Conceptual Models of Disability and Functioning: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
</div><div align="justify"> | </div><div align="justify"> | ||
== Introduction == | == Introduction == | ||
Models of disability and functioning are tools that are used to define impairment and more recently functioning, which are utilised by governments and society to devise strategies and policy for meeting the needs of those who have a loss in function as a result of health condition, disease or injury. While they provide a framework in which we can gain an understanding of impairment, disability and functioning, there is lots of contention, and discussion around the models. Overall these models reveal or reflect how society provides or limits access to work, goods, services, economic influence and political power for people with a disability or loss of function, and provide some insight into the attitudes, conceptions and prejudices in society. These models have changed as society has changed, and understanding the development and use of these models can provide us with a continuum on the changing societal attitudes towards disability and loss of functioning. | |||
These conceptual models should be used not only to define disability but also to consider functioning, and more importantly to understand the impact of disability and context-specific factors on function. The models have applications for quantitative and qualitative assessment of disability and functioning, to inform needs and resources, monitor costs, direct social policy, and maximize awareness and acceptance globally. | |||
== Medical Model == | |||
Historically approaches towards health and disease has been very much focused on the medical or biological model where a person’s ill-health was exclusively thought to be related to pathology and treated purely by medical means. In more recent times thinking has moved towards a more functional model.The medical or biomedical model of disability is focused on pathology and impairment, which describes disability as a consequence of a health condition, disease or injury/trauma that can disrupt the functioning of a person in a physiological or cognitive way. It then focuses on the prevention or treatment of the condition, which is generally lead by the physician who directs the delivery of the service, with the physician being the decision maker in the process. There has been a lot of discontent with this model, which may feel assumes several unhelpful notions about the nature of disability. This model was born around the first world war, where Rehabilitation was born around the time of the First World War when there was a strong philosophy of the doctor telling injured servicemen how to behave, how to get better, and how to get back as quickly as possible to active duty. Such a model may have been appropriate in that cultural context but not in wider society today. | |||
== Social Model == | == Social Model == | ||
The social model of disability views disability not as an underlying medical condition or pathology but rather as secondary to the social, legislative, and attitudinal environment in which the person lives. Although a person’s abilities may be different, the disability is because society either actively discriminates against the person with a disability or it fails to account for their different needs. The key features of the social model include; | The social model of disability views disability not as an underlying medical condition or pathology but rather as secondary to the social, legislative, and attitudinal environment in which the person lives. Although a person’s abilities may be different, the disability is because society either actively discriminates against the person with a disability or it fails to account for their different needs. The key features of the social model include; | ||
== Human Development Model - Disability Creation Process (HDM-DCP) == | |||
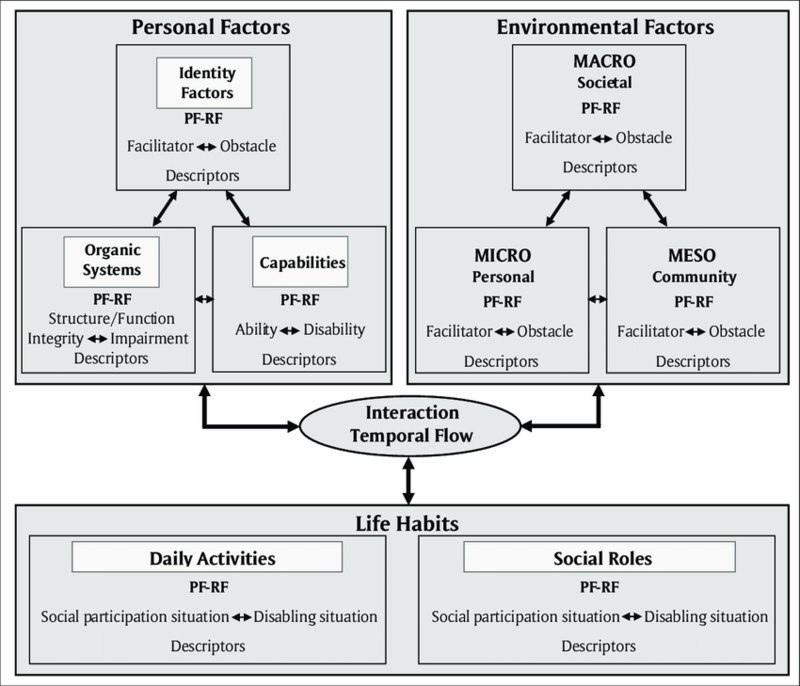
Designed to focus on the adaptation, rehabilitation, social participation and exercise of human rights of people with a disability and their families, the [https://ripph.qc.ca/en/hdm-dcp-model/the-model/ Human Development-Disability Creation Process], is a conceptual model that aims to document and explain the causes and consequences of disease, trauma, and other effects on the development of the person. Research, directed by Patrick Fougeyrollas in 1988, led to the development of the initial model in 1998,<ref>International Network on the Disability Creation Process. The HDM-DCP Model - History of the Model. Available from: https://ripph.qc.ca/en/hdm-dcp-model/history-of-the-model/ (accessed on 26/06/2021)</ref> which differed from other human development models at the time in that it incorporated the concepts of “risk factors”, “organic systems” and “capabilities” and was the first introduce the environmental factors dimension highlighting the interaction between impairments, disabilities and environmental obstacles, and defined disabling situations as the result of this interaction. <ref name=":0">International Network on the Disability Creation Process. The HDM-DCP Model - The Model. Available from: https://ripph.qc.ca/en/hdm-dcp-model/the-model/ (accessed on 26/06/2021)</ref>[[File:Human-Development-Model-and-Disability-Creation-Process-HDM-DCP-Legend-PF-RF.png|center|frameless|800x800px]]This model recognises the role that rehabilitation has in allowing an individual to reinforce their abilities, while compensating for the loss in function and consider that “environmental factors” found in a person’s or population’s environment may be either facilitators or obstacles e.g. a prejudice, the lack of assistance or resources, the lack of accessibility at home and at school, a problem in obtaining adapted printed information or moving around with the help of accessible signage. It allows us to view the impact of the environment, and provides us with an indicator of the quality of social participation, which is measured over a continuum or scale ranging from an optimal situation of social participation to a complete disabling situation.<ref name=":0" /> | |||
== Biopsychosocial Model == | == Biopsychosocial Model == | ||
The [[Biopsychosocial Model | The [[Biopsychosocial Model]] of disability is an attempt to account for both the social and biomedical models of disability. First conceptualised by George Engel in 1977, it suggests that to understand a person's medical condition it is not simply the biological factors that need to be considered, but also the psychological and social factors <ref name="gatchel">Gatchel, Robert J., Peng, Yuan Bo, Peters, Madelon, L.; Fuchs, Perry, N.; Turk, Dennis C. 2007 The biopsychosocial approach to chronic pain: Scientific advances and future directionsfckLR Psychological Bulletin, Vol 133(4), 581-624</ref>. | ||
*Bio (physiological pathology) | *Bio (physiological pathology) | ||
*Psycho (thoughts emotions and behaviours such as psychological distress, fear/avoidance beliefs, current coping methods and attribution) | *Psycho (thoughts emotions and behaviours such as psychological distress, fear/avoidance beliefs, current coping methods and attribution) | ||
*Social (socio-economical, socio-environmental, and cultural factors such as; work issues, family circumstances and benefits/economics) | *Social (socio-economical, socio-environmental, and cultural factors such as; work issues, family circumstances and benefits/economics) | ||
The WHO [[International Classification of Functioning, Disability and Health (ICF)|International Classification of Functioning, Disability and Health]] is underpinned by the Biopsychosocial Model. There has been some controversy around incorporating aspects of health within a model of disability from those that use the social model of disability, as they would define disability as being solely due to a lack of response of society to change the environment to accommodate the needs of the individual. The full ICF is a detailed and lengthy document, which recognises the importance not only of describing the functioning of an individual but also placing such functioning into its social context. | The WHO [[International Classification of Functioning, Disability and Health (ICF)|International Classification of Functioning, Disability and Health]] is underpinned by the Biopsychosocial Model. There has been some controversy around incorporating aspects of health within a model of disability from those that use the social model of disability, as they would define disability as being solely due to a lack of response of society to change the environment to accommodate the needs of the individual. The full ICF is a detailed and lengthy document, which recognises the importance not only of describing the functioning of an individual but also placing such functioning into its social context. | ||
=== | === References === | ||
= | |||
<references /> | <references /> | ||
Revision as of 00:22, 29 June 2021
Original Editors - Add your name/s here if you are the original editor/s of this page. User Name
Top Contributors - Naomi O'Reilly, Admin, Tarina van der Stockt, Kim Jackson, Oyemi Sillo, Olajumoke Ogunleye, Wanda van Niekerk, Lucinda hampton and Ashmita Patrao
Introduction[edit | edit source]
Models of disability and functioning are tools that are used to define impairment and more recently functioning, which are utilised by governments and society to devise strategies and policy for meeting the needs of those who have a loss in function as a result of health condition, disease or injury. While they provide a framework in which we can gain an understanding of impairment, disability and functioning, there is lots of contention, and discussion around the models. Overall these models reveal or reflect how society provides or limits access to work, goods, services, economic influence and political power for people with a disability or loss of function, and provide some insight into the attitudes, conceptions and prejudices in society. These models have changed as society has changed, and understanding the development and use of these models can provide us with a continuum on the changing societal attitudes towards disability and loss of functioning.
These conceptual models should be used not only to define disability but also to consider functioning, and more importantly to understand the impact of disability and context-specific factors on function. The models have applications for quantitative and qualitative assessment of disability and functioning, to inform needs and resources, monitor costs, direct social policy, and maximize awareness and acceptance globally.
Medical Model[edit | edit source]
Historically approaches towards health and disease has been very much focused on the medical or biological model where a person’s ill-health was exclusively thought to be related to pathology and treated purely by medical means. In more recent times thinking has moved towards a more functional model.The medical or biomedical model of disability is focused on pathology and impairment, which describes disability as a consequence of a health condition, disease or injury/trauma that can disrupt the functioning of a person in a physiological or cognitive way. It then focuses on the prevention or treatment of the condition, which is generally lead by the physician who directs the delivery of the service, with the physician being the decision maker in the process. There has been a lot of discontent with this model, which may feel assumes several unhelpful notions about the nature of disability. This model was born around the first world war, where Rehabilitation was born around the time of the First World War when there was a strong philosophy of the doctor telling injured servicemen how to behave, how to get better, and how to get back as quickly as possible to active duty. Such a model may have been appropriate in that cultural context but not in wider society today.
Social Model[edit | edit source]
The social model of disability views disability not as an underlying medical condition or pathology but rather as secondary to the social, legislative, and attitudinal environment in which the person lives. Although a person’s abilities may be different, the disability is because society either actively discriminates against the person with a disability or it fails to account for their different needs. The key features of the social model include;
Human Development Model - Disability Creation Process (HDM-DCP)[edit | edit source]
Designed to focus on the adaptation, rehabilitation, social participation and exercise of human rights of people with a disability and their families, the Human Development-Disability Creation Process, is a conceptual model that aims to document and explain the causes and consequences of disease, trauma, and other effects on the development of the person. Research, directed by Patrick Fougeyrollas in 1988, led to the development of the initial model in 1998,[1] which differed from other human development models at the time in that it incorporated the concepts of “risk factors”, “organic systems” and “capabilities” and was the first introduce the environmental factors dimension highlighting the interaction between impairments, disabilities and environmental obstacles, and defined disabling situations as the result of this interaction. [2]This model recognises the role that rehabilitation has in allowing an individual to reinforce their abilities, while compensating for the loss in function and consider that “environmental factors” found in a person’s or population’s environment may be either facilitators or obstacles e.g. a prejudice, the lack of assistance or resources, the lack of accessibility at home and at school, a problem in obtaining adapted printed information or moving around with the help of accessible signage. It allows us to view the impact of the environment, and provides us with an indicator of the quality of social participation, which is measured over a continuum or scale ranging from an optimal situation of social participation to a complete disabling situation.[2]Biopsychosocial Model[edit | edit source]
The Biopsychosocial Model of disability is an attempt to account for both the social and biomedical models of disability. First conceptualised by George Engel in 1977, it suggests that to understand a person's medical condition it is not simply the biological factors that need to be considered, but also the psychological and social factors [3].
- Bio (physiological pathology)
- Psycho (thoughts emotions and behaviours such as psychological distress, fear/avoidance beliefs, current coping methods and attribution)
- Social (socio-economical, socio-environmental, and cultural factors such as; work issues, family circumstances and benefits/economics)
The WHO International Classification of Functioning, Disability and Health is underpinned by the Biopsychosocial Model. There has been some controversy around incorporating aspects of health within a model of disability from those that use the social model of disability, as they would define disability as being solely due to a lack of response of society to change the environment to accommodate the needs of the individual. The full ICF is a detailed and lengthy document, which recognises the importance not only of describing the functioning of an individual but also placing such functioning into its social context.
References [edit | edit source]
- ↑ International Network on the Disability Creation Process. The HDM-DCP Model - History of the Model. Available from: https://ripph.qc.ca/en/hdm-dcp-model/history-of-the-model/ (accessed on 26/06/2021)
- ↑ 2.0 2.1 International Network on the Disability Creation Process. The HDM-DCP Model - The Model. Available from: https://ripph.qc.ca/en/hdm-dcp-model/the-model/ (accessed on 26/06/2021)
- ↑ Gatchel, Robert J., Peng, Yuan Bo, Peters, Madelon, L.; Fuchs, Perry, N.; Turk, Dennis C. 2007 The biopsychosocial approach to chronic pain: Scientific advances and future directionsfckLR Psychological Bulletin, Vol 133(4), 581-624