Classification of Gait Patterns in Cerebral Palsy
Introduction[edit | edit source]
This page will look at the different types of gait patterns found in people with cerebral palsy, the use of orthosis and the background of use, and interventions which might be used.
Gait Patterns [edit | edit source]
There are a couple of different common gait patterns found in people with cerebral palsy which will be covered in a little more detail below. This page will focus on:
- Spastic Hemiplegia / Unilateral CP
- Bilateral Spastic CP
It will them focus on the different types of gait patterns found within these two groups.
Spastic Hemiplegia / Unilateral CP[edit | edit source]
The most widely accepted classification of gait in spastic hemiplegia is that reported by Winters et al. (1987). They subdivided hemiplegia into four gait patterns based on sagittal plane kinematics. The classification has direct relevance to understanding the gait pattern and management.
- Type 1 –weak or paralysed/silent dorsiflexors (= dropfoot)
- Type 2 – type 1 + triceps surae contracture
- Type 3 – type 2 + hamstrings and/or Rectus Femoris spasticity
- Type 4 – type 3 + spastic hip flexors and adductors
Type 1 Hemiplegia[edit | edit source]
In Type 1 hemiplegia there is a `drop foot' which is noted most clearly in the swing phase of gait, due to inability to selectively control the ankle dorsiflexors during this part of the gait cycle. There is no calf contracture and therefore during stance phase, ankle dorsiflexion is relatively normal. In the experience of the author, this gait pattern is rare, unless there has already been a calf lengthening procedure. The only management maybe needed is a leaf spring or hinged ankle foot orthosis (AFO). Spasticity management and contracture surgery are clearly not required.
Management:[edit | edit source]
Orthotic management may include a leaf spring or hinged AFO.
Type 2 hemiplegia[edit | edit source]
Type 2 hemiplegia is by far the most common type in clinical practice. True equinus is noted in the stance phase of gait because of the spasticity and / or contracture of the gastroc-soleus muscles. There are two sub-catagories to type 2 hemiplegic gait patterns, which are:
- 2a Equinus plus neutral knee and extended hip.
- 2b Equinus plus recurvatum knee and extended hip
There is usually a variable degree of drop foot in swing because of impaired function in tibialis anterior and the ankle dorsiflexors. A pattern of true equinus can be seen, with the ankle in the plantar flexion range through most of the stance phase. The plantar flexion / knee extension couple is over active and the knee may adopt a position of extension or recurvatum.
Management: [edit | edit source]
If there is a mild contracture, supplemental casting can be very effective. The majority of children will also require orthotic support, both to control the tendency to `drop foot‘. Once a significant fixed contracture develops, lengthening of the gastrocnemius and soleus may be indicated. Type 2 hemiplegia with a fixed contracture of the gastroc-soleus constitutes the only indication for isolated lengthening of the tendon achilles. If the knee is fully extended or in recurvatum, then a hinged AFO with an appropriate plantar flexion stop is the most appropriate choice of orthosis. A plantarflexion stop or posterior stop in an AFO is designed to substitute for inadequate strength of the ankle dorsiflexors during swing phase of gait. This stop is effective by limiting the plantarflexion range of motion of the talocrural joint. Older children with progressive valgus deformities are likely to become brace intolerant and require bony surgery.
Common characteristics of types 2, 3 and 4 are a limb length discrepancy (hemiplegic leg is shorter)
Type 3 Hemiplegia[edit | edit source]
Type 3 hemiplegia is characterized by gastroc-soleus spasticity or contracture, impaired ankle dorsiflexion in swing and a flexed, `stiff knee gait' as the result of hamstring/quadriceps cocontraction. Management may consist of at a later stage, muscle tendon lengthening for gastroc-soleus contracture.
Management:
[edit | edit source]
A solid or hinged AFO may also be helpful; the choice should be according to the integrity of the `plantar-flexion, knee-extension couple'.
Type 4 Hemiplegia[edit | edit source]
In Type 4 hemiplegia there is much more marked proximal involvement and the pattern is similar to that seen in spastic diplegia. However, because involvement is unilateral, there will be marked asymmetry, including pelvic retraction. In the sagittal plane there is equinus, a flexed stiff knee, a flexed hip and an anterior pelvic tilt. In the coronal plane, there is hip adduction and in the transverse plane, internal rotation.
Management:[edit | edit source]
Management is similar to Type 2 and Type 3 hemiplegia, in respect of the distal problems. However, there is a high incidence of hip subluxation and careful radiographic examination of the hip is important. The adducted and internally rotated hip will usually require lengthening of the adductors and an external rotation osteotomy of the femur. Failure to address the hip adduction and hip internal rotation will usually mean that any distally focused intervention will fail and the overall outcome will be poor.
Common postural/gait patterns bilateral spastic cerebral palsy
[edit | edit source]
Torsional deformities of the long bones and foot deformities are frequently found in bilateral spastic CP, in association with musculo-tendinous contractures. These are collectively referred to as `lever arm disease‘. The most common bony problems are medial femoral torsion, lateral tibial torsion, mid foot breaching, with foot valgus and abduction. Rotational osteotomies and foot stabilization surgery are often required, in association with the spasticity and contracture management.
This shows the features of `lever arm disease'. There is an out toed stance and gait pattern because of mid foot breaching and lateral tibial torsion), the right image shows the sagittal view shows a crouch gait pattern. When the bony lever (the foot) is both bent and maldirected, the already weakened gastroc-soleus is unable to control the progression of the tibia over the planted foot and a crouch gait results.
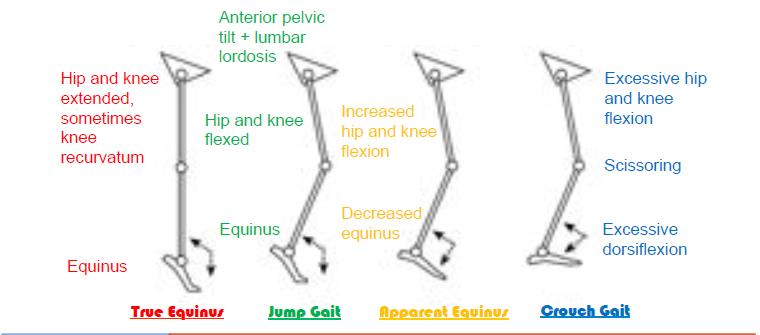
Type 1. True Equinus
[edit | edit source]
When the younger child with bilateral cerebral palsy begins to walk with or without assistance, calf spasticity is frequently dominant resulting in a `true equinus' gait with the ankle in plantar flexion throughout stance and the hips and knees extended. The patient can stand with the foot flat and the knee in recurvatum. The equinus is real, but hidden. A few children with bilateral cerebral palsy remain with a true equinus pattern throughout childhood and, if they develop flexed contracture, may eventually benefit from isolated gastrocnemius lengthening. The persistence of this pattern is unusual and seen in only a small minority of children with bilateral CP. Orthotic management: solid or hinged AFO.
Type 2. Jump gait (with or without stiff knee)[edit | edit source]
The jump gait pattern is very commonly seen in children with diplegia, who have more proximal involvement, with spasticity of the hamstrings and hip flexors in addition to calf spasticity. The ankle is in equinus, the knee and hip are in flexion, there is an anterior pelvic tilt and an increased lumbar lordosis. There is often a stiff knee, because of rectus femoris activity in the swing phase of gait.In younger children, this pattern can be managed effectively by botulinum toxin type A injections to the gastrocnemius and hamstrings and the provision of an AFO. In older children musculotendinous lengthening of the gastrocnemius, hamstrings and iliopsoas may be indicated with transfer of the rectus femoris to semi-tendinosus for co-contraction at the knee.
Type 3. Apparent equinus (with or without stiff knee)[edit | edit source]
As the child gets older and heavier, a number of changes may occur which may render the calf muscle and the plantar flexion – knee extension less competent. Equinus may gradually decrease as hip and knee flexion increase. There is frequently a stage of `apparent equinus' where the child is still noted to be walking on the toes and simple observational gait analysis may mistakenly conclude that the equinus is real, when it is in fact apparent. Sagittal plane kinematics will show that the ankle has a normal range of dorsi-flxion but the hip and knee are in excessive flexion throughout the stance phase of gait.
Management should be focused on the proximal levels, where the hamstrings and iliopsoas may benefit from spasticity treatment or musculotendinous lengthening (Corry et al., 1999). Redirection of the ground reaction vector in front of the knee can best be achieved by the use of a solid or a ground reaction AFO. Orthotic management: ground reaction (Saltiel) AFO, solid AFO or hinged AFO according to the integrity of the plantar flexion – knee extension.
Type 4. Crouch gait (with or without stiff knee gait)[edit | edit source]
Crouch gait is defined as excessive dorsiflexion or calcaneus at the ankle in combination with excessive flexion at the knee and hip. This pattern is part of the natural history of the gait disorder in children with more severe diplegia and in the majority of children with spastic quadriplegia. Regrettably, the commonest cause of crouch gait in children with spastic diplegia is isolated lengthening of the heel cord in the younger child (Sutherland and Cooper, 1978; Borton et al., 2001). Once the heel cord has been lengthened, if the spasticity/contracture of the hamstrings and iliopsoas has not been recognized and is not managedadequately, there will be a rapid increase in hip and knee flexion (Miller et al., 1995). The result is an unattractive, energy expensive gait pattern, followed by anterior knee pain and patellar pathology in adolescence
Crouch gait is always difficult to manage and usually requires lengthening of the hamstrings and iliopsoas, a ground reaction AFO and adequate correction of bony problems such as medial femoral torsion, lateral tibial torsion and stabilization of the foot. By the time it is recognized, the musculoskeletal pathology is usually too advanced to respond to intramuscular BTX-A.
Orthotic management: long-term use of a ground reaction (Saltiel) AFO until the integrity of the plantar flexion- knee extension couple is clearly re-established.
Summary Classification gait patterns bilateral spastic cerebral palsy[edit | edit source]
Gait Analysis [edit | edit source]
Ambulatory children with CP have various types of pathological�gait. Efficient intervention depends on proper evaluation. Video recording can support observation and analysis. But usually observation is the only way of evaluation.�� Computerized gait analysis is an objective, standardized, reproducible and quantifiable method to evaluate gait patterns. Although gait analysis has been shown to alter decision making, there is little evidence that the decisions based on gait analysis lead to better outcomes. Computerized Gait analysis is useful as a research and education tool. It is an additional aid in decision making for treatment. It requires expensive high technology equipment and educated staff. It shows how the child walks graphically but does not tell how functional the gait pattern is unless it measures the amount of energy consumed during walking. It adds little to the clinical examination and remains more a research tool than part of a routine clinical examination in most countries. Consequently, clinical gait analysis remains controversial.
Orthosis in Cerebral Palsy[edit | edit source]
Other words used are braces or splints. Ortho is the Greek word meaning “to make straight”. The evolution of orthoses in CP: From metal and leather to plastic and carbon, with better understanding of the biomechanics; from KAFOs(knee ankle foot orthosis) to AFOs(Ankle Foot Orthosis) with ankle control. Orthopaedic shoes, KAFOs and calipers have largely been abandoned. They are cumbersome, have very limited mechanical advantages, are very difficult to do on and off and in many cases they hide the deformity rather than correct it.
Children with CP are prone to develop deformities of their limbs and spine because of unbalanced forces created by spastic and weak muscles and the effect of gravity (the interaction between all these factors is called biomechanics). Additionally, the muscles may struggle to lengthen in proportion to the growing skeleton, which can cause loss of the ROM at joints. Orthoses can be used to alter body posture in an attempt to prevent deformities and may make some activities easier. However: orthoses may also make activities as crawling, toileting, dressing more difficult. Careful assessment of the benefits versus any disadvantages of often necessary.
Terminology in Orthosis[edit | edit source]
There are a confusing number of names to describe orthoses. The most common and simplest methods describes the parts of the body within the orthosis. Thus the AFO’s (ankle and foot orthoses) enclose the ankle and foot; KAFOs (knee ankle foot orthoses) additionally include the knee joint. WHOs (wrist hand orthoses) or EOs (elbow orthoses) are used for the arm. The names of people or places where orthoses where first used or commercial prodcut names are commonly used, as well with addition of terms like rigid or dynamic.
Solid or rigid AFOs prevent all movement and Hinged AFOs allow partial movement in the ankle