Classification of Peripheral Nerve Injury: Difference between revisions
Emma Sewell (talk | contribs) (Added references) |
(added to MOI) |
||
| Line 10: | Line 10: | ||
Peripheral nerves are responsible for somatic (voluntary) and autonomic (involuntary) functions. The primary functions of the peripheral nervous system are to receive general sensations (touch, pressure, temperature, and pain), and special sensations (sight, smell, taste, and hearing), integrate sensory input from the entire body, and generate a response<ref>Radhakrishnan, R. What are the 4 main functions of the nervous system? Available from <nowiki>https://www.medicinenet.com/4_main_functions_of_the_nervous_system/article.htm</nowiki> (Accessed 18 March 2023).</ref>. Peripheral Nerve Injury can be sustained from traumatic or idiopathic mechanisms. Individuals with diagnoses of diabetes, alcoholism, vascular disease, autoimmune diseases, or who have been exposed to chemotherapy drugs or infections that attack nerves have a higher likelihood of acquired peripheral neuropathy<ref name=":0">National Institute of Neurological Disorders and Stroke. Peripheral neuropathy. Available from <nowiki>https://www.ninds.nih.gov/health-information/disorders/peripheral-neuropathy</nowiki> (Accessed 18 May 2023).</ref>. The severity of peripheral nerve injury is determined with advanced imaging (CT, MRI, or MRI neurography) or nerve conduction velocity testing and classified using the Sunderland classification system<ref name=":0" />. Treatment of peripheral nerve damage depends on the severity of the damage and may include surgical procedures, skilled physical therapy, orthotics, or medications<ref>Johns Hopkins Medicine. Peripheral Nerve Injury. Available from <nowiki>https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-nerve-injury</nowiki> (Accessed 18 March 2023).</ref> .There are three basic types of peripheral nerve injuries (PNI) commonly seen in the clinic: stretch related, lacerations, and compressions<ref name="burn">Burnett MG, Zager EL. Pathophysiology of peripheral nerve injury: a brief review. Neurosurgical focus. 2004 May;16(5):1-7.</ref>. | Peripheral nerves are responsible for somatic (voluntary) and autonomic (involuntary) functions. The primary functions of the peripheral nervous system are to receive general sensations (touch, pressure, temperature, and pain), and special sensations (sight, smell, taste, and hearing), integrate sensory input from the entire body, and generate a response<ref>Radhakrishnan, R. What are the 4 main functions of the nervous system? Available from <nowiki>https://www.medicinenet.com/4_main_functions_of_the_nervous_system/article.htm</nowiki> (Accessed 18 March 2023).</ref>. Peripheral Nerve Injury can be sustained from traumatic or idiopathic mechanisms. Individuals with diagnoses of diabetes, alcoholism, vascular disease, autoimmune diseases, or who have been exposed to chemotherapy drugs or infections that attack nerves have a higher likelihood of acquired peripheral neuropathy<ref name=":0">National Institute of Neurological Disorders and Stroke. Peripheral neuropathy. Available from <nowiki>https://www.ninds.nih.gov/health-information/disorders/peripheral-neuropathy</nowiki> (Accessed 18 May 2023).</ref>. The severity of peripheral nerve injury is determined with advanced imaging (CT, MRI, or MRI neurography) or nerve conduction velocity testing and classified using the Sunderland classification system<ref name=":0" />. Treatment of peripheral nerve damage depends on the severity of the damage and may include surgical procedures, skilled physical therapy, orthotics, or medications<ref>Johns Hopkins Medicine. Peripheral Nerve Injury. Available from <nowiki>https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-nerve-injury</nowiki> (Accessed 18 March 2023).</ref> .There are three basic types of peripheral nerve injuries (PNI) commonly seen in the clinic: stretch related, lacerations, and compressions<ref name="burn">Burnett MG, Zager EL. Pathophysiology of peripheral nerve injury: a brief review. Neurosurgical focus. 2004 May;16(5):1-7.</ref>. | ||
=== ''' | === '''Mechanism of Injury for Peripheral Nerves''' === | ||
The peripheral nerves are | The three most common mechanisms of injury for peripheral nerves are stretch related, lacerations, and compressions. The most common of these three is stretch-related, followed by lacerations, and then compression<ref name="camp">Campbell WW. Evaluation and management of peripheral nerve injury. Clinical neurophysiology. 2008 Sep 30;119(9):1951-65.</ref>. | ||
=== '''Lacerations''' === | ==== Stretch Related ==== | ||
Due to the elastic nature of peripheral nerves, stretch related injuries can occur if a traction force is too strong for the nerves elasticity. If the traction force exceeds the nerves stretch abilities, a complete tear could occur. However, it is more common that the continuity of the nerve is retained during this type of injury.<ref name="burn" /> | |||
===='''Lacerations'''==== | |||
Another common type of PNI are lacerations created by blades. those types of injuries might be complete transections- but most commonly some continuity remains. | Another common type of PNI are lacerations created by blades. those types of injuries might be complete transections- but most commonly some continuity remains. | ||
=== '''Compressions''' === | ===='''Compressions'''==== | ||
The third type of PNI are compression These injuries include the Saturday Night palsy due to radial nerve compression as well as entrapment neuropathies and do not involve tearing of the neural elements<ref name="burn" />. | The third type of PNI are compression These injuries include the Saturday Night palsy due to radial nerve compression as well as entrapment neuropathies and do not involve tearing of the neural elements<ref name="burn" />. | ||
== Classification == | == Classification == | ||
Revision as of 20:36, 30 March 2023
Description[edit | edit source]
Peripheral nerves are responsible for somatic (voluntary) and autonomic (involuntary) functions. The primary functions of the peripheral nervous system are to receive general sensations (touch, pressure, temperature, and pain), and special sensations (sight, smell, taste, and hearing), integrate sensory input from the entire body, and generate a response[1]. Peripheral Nerve Injury can be sustained from traumatic or idiopathic mechanisms. Individuals with diagnoses of diabetes, alcoholism, vascular disease, autoimmune diseases, or who have been exposed to chemotherapy drugs or infections that attack nerves have a higher likelihood of acquired peripheral neuropathy[2]. The severity of peripheral nerve injury is determined with advanced imaging (CT, MRI, or MRI neurography) or nerve conduction velocity testing and classified using the Sunderland classification system[2]. Treatment of peripheral nerve damage depends on the severity of the damage and may include surgical procedures, skilled physical therapy, orthotics, or medications[3] .There are three basic types of peripheral nerve injuries (PNI) commonly seen in the clinic: stretch related, lacerations, and compressions[4].
Mechanism of Injury for Peripheral Nerves[edit | edit source]
The three most common mechanisms of injury for peripheral nerves are stretch related, lacerations, and compressions. The most common of these three is stretch-related, followed by lacerations, and then compression[5].
Stretch Related[edit | edit source]
Due to the elastic nature of peripheral nerves, stretch related injuries can occur if a traction force is too strong for the nerves elasticity. If the traction force exceeds the nerves stretch abilities, a complete tear could occur. However, it is more common that the continuity of the nerve is retained during this type of injury.[4]
Lacerations[edit | edit source]
Another common type of PNI are lacerations created by blades. those types of injuries might be complete transections- but most commonly some continuity remains.
Compressions[edit | edit source]
The third type of PNI are compression These injuries include the Saturday Night palsy due to radial nerve compression as well as entrapment neuropathies and do not involve tearing of the neural elements[4].
Classification[edit | edit source]
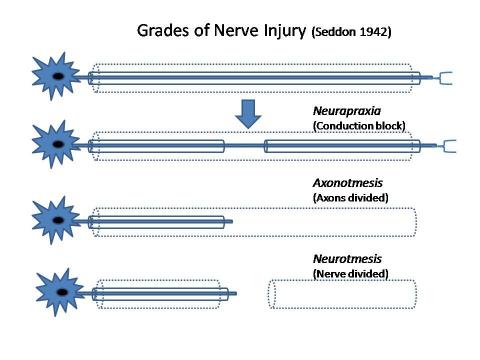
There are two commonly used classifications for PNI- the Seddon Classification and the Sunderland Classification.
Seddon classified nerve injuries into three major groups: neurapraxia, axonotmesis, and neurotmesis whereas Sunderland expanded Seddon's Classification to five degrees of peripheral nerve injury as described in the table below: [5] [6]
| Seddon | Process | Symptoms | Sunderland |
| Neurapraxia | This type of nerve injury is usually secondary to compression pathology. This is the mildest form of peripheral nerve injury with minimal structural damage. This allows for a complete and relatively short recovery period. In a neuropraxic injury, a focal segment of the nerve is demyelinated at the site of injury with no injury or disruption to the axon or its surroundings. This is usually due to prolonged ischemia from excess pressure or stretching of the nerve with no Wallerian degeneration [7]. |
|
First degree |
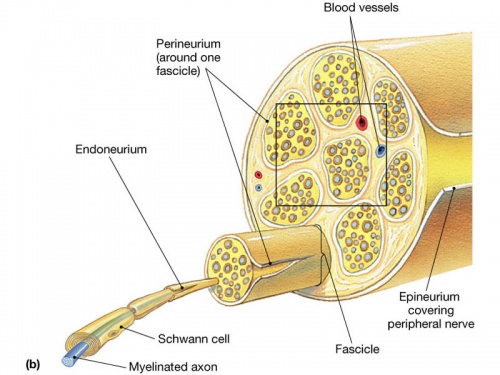
| Axonotmesis | An axonotmesis injury involves damage to the axon and its myelin sheath. However, the endoneurium, perineurium, and epineurium remain intact. Although the internal structure is preserved, the damage of the axons does lead to Wallerian degeneration () This type of nerve injury also results in a complete recovery although it does take longer than a neuropraxic injury. |
|
Second & Third degree |
| Neurotmesis | A neurotmesis injury can occur at different levels and thus Sunderland’s further breakdown into degrees of injury is useful. Disruption of the axon and endoneurium is considered a 3rd-degree injury, disruption of the axon and perineurium is a 4th degree, and a complete disruption of the nerve is classified as a 5th-degree injury. It is important to note that there is a slight overlap when looking at these nerve pathologies and these degrees of injuries are specific to the patient’s injury. Symptoms seen with a neurotmesis injury include no pain (anesthesia), muscle wasting, and complete motor, sensory, and sympathetic function loss () |
|
Third, Fourth, & Fifth Degree |
Nerve Anatomy[edit | edit source]
For a great information source for Physiotherapy following nerve injury see Nerve Injury Rehabilitation Physiotherapy
Resources[edit | edit source]
- http://www.gms-books.de/node/638
- http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-282X2013001100811
References[edit | edit source]
- ↑ Radhakrishnan, R. What are the 4 main functions of the nervous system? Available from https://www.medicinenet.com/4_main_functions_of_the_nervous_system/article.htm (Accessed 18 March 2023).
- ↑ 2.0 2.1 National Institute of Neurological Disorders and Stroke. Peripheral neuropathy. Available from https://www.ninds.nih.gov/health-information/disorders/peripheral-neuropathy (Accessed 18 May 2023).
- ↑ Johns Hopkins Medicine. Peripheral Nerve Injury. Available from https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-nerve-injury (Accessed 18 March 2023).
- ↑ 4.0 4.1 4.2 Burnett MG, Zager EL. Pathophysiology of peripheral nerve injury: a brief review. Neurosurgical focus. 2004 May;16(5):1-7.
- ↑ 5.0 5.1 Campbell WW. Evaluation and management of peripheral nerve injury. Clinical neurophysiology. 2008 Sep 30;119(9):1951-65.
- ↑ Lee SK, Wolfe SW. Peripheral nerve injury and repair. Journal of the American Academy of Orthopaedic Surgeons. 2000 Jul 1;8(4):243-52.
- ↑ Magee D, Manske R. Orthopedic Physical Assessment. 7th Edition. Wichita Kansas. Elsevier, 2020.
- ↑ http://www.gms-books.de/book/living-textbook-hand-surgery/chapter/nerve-injury-classification-clinical-assessment
- ↑ nerve damage and regeneration