Compartment Syndrome of the Lower Leg: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- [[User:Geoffrey De Vos|Geoffrey De Vos]] | '''Original Editors '''- [[User:Geoffrey De Vos|Geoffrey De Vos]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
Compartment syndrome of the lower leg has been defined as a condition which increased the pressure in a small place. This compromises the circulation and function of the tissues within that space. It is most commonly seen after injuries to the leg and forearm, but also occur in the arm, thigh, foot, buttock, hand and abdomen.<sup>[4]</sup> This condition ensures that there will be compression on nervers, blood vessels and muscle(s) inside the compartment of the lower leg.<sup>[</sup><sup>2,3,4] </sup><br>This injury may lead to tissue death (necrosis) due to the blood vessels being compressed by the raised pressure within the compartment. So this compression causes an ischemia, a lack of oxygen, that can result in serious and dangerous tissue damages or tissue death when this injury isn’t treated well. In the literature the speak about three types of compartment syndrome. It can be divided into acute (ACS) , subacute, and chronic compartment syndrome (CECS).[1]<br>Acute compartment syndrome (ACS) is caused by bleeding or oedema in a closed, non-elastic muscle compartment which is surrounded by fascia and bone. Among the most common causes of this complication are fractures, blunt trauma and reperfusion injury after acute arterial obstruction. Increasing intracompartmental pressure may lead to nerve damage and reduced tissue perfusion resulting in muscle ischaemia or necrosis mediated by infiltrating neutrophils.[6]<br>Chronic compartment syndrome (CCS) is is a common injury in young athletes, causing pain in the involved leg compartment during strenuous exercise.[10,11] It is clinically manifest by recurrent episodes of muscle cramping, tightness, and occasional paresthesias.[13] Also their is an increase of pressure in skeletal muscle accompanied by pain, swelling, and impaired muscle function. Unlike other exertional injuries such as stress fracture, periostitis, or tendonitis, this problem does not respond to antiinflammatory medications or physical therapy.[10,11]<br>This syndrome occurs fairly regularly and occurs in most of the times in athletes, such as long distance runners, soccer players, basketball players and military men and women.[7,13] It can also occur in children, adolescents or adults, but more often in adults.[2,3] | Compartment syndrome of the lower leg has been defined as a condition which increased the pressure in a small place. This compromises the circulation and function of the tissues within that space. It is most commonly seen after injuries to the leg and forearm, but also occur in the arm, thigh, foot, buttock, hand and abdomen.<sup>[4]</sup> This condition ensures that there will be compression on nervers, blood vessels and muscle(s) inside the compartment of the lower leg.<sup>[</sup><sup>2,3,4] </sup><br>This injury may lead to tissue death (necrosis) due to the blood vessels being compressed by the raised pressure within the compartment. So this compression causes an ischemia, a lack of oxygen, that can result in serious and dangerous tissue damages or tissue death when this injury isn’t treated well. In the literature the speak about three types of compartment syndrome. It can be divided into acute (ACS) , subacute, and chronic compartment syndrome (CECS).[1]<br>Acute compartment syndrome (ACS) is caused by bleeding or oedema in a closed, non-elastic muscle compartment which is surrounded by fascia and bone. Among the most common causes of this complication are fractures, blunt trauma and reperfusion injury after acute arterial obstruction. Increasing intracompartmental pressure may lead to nerve damage and reduced tissue perfusion resulting in muscle ischaemia or necrosis mediated by infiltrating neutrophils.[6]<br>Chronic compartment syndrome (CCS) is is a common injury in young athletes, causing pain in the involved leg compartment during strenuous exercise.[10,11] It is clinically manifest by recurrent episodes of muscle cramping, tightness, and occasional paresthesias.[13] Also their is an increase of pressure in skeletal muscle accompanied by pain, swelling, and impaired muscle function. Unlike other exertional injuries such as stress fracture, periostitis, or tendonitis, this problem does not respond to antiinflammatory medications or physical therapy.[10,11]<br>This syndrome occurs fairly regularly and occurs in most of the times in athletes, such as long distance runners, soccer players, basketball players and military men and women.[7,13] It can also occur in children, adolescents or adults, but more often in adults.[2,3] | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
| Line 22: | Line 18: | ||
The lateral compartment include M. peroneus longus and brevis and also the N. superficial peroneal. The deep posterior compartment include M. tibialis posterior, M. flex. hallucis longus, M. flex. digitorum longus, M. popliteus, A. tibialis posterior and the N. tibialis. The superficial posterior compartment include the M. gastrocnemius, M. soleus, M. plantaris and N. sural. 1All this compartments are surrounded by fascia. This fascia is connected to bone and each of them has a blood and nerve supply. These fascias do not expand and when a compartment swells the pressure inside the compartment will increase which will cause tissue necrosis due by the compressing of blood vessels and nerves.<sup>[9,19]</sup> <br> | The lateral compartment include M. peroneus longus and brevis and also the N. superficial peroneal. The deep posterior compartment include M. tibialis posterior, M. flex. hallucis longus, M. flex. digitorum longus, M. popliteus, A. tibialis posterior and the N. tibialis. The superficial posterior compartment include the M. gastrocnemius, M. soleus, M. plantaris and N. sural. 1All this compartments are surrounded by fascia. This fascia is connected to bone and each of them has a blood and nerve supply. These fascias do not expand and when a compartment swells the pressure inside the compartment will increase which will cause tissue necrosis due by the compressing of blood vessels and nerves.<sup>[9,19]</sup> <br> | ||
Picture: http://www.clinorthop.org/volume/468/issue/4 | Picture: http://www.clinorthop.org/volume/468/issue/4 | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
The average annual incidence of ACS for men are 7.3 per 100.000 and by women 0.7 per 100.000. To most of the patients are young men with fractures of the tibial diaphysis, with a injury to the soft tissues or those with a bleeding diathesis. Any condition that results in an increase of pressure in a compartment can lead to the development of an acute (ACS) or chronic exertional compartment syndrome (CECS). <br>In most of the times ACS occurs after: <sup>[8,9]</sup> | The average annual incidence of ACS for men are 7.3 per 100.000 and by women 0.7 per 100.000. To most of the patients are young men with fractures of the tibial diaphysis, with a injury to the soft tissues or those with a bleeding diathesis. Any condition that results in an increase of pressure in a compartment can lead to the development of an acute (ACS) or chronic exertional compartment syndrome (CECS). <br>In most of the times ACS occurs after: <sup>[8,9]</sup> | ||
<blockquote> | <blockquote> | ||
*Fracture of the tibial diaphysis | *Fracture of the tibial diaphysis | ||
*Soft-tissue injury | *Soft-tissue injury | ||
*Intensive muscle use | *Intensive muscle use | ||
*Everyday extreme exercise activities | *Everyday extreme exercise activities | ||
*Arterial injury | *Arterial injury | ||
*Drug overdose | *Drug overdose | ||
*Burns | *Burns | ||
</blockquote> | </blockquote> | ||
<br>One of the main causes of CECS is repetitive and strenuous exercise (sports). During strenuous exercise, there can be up to a 20% increase in muscle volume and weight due to increased blood flow and oedema, so the pressure increases.<sup>[2] </sup>Oedema of the soft tissue within the compartment further raises the intra-compartment pressure, which compromises venous and lymphatic drainage of the injured area. If the pressure further increases, it will eventually turn into a vicious circle, that can lead to tissue ischemia. The normal mean interstitial tissue pressure in relaxed muscles is ± 10-12 mmHg. If this pressure elevates to 30 mmHg or more, small vessels in the tissue become compressed, which leads to reduced nutrient blood flow, ischemia and pain.<sup>[1,2] </sup>The anterior compartment is affected more frequently than the lateral, deep and superficial posterior compartments.<sup>[7]</sup><br><br> | <br>One of the main causes of CECS is repetitive and strenuous exercise (sports). During strenuous exercise, there can be up to a 20% increase in muscle volume and weight due to increased blood flow and oedema, so the pressure increases.<sup>[2] </sup>Oedema of the soft tissue within the compartment further raises the intra-compartment pressure, which compromises venous and lymphatic drainage of the injured area. If the pressure further increases, it will eventually turn into a vicious circle, that can lead to tissue ischemia. The normal mean interstitial tissue pressure in relaxed muscles is ± 10-12 mmHg. If this pressure elevates to 30 mmHg or more, small vessels in the tissue become compressed, which leads to reduced nutrient blood flow, ischemia and pain.<sup>[1,2] </sup>The anterior compartment is affected more frequently than the lateral, deep and superficial posterior compartments.<sup>[7]</sup><br><br> | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Patients with compartment syndrome of the lower leg suffer from long term impairment such as reduced muscular strength, reduced range of motion and pain.<sup>[6] </sup><br>The most common symptoms by a compartment syndrome are:<sup>[9]</sup> | Patients with compartment syndrome of the lower leg suffer from long term impairment such as reduced muscular strength, reduced range of motion and pain.<sup>[6] </sup><br>The most common symptoms by a compartment syndrome are:<sup>[9]</sup> | ||
<blockquote> | <blockquote> | ||
*Feeling of tightness | *Feeling of tightness | ||
*Swelling | *Swelling | ||
*Pain (by active flexion knee and particularly passive stretching of the muscles) | *Pain (by active flexion knee and particularly passive stretching of the muscles) | ||
*Paresthesia | *Paresthesia | ||
</blockquote> | </blockquote> | ||
<br>Pain and swelling are the leading symptoms in this disease and it appears and aggravates during physical activities such as running and other sports like basketball and soccer. The pain is usually located over<br>the involved compartments and may radiate to the ankle or foot. Burning, cramping, or aching pain and tightness develop while exercising. In extreme cases (no or bad treatment) it is possible that the lower leg, ankle and foot can be paralysed.<sup>[2]</sup> (C Reid D. et al)<br><br><br> | <br>Pain and swelling are the leading symptoms in this disease and it appears and aggravates during physical activities such as running and other sports like basketball and soccer. The pain is usually located over<br>the involved compartments and may radiate to the ankle or foot. Burning, cramping, or aching pain and tightness develop while exercising. In extreme cases (no or bad treatment) it is possible that the lower leg, ankle and foot can be paralysed.<sup>[2]</sup> (C Reid D. et al)<br><br><br> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 61: | Line 57: | ||
'''<u>Neurological symptoms and signs:</u>'''<br>Paraesthesia and hypoesthesia may occur in the territory of the nerves traversing the affected compartment and are usually the first signs of nerve ischaemia, although sensory abnormality may be the result of concomitant nerve injury. Ulmer reports a sensitivity of 13 % and specificity of 98 % for the clinical finding of paraesthesia in ACS, a false-negative rate that precludes this symptom from being a useful diagnostic tool.<br>Paralysis of muscles contained in the affected compartments is recognised as being a late sign and has equally low sensitivity as others in predicting the presence of ACS, probably because of the difficulty in interpreting the underlying cause of the weakness, which could be inhibition by pain, direct injury to muscle, or associated nerve injury. | '''<u>Neurological symptoms and signs:</u>'''<br>Paraesthesia and hypoesthesia may occur in the territory of the nerves traversing the affected compartment and are usually the first signs of nerve ischaemia, although sensory abnormality may be the result of concomitant nerve injury. Ulmer reports a sensitivity of 13 % and specificity of 98 % for the clinical finding of paraesthesia in ACS, a false-negative rate that precludes this symptom from being a useful diagnostic tool.<br>Paralysis of muscles contained in the affected compartments is recognised as being a late sign and has equally low sensitivity as others in predicting the presence of ACS, probably because of the difficulty in interpreting the underlying cause of the weakness, which could be inhibition by pain, direct injury to muscle, or associated nerve injury. | ||
<u>'''Swelling:'''</u><br>Swelling in the compartment affected can be a sign of ACS, although the degree of swelling is difficult to assess accurately, making this sign very subjective. The compartment may be obscured by casts, dressing, or other muscle groups, for example in the case of the deep posterior compartment. Poor sensitivity, specificity, and negative and positive predictive values have been demonstrated when manual palpation was used to determine whether ICP was raised in cadaveric limbs.<br><br> | <u>'''Swelling:'''</u><br>Swelling in the compartment affected can be a sign of ACS, although the degree of swelling is difficult to assess accurately, making this sign very subjective. The compartment may be obscured by casts, dressing, or other muscle groups, for example in the case of the deep posterior compartment. Poor sensitivity, specificity, and negative and positive predictive values have been demonstrated when manual palpation was used to determine whether ICP was raised in cadaveric limbs.<br><br> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 218: | Line 214: | ||
|} | |} | ||
<br> | <br> | ||
== Outcome Measures == | == Outcome Measures == | ||
The most important determinant of a poor outcome from acute compartment syndrome after injury is delay in diagnosis. The complications are usually disabling and include infection, contracture and amputation. One of the main causes of delay may be insufficient awareness of the condition. While it is acknowledged that children, because of difficulty in assessment, and hypotensive patients are at risk, most adults who develop acute compartment syndrome are not hypotensive. Awareness of the risk of the syndrome may reduce delay in diagnosis. Continuous monitoring of compartment pressure may allow the diagnosis to be made earlier and complications to be minimised.<br>Early diagnosis and treatment are of the utmost importance in order to avoid long-term disability after acute compartment syndrome.<sup>[8]</sup><br> | The most important determinant of a poor outcome from acute compartment syndrome after injury is delay in diagnosis. The complications are usually disabling and include infection, contracture and amputation. One of the main causes of delay may be insufficient awareness of the condition. While it is acknowledged that children, because of difficulty in assessment, and hypotensive patients are at risk, most adults who develop acute compartment syndrome are not hypotensive. Awareness of the risk of the syndrome may reduce delay in diagnosis. Continuous monitoring of compartment pressure may allow the diagnosis to be made earlier and complications to be minimised.<br>Early diagnosis and treatment are of the utmost importance in order to avoid long-term disability after acute compartment syndrome.<sup>[8]</sup><br> | ||
== Examination == | == Examination == | ||
<u>Palpation of the lower leg:</u> If there is a compartment syndrome, you can feel a firm, wooden feeling of the leg.<sup>[9]</sup><br><u>Children:</u> Identification of evolving CS in a child is difficult because of the child’s limited ability to communicate and anxiety about being examined by a stranger. Orthopedists are trained to look for the 5 P’s (pain, paresthesia, paralysis, pallor, pulselessness) associated with CS. Examining an anxious, frightened young child is difficult, and documenting the degree of pain is not practical in a child who may not be able or willing to communicate effectively.<sup>[21] </sup><br><br> | <u>Palpation of the lower leg:</u> If there is a compartment syndrome, you can feel a firm, wooden feeling of the leg.<sup>[9]</sup><br><u>Children:</u> Identification of evolving CS in a child is difficult because of the child’s limited ability to communicate and anxiety about being examined by a stranger. Orthopedists are trained to look for the 5 P’s (pain, paresthesia, paralysis, pallor, pulselessness) associated with CS. Examining an anxious, frightened young child is difficult, and documenting the degree of pain is not practical in a child who may not be able or willing to communicate effectively.<sup>[21] </sup><br><br> | ||
== Medical Management <br> == | == Medical Management <br> == | ||
The gold standard treatment is fasciotomy, but most of the reports on its effectiveness are shown in short follow-up periods.<sup>[13]</sup>(Level of evidence 3) It is recommended that during surgical procedures all four compartments (anterior, lateral, deep posterior and superficial posterior) should be decompressed by one lateral incision or anterolateral and posteromedial incisions.<sup>[6]</sup>(Level of evidence 3) A few days after surgery patients may be able to participate in all common activities.<sup>[15]</sup>(Level of evidence 4) Treatment should begin with rest, icing (RICE), activity modification and sometimes nonsteroidal anti-inflammatory drugs.<br> | The gold standard treatment is fasciotomy, but most of the reports on its effectiveness are shown in short follow-up periods.<sup>[13]</sup>(Level of evidence 3) It is recommended that during surgical procedures all four compartments (anterior, lateral, deep posterior and superficial posterior) should be decompressed by one lateral incision or anterolateral and posteromedial incisions.<sup>[6]</sup>(Level of evidence 3) A few days after surgery patients may be able to participate in all common activities.<sup>[15]</sup>(Level of evidence 4) Treatment should begin with rest, icing (RICE), activity modification and sometimes nonsteroidal anti-inflammatory drugs.<br> | ||
== Physical Therapy Management <br> == | == Physical Therapy Management <br> == | ||
| Line 273: | Line 269: | ||
*Modifying your workplace to lower risk of injury | *Modifying your workplace to lower risk of injury | ||
</blockquote> | </blockquote> | ||
<br> '''How Can a Physical Therapist Help Before & After Surgery?'''<br>In the event that your case of compartment syndrome requires surgery (either due to an acute injury or chronic condition), postoperative physical therapy will be essential to a successful recovery. Your physical therapist will be in close communication with your surgeon regarding the nature of your procedure, expected timelines for healing, and your progress during rehabilitation. As a healthcare team, your providers will develop a plan to ensure your body has adequate time to heal, while incorporating strategies to restore your motion, mobility, strength, and function.<sup>[24]</sup>(Level of evidence 3)<br> | <br> '''How Can a Physical Therapist Help Before & After Surgery?'''<br>In the event that your case of compartment syndrome requires surgery (either due to an acute injury or chronic condition), postoperative physical therapy will be essential to a successful recovery. Your physical therapist will be in close communication with your surgeon regarding the nature of your procedure, expected timelines for healing, and your progress during rehabilitation. As a healthcare team, your providers will develop a plan to ensure your body has adequate time to heal, while incorporating strategies to restore your motion, mobility, strength, and function.<sup>[24]</sup>(Level of evidence 3)<br> | ||
== Key Research == | == Key Research == | ||
Matthew R., Daniel B., Laith M. and Andrew S. Chronic exertional compartment syndrome: diagnosis and management. BioMedSearch. (2005) Volume 62<br> | Matthew R., Daniel B., Laith M. and Andrew S. Chronic exertional compartment syndrome: diagnosis and management. BioMedSearch. (2005) Volume 62<br> | ||
== Resources <u></u><br> == | == Resources <u></u><br> == | ||
| Line 298: | Line 294: | ||
*http://www.physio-pedia.com/Compartment_Syndrome | *http://www.physio-pedia.com/Compartment_Syndrome | ||
</blockquote> | </blockquote> | ||
<br> <br><br> | <br> <br><br> | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Acute compartment syndrome (ACS) occurs when increased pressure within a compartment bounded by unyielding fascial membranes compromises the circulation and function of the tissues within that space. ACS is a surgical emergency.<sup>[14,25]</sup> | Acute compartment syndrome (ACS) occurs when increased pressure within a compartment bounded by unyielding fascial membranes compromises the circulation and function of the tissues within that space. ACS is a surgical emergency.<sup>[14,25]</sup> | ||
<blockquote> | <blockquote> | ||
*ACS most often develops soon after significant trauma, particularly involving long bone fractures of the lower leg or forearm. ACS may also occur following penetrating or minor trauma, or from nontraumatic causes, such as ischemia-reperfusion injury, coagulopathy, certain animal envenomations and bites, extravasation of IV fluids, injection of recreational drugs, and prolonged limb compression.<sup>[14,25]</sup> | *ACS most often develops soon after significant trauma, particularly involving long bone fractures of the lower leg or forearm. ACS may also occur following penetrating or minor trauma, or from nontraumatic causes, such as ischemia-reperfusion injury, coagulopathy, certain animal envenomations and bites, extravasation of IV fluids, injection of recreational drugs, and prolonged limb compression.<sup>[14,25]</sup> | ||
| Line 315: | Line 311: | ||
</blockquote><blockquote> | </blockquote><blockquote> | ||
*Immediate management of suspected ACS includes relieving all external pressure on the compartment. Any dressing, splint, cast, or other restrictive covering should be removed. The limb should be kept level with the torso, not elevated or lowered. Analgesics should be given and supplementary oxygen provided. Hypotension reduces perfusion and should be treated with intravenous boluses of isotonic saline.<sup>[14,25]</sup> | *Immediate management of suspected ACS includes relieving all external pressure on the compartment. Any dressing, splint, cast, or other restrictive covering should be removed. The limb should be kept level with the torso, not elevated or lowered. Analgesics should be given and supplementary oxygen provided. Hypotension reduces perfusion and should be treated with intravenous boluses of isotonic saline.<sup>[14,25]</sup> | ||
</blockquote> | </blockquote> | ||
Fasciotomy to fully decompress all involved compartments is the definitive treatment for ACS in the great majority of cases. Delays in performing fasciotomy increase morbidity.<sup>[14,25]</sup><br><br> | Fasciotomy to fully decompress all involved compartments is the definitive treatment for ACS in the great majority of cases. Delays in performing fasciotomy increase morbidity.<sup>[14,25]</sup><br><br> | ||
<u>Chronic exertional compartment syndrome (CECS) </u> <br>In patients with clinical symptoms of CECS and confirmation of elevated exertional compartment pressures, operative treatment demonstrated improved clinical outcomes compared with conservative treatment. High school and college patient's (age \23 years) and isolated anterior compartment release (compared with anterior/lateral release) were factors associated with improved subjective function and satisfaction after fasciotomy. Based on these results, high school– and college-aged patients with isolated anterior compartment release would be expected to have the best outcome from fasciotomy. We recommend the avoidance of lateral release unless clearly warranted.<sup>[16]</sup> | <u>Chronic exertional compartment syndrome (CECS) </u> <br>In patients with clinical symptoms of CECS and confirmation of elevated exertional compartment pressures, operative treatment demonstrated improved clinical outcomes compared with conservative treatment. High school and college patient's (age \23 years) and isolated anterior compartment release (compared with anterior/lateral release) were factors associated with improved subjective function and satisfaction after fasciotomy. Based on these results, high school– and college-aged patients with isolated anterior compartment release would be expected to have the best outcome from fasciotomy. We recommend the avoidance of lateral release unless clearly warranted.<sup>[16]</sup> | ||
<u></u> | <u></u> | ||
<u>Compartment Syndrome in children</u> <br>Increased need for analgesics is often the first sign of CS in children and should be considered the sentinel alarm for ongoing tissue necrosis. CS remains a clinical diagnosis, and compartment pressure should be measured only as a confirmatory test in noncommunicative patients or when the diagnosis is unclear. Children with supracondylar humeral fractures, forearm fractures, tibial fractures, and medical risk factors for coagulopathy are at increased risk and should be monitored closely. When the diagnosis is made promptly and the condition is treated with fasciotomy, good long-term clinical results can be expected.<sup>[21] </sup><br> | <u>Compartment Syndrome in children</u> <br>Increased need for analgesics is often the first sign of CS in children and should be considered the sentinel alarm for ongoing tissue necrosis. CS remains a clinical diagnosis, and compartment pressure should be measured only as a confirmatory test in noncommunicative patients or when the diagnosis is unclear. Children with supracondylar humeral fractures, forearm fractures, tibial fractures, and medical risk factors for coagulopathy are at increased risk and should be monitored closely. When the diagnosis is made promptly and the condition is treated with fasciotomy, good long-term clinical results can be expected.<sup>[21] </sup><br> | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
| Line 372: | Line 368: | ||
25. http://www.uptodate.com/contents/acute-compartment-syndrome-of-the-extremities#H18<br><br> | 25. http://www.uptodate.com/contents/acute-compartment-syndrome-of-the-extremities#H18<br><br> | ||
[[Category:Vrije_Universiteit_Brussel_Project | [[Category:Vrije_Universiteit_Brussel_Project]][[Category:Sports_Injuries]][[Category:Foot_and_Ankle_Conditions]] | ||
Revision as of 12:33, 29 March 2017
Original Editors - Geoffrey De Vos
Top Contributors - Delmoitie Giovanni, Scott Cornish, Geoffrey De Vos, Admin, Lucinda hampton, Kim Jackson, Glenn-Gerlo, Bettina Vansintjan, WikiSysop, Fasuba Ayobami, Karen Wilson, Wanda van Niekerk and Naomi O'Reilly
Definition/Description[edit | edit source]
Compartment syndrome of the lower leg has been defined as a condition which increased the pressure in a small place. This compromises the circulation and function of the tissues within that space. It is most commonly seen after injuries to the leg and forearm, but also occur in the arm, thigh, foot, buttock, hand and abdomen.[4] This condition ensures that there will be compression on nervers, blood vessels and muscle(s) inside the compartment of the lower leg.[2,3,4]
This injury may lead to tissue death (necrosis) due to the blood vessels being compressed by the raised pressure within the compartment. So this compression causes an ischemia, a lack of oxygen, that can result in serious and dangerous tissue damages or tissue death when this injury isn’t treated well. In the literature the speak about three types of compartment syndrome. It can be divided into acute (ACS) , subacute, and chronic compartment syndrome (CECS).[1]
Acute compartment syndrome (ACS) is caused by bleeding or oedema in a closed, non-elastic muscle compartment which is surrounded by fascia and bone. Among the most common causes of this complication are fractures, blunt trauma and reperfusion injury after acute arterial obstruction. Increasing intracompartmental pressure may lead to nerve damage and reduced tissue perfusion resulting in muscle ischaemia or necrosis mediated by infiltrating neutrophils.[6]
Chronic compartment syndrome (CCS) is is a common injury in young athletes, causing pain in the involved leg compartment during strenuous exercise.[10,11] It is clinically manifest by recurrent episodes of muscle cramping, tightness, and occasional paresthesias.[13] Also their is an increase of pressure in skeletal muscle accompanied by pain, swelling, and impaired muscle function. Unlike other exertional injuries such as stress fracture, periostitis, or tendonitis, this problem does not respond to antiinflammatory medications or physical therapy.[10,11]
This syndrome occurs fairly regularly and occurs in most of the times in athletes, such as long distance runners, soccer players, basketball players and military men and women.[7,13] It can also occur in children, adolescents or adults, but more often in adults.[2,3]
Clinically Relevant Anatomy[edit | edit source]
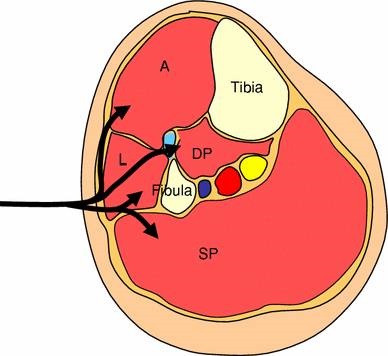
In the lower leg, they speak about four compartments.
So as you can see on the picture, we have the anterior (A), lateral (L), deep posterior (DP) and superficial posterior (SP). The bones of the lower leg (tibia and fibula), the interosseous membrane and the anterior intermuscular septum are the borders of the compartments. The anterior compartment include M. tibialis anterior, M. ext. hallucis longus, M. ext. digitorum longus, M. peroneus tertius, A. tibialis anterior and the deep peroneal nerve.
The lateral compartment include M. peroneus longus and brevis and also the N. superficial peroneal. The deep posterior compartment include M. tibialis posterior, M. flex. hallucis longus, M. flex. digitorum longus, M. popliteus, A. tibialis posterior and the N. tibialis. The superficial posterior compartment include the M. gastrocnemius, M. soleus, M. plantaris and N. sural. 1All this compartments are surrounded by fascia. This fascia is connected to bone and each of them has a blood and nerve supply. These fascias do not expand and when a compartment swells the pressure inside the compartment will increase which will cause tissue necrosis due by the compressing of blood vessels and nerves.[9,19]
Picture: http://www.clinorthop.org/volume/468/issue/4
Epidemiology /Etiology[edit | edit source]
The average annual incidence of ACS for men are 7.3 per 100.000 and by women 0.7 per 100.000. To most of the patients are young men with fractures of the tibial diaphysis, with a injury to the soft tissues or those with a bleeding diathesis. Any condition that results in an increase of pressure in a compartment can lead to the development of an acute (ACS) or chronic exertional compartment syndrome (CECS).
In most of the times ACS occurs after: [8,9]
- Fracture of the tibial diaphysis
- Soft-tissue injury
- Intensive muscle use
- Everyday extreme exercise activities
- Arterial injury
- Drug overdose
- Burns
One of the main causes of CECS is repetitive and strenuous exercise (sports). During strenuous exercise, there can be up to a 20% increase in muscle volume and weight due to increased blood flow and oedema, so the pressure increases.[2] Oedema of the soft tissue within the compartment further raises the intra-compartment pressure, which compromises venous and lymphatic drainage of the injured area. If the pressure further increases, it will eventually turn into a vicious circle, that can lead to tissue ischemia. The normal mean interstitial tissue pressure in relaxed muscles is ± 10-12 mmHg. If this pressure elevates to 30 mmHg or more, small vessels in the tissue become compressed, which leads to reduced nutrient blood flow, ischemia and pain.[1,2] The anterior compartment is affected more frequently than the lateral, deep and superficial posterior compartments.[7]
Characteristics/Clinical Presentation[edit | edit source]
Patients with compartment syndrome of the lower leg suffer from long term impairment such as reduced muscular strength, reduced range of motion and pain.[6]
The most common symptoms by a compartment syndrome are:[9]
- Feeling of tightness
- Swelling
- Pain (by active flexion knee and particularly passive stretching of the muscles)
- Paresthesia
Pain and swelling are the leading symptoms in this disease and it appears and aggravates during physical activities such as running and other sports like basketball and soccer. The pain is usually located over
the involved compartments and may radiate to the ankle or foot. Burning, cramping, or aching pain and tightness develop while exercising. In extreme cases (no or bad treatment) it is possible that the lower leg, ankle and foot can be paralysed.[2] (C Reid D. et al)
Differential Diagnosis[edit | edit source]
Patients with exercise-induced lower leg pain, differential diagnosis includes: medial tibial stress syndrome (MTSS), fibular and tibial stress fractures, fascial defects, nerve entrapment syndromes, vascular claudication and lumbar disc herniation.[2]
Pain:
Pain is classically the first sign of the development of ACS, is ischaemic in nature, and is described as being out of proportion to the clinical situation. There are a number of problems with this symptom, not least of which is the subjective nature of the severity of pain with psychosocial factors such as anxiety, heightened concern about illness, beliefs, and expectations influencing pain intensity in patients with disabling musculoskeletal pain. Pain may be an unreliable indication of the presence of ACS because it can be variable in its intensity. It may be absent in ACS associated with nerve injury, or minimal in the deep posterior compartment syndrome, and cannot be elicited in the unconscious patient or where regional anaesthesia is used. Children or patients with learning disabilities may not be able to express the severity of their pain, so restlessness, agitation, and anxiety with increasing analgesic requirements should raise the suspicion of the presence of ACS. Increasing requirements for opiates in all patients should also be considered in assessing the severity of pain.
The sensitivity of pain in the diagnosis of ACS is only 19 % with a specificity of 97 %, which results in a high proportion of false-negative or missed cases but a low proportion of false-positive cases, but if present it is recognised as a relatively early symptom of ACS in the awake alert patient.
Pain with passive stretch is assessed by stretching the affected muscle group. For example, if ACS is suspected in the deep posterior compartment of the leg and the foot is dorsiflexed, increased pain should be evident.
Neurological symptoms and signs:
Paraesthesia and hypoesthesia may occur in the territory of the nerves traversing the affected compartment and are usually the first signs of nerve ischaemia, although sensory abnormality may be the result of concomitant nerve injury. Ulmer reports a sensitivity of 13 % and specificity of 98 % for the clinical finding of paraesthesia in ACS, a false-negative rate that precludes this symptom from being a useful diagnostic tool.
Paralysis of muscles contained in the affected compartments is recognised as being a late sign and has equally low sensitivity as others in predicting the presence of ACS, probably because of the difficulty in interpreting the underlying cause of the weakness, which could be inhibition by pain, direct injury to muscle, or associated nerve injury.
Swelling:
Swelling in the compartment affected can be a sign of ACS, although the degree of swelling is difficult to assess accurately, making this sign very subjective. The compartment may be obscured by casts, dressing, or other muscle groups, for example in the case of the deep posterior compartment. Poor sensitivity, specificity, and negative and positive predictive values have been demonstrated when manual palpation was used to determine whether ICP was raised in cadaveric limbs.
Diagnostic Procedures[edit | edit source]
A precise diagnosis of chronic exertional compartment syndrome can generally be made with a high degree of clinical suspicion, a careful history, a full physical examination, and compartment pressure testing, bone scanning, or both.[12]
ACS:
Patient history and physical examination play an important role in diagnosing ACS. In some cases are history and physical examination insufficient to arrive at a correct diagnosis. In these cases and in other situations where it is impossible to elicit a reliable history or to do a physical examination (lack of consciousness/coma, intoxication, little children, etc.), intra-compartmental pressure can offer a solution. The normal pressure in a muscle compartment is between 10-12 mm Hg.[1]
- Upon inspection, the primary finding is swelling of the affected extremity
- The inability to actively move flexors and extensors of the foot is an important indicator [1]
- Signs such as progression of pain complaints
- Pain with passive stretching of the affected muscles
- Often a sensation disturbance in the web space between the first and second toes is found as a consequence of compression or ischemia of the deep peroneal nerve. This nerve is found in the anterior compartment; reduced sensibility represents a late sign of the ACS
- Absence of arterial pulsations is more often a sign of arterial injury than a very late sign of the ACS
CECS:
- Pain starts within first 30 minutes of exercise and can radiate to ankle/foot [2]
- Pain ceases when activity is stopped
- Daily activities usually not provocative
- Upon inspection, the primary finding is swelling of the affected extremity
- The inability to actively move flexors and extensors of the foot is an important indicator
- Signs such as progression of pain complaints
- Recording of intra-compartmental tissue pressures[2,22] (needle and manometer, wick catheter, slit catheter):
- A pre-exercise pressure of ≥ 15 mmHg
- 1 minute post-exercise pressure of ≥ 30 mmHg
- 5 minute post-exercise pressure of ≥ 20 mmHg
- MRI:
- More studies are needed to define threshold values for the diagnosis of CECS
- MRI may emerge as a noninvasive alternative to detecting elevated compartment tissue pressures[2]
By recognizing these signs in a timely fashion, it is possible to identify an ACS en CECS early, so that the treatment can be started immediately.
Reported sensitivities and specificities of the clinical symptoms and signs of ACS:
|
Sympton or sign |
Particular features | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) |
|
Pain |
Out of proportion to the clinical situation |
19 |
97 |
14 |
98 |
|
Stretch pain |
Increased pain on stretching the affected muscles |
19 |
97 |
14 |
98 |
|
Sensory changes |
Paraesthesia or numbness |
13 |
98 |
15 |
98 |
|
Motor changes |
Weakness or paralysis of affected muscle groups |
13 |
97 |
11 |
98 |
|
Swelling |
Assessed by manual palpation |
54 |
76 |
70 |
63 |
Outcome Measures[edit | edit source]
The most important determinant of a poor outcome from acute compartment syndrome after injury is delay in diagnosis. The complications are usually disabling and include infection, contracture and amputation. One of the main causes of delay may be insufficient awareness of the condition. While it is acknowledged that children, because of difficulty in assessment, and hypotensive patients are at risk, most adults who develop acute compartment syndrome are not hypotensive. Awareness of the risk of the syndrome may reduce delay in diagnosis. Continuous monitoring of compartment pressure may allow the diagnosis to be made earlier and complications to be minimised.
Early diagnosis and treatment are of the utmost importance in order to avoid long-term disability after acute compartment syndrome.[8]
Examination[edit | edit source]
Palpation of the lower leg: If there is a compartment syndrome, you can feel a firm, wooden feeling of the leg.[9]
Children: Identification of evolving CS in a child is difficult because of the child’s limited ability to communicate and anxiety about being examined by a stranger. Orthopedists are trained to look for the 5 P’s (pain, paresthesia, paralysis, pallor, pulselessness) associated with CS. Examining an anxious, frightened young child is difficult, and documenting the degree of pain is not practical in a child who may not be able or willing to communicate effectively.[21]
Medical Management
[edit | edit source]
The gold standard treatment is fasciotomy, but most of the reports on its effectiveness are shown in short follow-up periods.[13](Level of evidence 3) It is recommended that during surgical procedures all four compartments (anterior, lateral, deep posterior and superficial posterior) should be decompressed by one lateral incision or anterolateral and posteromedial incisions.[6](Level of evidence 3) A few days after surgery patients may be able to participate in all common activities.[15](Level of evidence 4) Treatment should begin with rest, icing (RICE), activity modification and sometimes nonsteroidal anti-inflammatory drugs.
Physical Therapy Management
[edit | edit source]
The only nonoperative treatment that is certain to alleviate the pain of CECS is the cessation of causative activities. The patient should continue his normal physical activities, to the limit that the pain allows it, so lower intensity of frequency of exercising (activity modification). Unfortunately, this is an unappealing option for the competitive and recreational athlete. Cycling may be substituted for running in patients who wish to maintain their cardiorespiratory fitness, as it is associated with a lower risk of compartment pressure elevation. Massage therapy may provide some benefit to patients with mild symptoms or to those who decline surgical intervention. Overall, however, nonoperative treatment has been generally unsuccessful.[2]( Level of evidence 2)
The symptoms will not disappear without treatment. Untreated compartment syndrome can cause ischemia of the muscles and nerves and can eventually lead to irreversible damage like tissue death, muscle necrosis and permanent neurological deficit within the compartment.
The only treatment that’s effective in this disease is surgical treatment, more specifically a fasciotomy. A little incision will be made in the lower leg (one of the compartments) to decrease the intra compartment pressure and eventually the symptoms will disappear and most of the patients recover well.[2](M Béuima M. et al) ( Level of evidence 2)
Most patients suffering from muscular pain of uncertain origin are advised to increase their physical training to achieve pain relief. However, patients with Chronic Compartment Syndrome (CCS) may experience both increase in pain in the legs and increase in referred muscular pain, the latter of uncertain aetiology. Children and adults alike may become unable to participate in common physical activities down to walking to school, resulting in isolation and depression.[15](Level of evidence 4)
Physical Therapy in CECS
Conservative therapy has been attempted for CECS, but it is generally unsuccessful. Symptoms typically recur once the patient returns to exercise. Discontinuing participation in sports is an option, but it is a choice that most athletes refuse.[17,23](Level of evidence, 4)
- Conservative therapy
Conservative treatment of CECS mainly involves a decrease in activity or load to the affected compartment. The activity level gradually is increased, depending on the patient’s symptoms. Aquatic exercises, such as running in water, can improve mobility and strength without unnecessarily loading the affected compartment. Massage and stretching exercises also have been shown to be effective, according to Hutchinson and Ireland.[17,23](Level of evidence 4)
Massage therapy can also help by patients with mild symptoms or people who declined surgical intervention. The patients are able to do more exercise without pain.[19](Level of evidence 4)
Nonoperative therapy is aimed at obtaining or preserving joint mobility.[20](Level of evidence 4)
- Presurgical therapy
Presurgical therapy in CECS includes reduction of activity, with encouragement of cross-training exercises (eg, swimming, bicycling, other low-impact activities) and muscle stretching before initiating exercise. This approach may also be helpful for primary prevention of CECS, although only limited information is available on this topic. Other preoperative measures are rest, shoe modification, and the use of nonsteroidal anti-inflammatory medications (NSAIDs) to reduce inflammation. It is recommended to avoid casting, splinting, or compression of the affected limb.[17,23](Level of evidence 4)
- Postsurgical therapy
Postsurgical therapy for CECS includes assisted weight bearing with some variation, depending on surgical technique. Some physicians recommend immediate postsurgical range-of-motion activity that may include walking (unaided by 3-5 d). Early mobilization as soon as is feasible is recommended by many surgeons to minimize scarring, which can lead to adhesions and a recurrence of the syndrome.
Activity can be upgraded to stationary cycling and swimming after healing of the surgical wounds. Isokinetic muscle strengthening exercises can begin at 3-4 weeks. Running is integrated into the activity program at 3-6 weeks. Full activity is introduced at approximately 6-12 weeks, with a focus on speed and agility.[17,23](Level of evidence 4)
How Can a Physical Therapist Help?
If you are diagnosed with compartment syndrome, your physical therapist will play an important role in the treatment of the condition, whether it requires surgery or not. Your physical therapist will work with you to design an individualized treatment program based on your condition and your personal goals. Your physical therapist may recommend:[24](Level of evidence 3)
- Range-of-Motion Exercises. Restrictions in the motion of your knee, foot, or ankle may be causing increased strain in the muscles housed within the compartments of your lower leg. Stretching techniques can be used to help restore motion in these joints to minimize undue muscle tension.[24](Level of evidence 3)
- Muscle Strengthening. Hip and core weakness can influence how your lower body moves, and can cause imbalanced forces through the lower-leg muscle groups that may contribute to compartment syndrome. Building core strength (in the muscles of the abdomen, low back, and pelvis) is important; a strong midsection allows greater stability through the body as the arms and legs perform different motions. For athletes engaged in endurance sports, it is important to have a strong core to stabilize the hip and knee joints during repetitive leg motions. Your physical therapist will be able to determine which muscles are weak, and provide specific exercises to target these areas.[24](Level of evidence 3)
- Manual Therapy. Many physical therapists are trained in manual (hands-on) therapy, using their hands to move and manipulate muscles and joints to improve motion and strength. These techniques can target areas that are difficult to treat on your own.[24](Level of evidence 3)
- Modalities. Your physical therapist may use modalities ( e.g., ultrasound, iontophoresis, moist heat, cold therapy) as a part of your rehabilitation program. These tools can help improve tissue mobility and flexibility, and enhance recovery. Your physical therapist will discuss the purpose of each modality with you.[24](Level of evidence 3)
- Education. Your treatment will include education about how to safely return to your previous activities, particularly if your condition required a fasciotomy. Your physical therapist may recommend:[24] Level of evidence 3)
- Wearing more appropriate footwear
- Choosing more appropriate surfaces and terrain for exercise
- Pacing your activities
- Avoiding certain activities altogether
- Mastering strategies for recovery and maintenance of good health (e.g., allowing your muscles and joints proper rest time)
- Modifying your workplace to lower risk of injury
How Can a Physical Therapist Help Before & After Surgery?
In the event that your case of compartment syndrome requires surgery (either due to an acute injury or chronic condition), postoperative physical therapy will be essential to a successful recovery. Your physical therapist will be in close communication with your surgeon regarding the nature of your procedure, expected timelines for healing, and your progress during rehabilitation. As a healthcare team, your providers will develop a plan to ensure your body has adequate time to heal, while incorporating strategies to restore your motion, mobility, strength, and function.[24](Level of evidence 3)
Key Research[edit | edit source]
Matthew R., Daniel B., Laith M. and Andrew S. Chronic exertional compartment syndrome: diagnosis and management. BioMedSearch. (2005) Volume 62
Resources
[edit | edit source]
Literature:
- M Béuima M., Bojanic I.. Overuse injuries of the musculoskeletal system. CRC press,
- C Reid D.. Sports injuries assessment and rehabilitation. Churchill Livingstone USA, 1992
Books:
- Schünke M., Schulte E., Schumacher U., Voll M. and Wesker K. Prometheus: Algemene anatomie en bewegingsapparaat. Bohn Stafleu van Longhum Houten, 2010
Websites:
Clinical Bottom Line[edit | edit source]
Acute compartment syndrome (ACS) occurs when increased pressure within a compartment bounded by unyielding fascial membranes compromises the circulation and function of the tissues within that space. ACS is a surgical emergency.[14,25]
- ACS most often develops soon after significant trauma, particularly involving long bone fractures of the lower leg or forearm. ACS may also occur following penetrating or minor trauma, or from nontraumatic causes, such as ischemia-reperfusion injury, coagulopathy, certain animal envenomations and bites, extravasation of IV fluids, injection of recreational drugs, and prolonged limb compression.[14,25]
- The accuracy of the physical examination for diagnosing ACS is limited. Early symptoms of ACS include progressive pain out of proportion to the injury; signs include tense swollen compartments and pain with passive stretching of muscles within the affected compartment. Important clues to the development of ACS include rapid progression of symptoms and signs over a few hours and the presence of multiple findings consistent with the diagnosis in a patient at risk. Close observation and serial examinations in patients at risk for ACS are of great importance. Motor deficits are LATE findings associated with irreversible muscle and nerve damage.[14,25]
- Immediate surgical consultation should be obtained whenever ACS is suspected based upon the patient's risk factors and clinical findings. Whenever possible, the surgeon should determine the need for measuring compartment pressures, which can aid diagnosis. A single normal compartment pressure reading, which may be performed early in the course of the disease, does NOT rule out ACS. Serial or continuous measurements are important when patient risk is moderate to high or clinical suspicion persists.[14,25]
- The normal pressure of a tissue compartment falls between 0 and 8 mmHg. Signs of ACS develop as tissue pressure rises and approaches systemic pressure. However, the pressure necessary for injury varies. Higher pressures may be necessary before injury occurs to peripheral nerves in patients with systemic hypertension, while ACS may develop at lower pressures in those with hypotension or peripheral vascular disease.[14,25]
- When interpreting compartment pressure measurements in patients with clinical findings suggestive of ACS, we suggest using a difference between the diastolic blood pressure and the compartment pressure of 30 mmHg or less as the threshold for an elevated compartment pressure.[14,25]
- Immediate management of suspected ACS includes relieving all external pressure on the compartment. Any dressing, splint, cast, or other restrictive covering should be removed. The limb should be kept level with the torso, not elevated or lowered. Analgesics should be given and supplementary oxygen provided. Hypotension reduces perfusion and should be treated with intravenous boluses of isotonic saline.[14,25]
Fasciotomy to fully decompress all involved compartments is the definitive treatment for ACS in the great majority of cases. Delays in performing fasciotomy increase morbidity.[14,25]
Chronic exertional compartment syndrome (CECS)
In patients with clinical symptoms of CECS and confirmation of elevated exertional compartment pressures, operative treatment demonstrated improved clinical outcomes compared with conservative treatment. High school and college patient's (age \23 years) and isolated anterior compartment release (compared with anterior/lateral release) were factors associated with improved subjective function and satisfaction after fasciotomy. Based on these results, high school– and college-aged patients with isolated anterior compartment release would be expected to have the best outcome from fasciotomy. We recommend the avoidance of lateral release unless clearly warranted.[16]
Compartment Syndrome in children
Increased need for analgesics is often the first sign of CS in children and should be considered the sentinel alarm for ongoing tissue necrosis. CS remains a clinical diagnosis, and compartment pressure should be measured only as a confirmatory test in noncommunicative patients or when the diagnosis is unclear. Children with supracondylar humeral fractures, forearm fractures, tibial fractures, and medical risk factors for coagulopathy are at increased risk and should be monitored closely. When the diagnosis is made promptly and the condition is treated with fasciotomy, good long-term clinical results can be expected.[21]
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
- Oprel PP., Eversdij MG., Vlot J., Tuinebreijer WE. The Acute Compartment Syndrome of the Lower Leg: A Difficult Diagnosis? Department of Surgery-Traumatology and Pediatric Surgery, Erasmus MC, University Medical Center Rotterdam, The Open Orthopaedics Journal, 2010, 4, 115-119 (Level of evidence 1)
- Bong MR., Polatsch DB., Jazrawi LM., Rokit AS. Chronic Exertional Compartment Syndrome, Diagnosis and Management. Hospital for Joint Diseases 2005, Volume 62, Numbers 3 & 4 (Level of evidence 2)
- Rorabeck CH. The treatment of compartment syndromes of the leg. Division of Orthopaedic Surgery, University Hospital, London, Ontario, Canada, © 1984 British Editorial Society of Bone and Joint Surgery vol. 66-b (Level of evidence 2)
- Kirsten G.B, Elliot A, Jonhstone J. Diagnosing acute compartment syndrome. Journal of bone and joint surgery (Br) 2003. Volume 85, Number 5, 625-632
- Frink M., Hildebrand F., Krettek C., Brand J., Hankenmeier C. Compartment Syndrome of the lower leg and Foot. Clinical Orthopaedics and Related Research. 2010, 4, 940-950.
- Frink, Michael, et al. "Long term results of compartment syndrome of the lower limb in polytraumatised patients." Injury 38.5 (2007): 607-613. (Level of evidence 3)
- Van der Wal, W. A., et al. "The natural course of chronic exertional compartment syndrome of the lower leg." Knee Surgery, Sports Traumatology, Arthroscopy 23.7 (2015): 2136-2141.
- McQueen, M. M., and P. Gaston. "Acute compartment syndrome." Bone & Joint Journal 82.2 (2000): 200-203.
- Abraham TR. Acute Compartment Syndrome. Physical Medicine and Rehabilitation. (2016)
- Turnipseed, William D., Christof Hurschler, and Ray Vanderby. "The effects of elevated compartment pressure on tibial arteriovenous flow and relationship of mechanical and biochemical characteristics of fascia to genesis of chronic anterior compartment syndrome." Journal of vascular surgery 21.5 (1995): 810-817.
- Styf, Jorma R., and Lars M. Körner. "Diagnosis of chronic anterior compartment syndrome in the lower leg." Acta orthopaedica Scandinavica 58.2 (1987): 139-144.
- Slimmon, Drew, et al. "Long-term outcome of fasciotomy with partial fasciectomy for chronic exertional compartment syndrome of the lower leg." The American Journal of Sports Medicine 30.4 (2002): 581-588.
- Chechik, O., G. Rachevsky, and G. Morag. "Michael Drexler, T. Frenkel Rutenberg, N. Rozen, Y. Warschawski, E. Rath." (Level of evidence 3)
- Andrea Stracciolini MD , E. Mark Hammerberg MD, Maria E Moreira, MD Richard G Bachur, MD Jonathan Grayzel, MD, FAAEM Acute compartment syndrome of the extremities
- Orlin, Jan Roar, et al. "Prevalence of chronic compartment syndrome of the legs: Implications for clinical diagnostic criteria and therapy." Scandinavian Journal of Pain 12 (2016): 7-12. (Level of evidence 4)
- Am J Sports Med. 2013 Feb;41(2):430-6. doi: 10.1177/0363546512471330. Functional outcomes and patient satisfaction after fasciotomy for chronic exertional compartment syndrome. Packer JD1, Day MS, Nguyen JT, Hobart SJ, Hannafin JA, Metzl JD.
- Gregory A Rowdon, MD; Chief Editor: Craig C Young, MD more… Chronic Exertional Compartment Syndrome Treatment & Management Updated: Oct 08, 2015
- The diagnosis of acute compartment syndrome: a review - By:McQueen, MM (McQueen, M. M.)[ 1 ] ; Duckworth, AD (Duckworth, A. D.)
- Blackman PG, Simmons LR, Crossley KM: Treatment of chronic exertional anterior compartment syndrome with massage: a pilot study. Clin J Sport Med 1998;8:14-7. (Level of evidence: 4)
- Wiegand, N., et al. "Differential scanning calorimetric examination of the human skeletal muscle in a compartment syndrome of the lower extremities." Journal of thermal analysis and calorimetry 98.1 (2009): 177-182. (Level of evidence 4)
- Am J Orthop. Pooya Hosseinzadeh, MD, and Vishwas R. Talwalkar, MD 2016 January;45(1):19-22 Compartment Syndrome in Children: Diagnosis and Management
- Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH: Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med 1990;18:35-40.
- http://emedicine.medscape.com/article/88014-treatment#d10 (Level of evidence 4)
- 17. Gregory A Rowdon, MD; Chief Editor: Craig C Young, MD more… Chronic Exertional Compartment Syndrome Treatment & Management Updated: Oct 08, 2015
- Hutchinson MR1, Ireland ML. “Common compartment syndromes in athletes. Treatment and rehabilitation” Sports Med. 1994 Mar;17(3):200-8.
- Wittstein J1, Moorman CT 3rd, Levin LS. “Endoscopic compartment release for chronic exertional compartment syndrome: surgical technique and results.” Am J Sports Med. 2010 Aug (Level of evidence 4)
24. http://www.moveforwardpt.com/symptomsconditionsdetail.aspx?cid=a373249d-d523-4eb7-90b0-b252f164f405
- Davis DE1, Raikin S, Garras DN, Vitanzo P, Labrador H, Espandar R. “Characteristics of patients with chronic exertional compartment syndrome.” Foot Ankle Int. 2013 Oct;34(10):1349-54. doi: 10.1177/1071100713490919. Epub 2013 May 13. (Level of evidence 3)
- Val Irion, Robert A. Magnussen, Timothy L. Miller , Christopher C. Kaeding “Return to activity following fasciotomy for chronic exertional compartment syndrome” Eur J Orthop Surg Traumatol (2014) (Level of evidence 3)
25. http://www.uptodate.com/contents/acute-compartment-syndrome-of-the-extremities#H18