm/45. Accessed April 15, 2009. (level 5)
7. Kayser HL. Tietze's syndrome: a review of the literature. Am J Med. 1956;21(6):982-989. (level 1A)
8. Massin MM, Bourguignont A, Coremans C, Comté L, Lepage P, Gérard P. Chest pain in pediatric patients presenting to an emergency department or to a cardiac clinic. Clin Pediatr (Phila). 2004;43(3):231-238. (level 1B)
9. Klinkman MS, Stevens D, Gorenflo DW. Episodes of care for chest pain: a preliminary report from MIRNET. Michigan Research Network. J Fam Pract. 1994;38(4):345-352. (level 2B)
10. Buntinx F, Knockaert D, Bruyninckx R, et al. Chest pain in general practice or in the hospital emergency department: is it the same? Fam Pract. 2001;18(6):586-589. (level 2b)
11. Beck WC, Berkeheiser S. Prominent costal cartilages (Tietze’s syndrome). Surgery 1954;35:762–5. (level 4)
12. Motulsky AG, Rhon RJ. Tietze’s syndrome. J Am Med Assoc 1953;152:504–6. (level 1B)
13. Martino F, D’Amore M, Angdelli G, Macarini L, Cantatore FP. Echographic study of Tietze’s syndrome. Clin Rheumatol 1991;10:2–4. (level 5)
14. Fam AG. Approach to musculoskeletal chest wall pain. Prim Care. 1988;15(4):767-782 (Level 3A)
15)Proulx, A. M., & Zryd, T. W. (2009). Costochondritis: Diagnosis and treatment. American Family Physician, 80(6), 617–620. doi:10.1016/S0015-1882(09)70196 (level 3A)
16)Freeston J1 Can early diagnosis and management of costochondritis reduce acute chest pain admissions?
2004, J Rheumatol. 2004 Nov;31(11):2269-71. (level 2B)
17)Terry L Grindstaff.Treatment of a female collegiate rower with costochondritis: a case report. J Man Manip Ther. 2010 June; 18(2): 64–68. (Level 4)
18)Karen Hudes.Low-tech rehabilitation and management of a 64 year old male patient with acute idiopathic onset of costochondritis. J Can Chiropr Assoc. 2008 December; 52(4): 224–228. (LOE 4)(level 4)
19)Richard B. Westrick,.EVALUATION AND TREATMENT OF MUSCULOSKELETAL CHEST WALL PAIN IN A MILITARY ATHLETE. Int J Sports Phys Ther. 2012 June; 7(3): 323–332(LOE 4)(level 4)
20)Wise CM, Semble EL, Dalton CB. Musculoskeletal chest wall syndromes in patients with noncardiac chest pain: a study of 100 patients. Arch Phys Med Rehabil. 1992;73(2):147-149. (level 1B)
21) Disla E, Rhim HR, Reddy A, Karten I, Taranta A. Costochondritis. A prospective analysis in an emergency department setting. Arch Intern Med. 1994;154(21):2466-2469. (Level 2B)
22)Miller CD, Lindsell CJ, Khandelwal S, et al. Is the initial diagnostic impression of “noncardiac chest pain” adequate to exclude cardiac disease? [published correction appears in Ann Emerg MedCayley WE Jr. Diagnosing the cause of chest pain. Am Fam Physician. 2005;72(10):2012-2021.. 2005;45(1):87]. Ann Emerg Med. 2004;44(6):565-57 (level 2B)
23) Rovetta G, Sessarego P, Monteforte P. Stretching exercises for costochondritis pain. G Ital Med Lav Ergon. Apr-Jun 2009;31(2):169-71 (level 3A)
24. Disla E, Rhim HR, Reddy A, Karten I, Taranta A. Costochondritis. A prospective analysis in an emergency department setting. Arch Intern Med. 1994;154(21):2466-2469. (level 2B)
25.Biundo JJ Jr. Regional rheumatic pain syndrome. In: Schumachar R Jr, Klippel J, Robinson R, eds. Primer on the rheumatic diseases. Atlanta, GA: Arthritic Foundation, 1988:263–74. (Level 1B)
26. Aspegren D et al., Conservative treatment of a female collegiate volleyball player with costochondritis., J Manipulative Physiol Ther. 2007 May;30(4):321-5. (LOE 4)(Level 4)
27. D’Angelo, S., Padula, A., Nigro, A., Cantini, F., Matucci-Cerinic, M., Modena, V., … Olivieri, I. (2008). Italian evidence-based recommendations for the management of ankylosing spondylitis: The 3E Initiative in rheumatology. Clinical and Experimental Rheumatology, 26(6), 1005–1011. (Level 1B)