|
|
| (10 intermediate revisions by the same user not shown) |
| Line 4: |
Line 4: |
| '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} |
| </div> | | </div> |
| == Definition/Description == | | == Intoduction == |
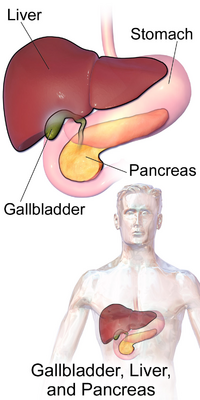
| | [[File:Gallbladder, Liver, and Pancreas.png|right|frameless|400x400px]] |
| | Cholecystitis is an inflammation of the gallbladder, which can be acute or chronic and occur with (calculus) or without (acalculus) gallstones<ref name="p6">HOWARD M. MEDICAL NUTRITION THERAPY IN CHOLECYSTITIS, CHOLELITHIASIS AND CHOLECYSTECTOMY. 2015.</ref>. It occurs most often as a result of impaction of the gallstones in the cystic duct, leading to obstruction of bile flow and painful distention of the gallbladder. It can be very painful and usually needs prompt medical treatment. |
|
| |
|
| {| width="40%" cellspacing="1" cellpadding="1" border="0" align="right" class="FCK__ShowTableBorders"
| | The gallbladder is a small organ underneath the liver on the right side of the upper abdomen. It stores a thick dark green fluid called bile which the liver produces to help with digestion.<ref name=":2">Health Direct Cholecystitis Available:https://www.healthdirect.gov.au/cholecystitis-gallbladder-inflammation (accessed 3.9.2021)</ref> |
| |-
| |
| | align="right" |
| |
| {{#ev:youtube|9qVg4OQTXMA|250}} <ref>WashingtonDeceit. Histopathology Gallbladder--Acute cholecystitis . Available from: http://www.youtube.com/watch?v=9qVg4OQTXMA[last accessed 09/03/13]</ref>
| |
|
| |
|
| |} | | This 2.5 minute video gives a good summary of the condition{{#ev:youtube|SKxl_6QPMHY}} |
|
| |
|
| Cholecystitis is inflammation of the gallbladder which can be acute or chronic and occur with (calculus) or without (acalculus) gallstones<ref name="p6">HOWARD M. MEDICAL NUTRITION THERAPY IN CHOLECYSTITIS, CHOLELITHIASIS AND CHOLECYSTECTOMY. 2015.</ref>. It occurs most often as a result of impaction of the gallstones in the cystic duct, leading to obstruction of bile flow and painful distention of the gallbladder <ref name="G&F">Goodman CC, Fuller K. Pathology Implications for the Physical Therapist Third Edition. Saunders Elsevier: St. Louis; 2009.</ref> Other causes may be typhoid fever or a malignant tumor.<ref name="p7">Goodman CC, Snyder TEK. Differential diagnosis for physical therapists screening for referral. St. Louis, MO: Saunders Elsevier; 2013.</ref><br> | | == Etiology == |
| | Cholecystitis most frequently occurs when gallstones (stones that form within the bile coming down from the liver) block the tube leading out of the gallbladder. This results in a build-up of bile, which causes inflammation. |
|
| |
|
| <br>'''Acute Cholecystitis''' | | Cholecystitis can also be caused by other problems with the bile duct eg a tumour, problems with blood supply to the gallbladder, and [[Infectious Disease|infection]]<nowiki/>s. |
|
| |
|
| <br>
| | The condition may settle down on its own, but cholecystitis tends to come back. Most people eventually need [[Surgery and General Anaesthetic|surgery]] to remove the gallbladder. Sometimes, cholecystitis can lead to liver inflammation, a serious infection, a torn gallbladder, or the death of some of the tissue in the gallbladder. |
|
| |
|
| Inflammation of the gallbladder that develops over hours, usually resulting from a cystic duct obstruction by a gallstone <ref name="Merck Manual" >Porter RS, Kaplan JL. The Merck manual of diagnosis and therapy. Merck Sharp & Dohme Corp.; 2011.</ref>. This form of gallbladder disease usually subsides within 1 to 7 days with a conservative plan of treatment <ref name="G&B">Goodman CC, Boissonnault W. Pathology Implications for the Physical Therapist. Saunders: Philadelphia; 1998.</ref><br>
| | == Epidemiolgy == |
| | Gallstone disease is very common. About 10-20% of the world population will develop gallstones at some point in their life and about 80% of them are asymptomatic. There are approximately 500,000 cholecystectomies done yearly in the United Stated for gallbladder disease. |
|
| |
|
| <br> | | * The incidence of gallstone formation increases yearly with age. |
| | * Over one-quarter of women older than the age of 60 will have gallstones. |
| | * Obesity increases the likelihood of gallstones, especially in women due to increases in the biliary secretion of cholesterol. On the other hand, patients with drastic weight loss or fasting have a higher chance of gallstones secondary to biliary stasis. |
| | * People with chronic illnesses such as diabetes also have an increase in gallstone formation as well as reduced gallbladder wall contractility due to neuropathy.<ref name=":0">Jones MW, Gnanapandithan K, Panneerselvam D, Ferguson T. [https://www.ncbi.nlm.nih.gov/books/NBK470236/ Chronic Cholecystitis]. Available:https://www.ncbi.nlm.nih.gov/books/NBK470236/ (accessed 3.9.2021)</ref> |
| | * Other conditions that cause the breakdown of blood cells, for example, sickle cell disease, also increase the incidence of gallstones.<ref name=":1">Jones MW, Genova R, O'Rourke MC. Acute cholecystitis.Available:https://www.ncbi.nlm.nih.gov/books/NBK459171/ (accessed 3.9.2021)</ref> |
|
| |
|
| <br><br>'''Chronic Cholecystitis''' | | == Pathology == |
| | [[File:Gallbladder.gif|right|frameless]] |
| | Occlusion of the cystic duct or malfunction of the mechanics of the gallbladder emptying is the basic underlying pathologies of this disease. Over 90% of chronic cholecystitis is associated with the presence of gallstones. Gallstones, by causing intermittent obstruction of the bile flow, most commonly by blocking the cystic duct lead to inflammation and edema in the gall bladder wall. Occlusion of the common bile duct such as in neoplasms or strictures can also lead to stasis of the bile flow causing gallstone formation with resultant chronic cholecystitis<ref name=":0" />. |
|
| |
|
| <br> | | Cases of acute untreated cholecystitis could lead to perforation of the gallbladder, sepsis, and death. Gallstones form from various materials such as bilirubinate or cholesterol. These materials increase the likelihood of cholecystitis and cholelithiasis in conditions such as sickle cell disease where red blood cells are broken down forming excess bilirubin and forming pigmented stones. Patients with excessive calcium such as in hyperparathyroidism can form calcium stones. Patients with excessive cholesterol can form cholesterol stones. Occlusion of the common bile duct such as in neoplasms or strictures can also lead to stasis of the bile flow causing gallstone formation.<ref name=":1" /> |
|
| |
|
| {| width="40%" cellspacing="1" cellpadding="1" border="0" align="right" class="FCK__ShowTableBorders"
| | Image 2: Gall Bladder |
| |-
| |
| | align="right" |
| |
| {{#ev:youtube|gxGvP3GV_1E|250}} <ref>WashingtonDeceit. Histopathology Gallbladder--Chronic cholecystitis. Available from: http://www.youtube.com/watch?v=gxGvP3GV_1E[last accessed 09/03/13]</ref>
| |
|
| |
|
| |}
| | == Presentation == |
| | Symptoms of cholecystitis include: |
| | * an intense pain in the middle or right side of the upper abdomen, or between the shoulders |
| | * indigestion, especially after fatty food |
| | * nausea and/or vomiting |
| | * fever |
| | * Symptoms often appear after someone has eaten a large, fatty meal. |
| | == Diagnosis == |
| | If cholecystitis is suspected, the Dr will examine the client and ask you about their medical history. They will usually order an ultrasound of your abdomen. They may also do a blood test to look for signs of liver inflammation or infection<ref name=":2" />. |
|
| |
|
| Chronic Cholecystitis is long standing gall bladder inflammation or prolonged episodes of acute cholecystitis<ref name="p6" /> almost always caused by gallstones <ref name="Merck Manual" />. The gallbladder wall is thickened with fibrosis noted between the layers of the gallbladder and liver<ref name="p6"/> This can also be called cystic duct inflammation. A cholecstectomy, or removal of the gallbladder, is required when symptoms do not resolve with conservative treatment, or may be indicated if a person has chronic cholecystitis <ref name="G&B" />.
| | [[Laboratory Tests|Laboratory testing]] is not specific or sensitive in making a diagnosis of chronic cholecystitis. Leukocytosis and abnormal liver function tests may not be present in these patients, unlike the acute disease. However basic laboratory testing in the form of a metabolic panel, [[Liver Function Tests|liver function]]<nowiki/>s, and complete blood count should be performed. Cardiac testing including [[Electrocardiogram|EKG]] and troponins should be considered in the appropriate clinical setting<ref name=":0" />. |
|
| |
|
| <br>
| | == Treatment == |
| | Cholecystitis can sometimes settle down if you eat a low-fat diet. You may also be given medicine to dissolve gallstones. |
|
| |
|
| Cholecystitis often occurs due to untreated gallstones. Cholelithiasis, or gallstones, are small, pebble-like substances that develop in the gallbladder called calculi <ref name="G&S">Goodman CC, Snyder T. Differential Diagnosis for Physical Therapists Screening for Referral Fourth Edition. Saunders Elsevier: St. Louis; 2007.</ref>. Gallstones occur when liquid stored in the gallbladder is not secreted properly and hardens into pieces of stone-like material. The liquid—called bile—helps the body digest fats. Bile is made in the liver, then stored in the gallbladder until the body needs it. The gallbladder contracts and pushes the bile into a tube—called the common bile duct—that carries it to the small intestine, where it helps with digestion <ref name="NDDIC">National Digestive Diseases Information Clearinghouse. http://digestive.niddk.nih.gon. Last accessed April 11, 2010</ref>. Gallstones can also be collection of cholesterol, bile pigment or a combination of the two, which can form in the gallbladder or within the bile ducts of the liver. Cholesterol stones form due to an imbalance in the production of cholesterol or the secretion of bile. 80 percent of all gallstones diagnosed are of cholesterol form <ref name="G&F" />. Pigmented stones are primarily composed of bilirubin, which is a chemical produced as a result of the normal breakdown of red blood cells <ref name="TACG">The American College of Gastroenterology. http://www.acg.gi.org/patients/gihealth.asp#GI. Last accessed April 11, 2010.</ref>. The bilirubin stones account for 20 percent of the stones being diagnosed <ref name="G&F" />. Someone can develop what is called acholelithiasis cholecystitis, or inflammation of the gallbladder without gallstones <ref name="G&B" />. <br>
| | If admitted to hospital, client will be fed and hydrated through an intravenous drip and may have antibiotics to fight infection. They also will probably also need medicine for pain relief. |
|
| |
|
| == Prevalence == | | * Most people have their gallbladder removed 2 to 3 days after they are admitted to hospital (preferred recommended treatment is the removal of the gallbladder). In the past, this was done through an open laparotomy incision. Now laparoscopic cholecystectomy is the procedure of choice. This procedure has low mortality and morbidity, a quick recovery time (usually one week), and good results<ref name=":1" />. |
| | * You don’t need your gallbladder, and after the operation, bile will flow straight from your liver to your small intestine<ref name=":2" />. |
|
| |
|
| In the United States, the most common type of gallstones is made of cholesterol. Bilirubin gallstones are more common in Asians and Africans, but are seen in diseases that damage red blood cells such as sickle cell anemia. American Indians have the highest rate of gallstones in the United States. The majority of American Indian men have gallstones by age 60. Among the Pima Indians of Arizona, 70 percent of women have gallstones by age 30 <ref name="NDDIC" /><ref name="TACG" />.
| | The diagnosis and management of cholecystitis is a multi-disciplinary team approach. A high index of suspicion is vital in the diagnosis. Referral to the surgical team followed by decision making on the need for laparoscopic surgery are the next steps. Good surgical care with good postoperative follow up is also essential. Counseling for food habits with nutritionist support and lifestyle changes are crucial in patients being treated conservatively.<ref name=":0" /> |
|
| |
|
| <br>
| | == Physical Therapy Management == |
|
| |
|
| Gallstones, occur increasingly with advancing age, so 20% of men and 35% of women have gallstones present by the age of 75. It is estimated that 15-20 million people in the United States have gallstones <ref name="G&B" /><ref name="G&S" />. Cholelithiasis is the fifth leading cause of hospitalization among adults. Gallstones account for 90% of all gallbladder and duct diseases <ref name="G&S" />. Greater than 80% of patients are asymptomatic with gallstones.<ref name="p1">John P, Pasley A. Torsion of Hydrosalpinx with Concurrent Acute Cholecystitis: Case Report and Review of Literature. Case Reports In Surgery [serial on the Internet]. (2016, Dec 14), [cited March 22, 2017]; 1-4. Available from: Academic Search Complete.</ref>
| | *Systemic screen indicated if mid back, scapular, or right shoulder pain with no trauma<ref name="p7">Goodman CC, Snyder TEK. Differential diagnosis for physical therapists screening for referral. St. Louis, MO: Saunders Elsevier; 2013.</ref>. |
| | | *Immediate referral: new onset myopathy (especially older adult) with a history of statin use<ref name="p7" />. |
| <br>
| |
| | |
| Cholelithiasis is the most common gastrointestinal disease in the United States. 25 percent of all cases, symptoms and complications develop secondary to the the presence of gallstones. These cases will require surgery or other forms of treatment <ref name="G&F" />. <br><br>
| |
| | |
| == Pathology<ref name="G&F" /> ==
| |
| | |
| Cholesterol that is needed to form cholesterol gallstones mainly comes from the diet. Cholesterol is then absorbed into the liver from the blood by receptors. Each lipoprotein has its own receptor. Low density lipoproteins are removed from the blood by the binding of the apo B,E receptor. The B1 receptor travels around looking for high density lipoproteins and removes them. Through a series of reactions and protein interactions helps keep this process moving.
| |
| | |
| The bile that is produced in the liver helps aid in the excretion of excess cholesterol. Biliary lipids that are secreted from the liver help compose bile. Each of the lipids secreted into bile has a specific transporter. Once the lipids are secreted into the bile, the phospholipids and cholesterol form vesicles while the bile salts form micelles. The vesicles and micelles interact and pass through the gallbladder.
| |
| | |
| Cholesterol needs detergent properties of the phospholipids and bile salts to remain a liquid solution. If there is a larger presence of cholesterol in bile, the bile will become oversaturated with cholesterol and then crystals will form.
| |
| | |
| Common mechanisms associated with cholesterol stone formation are:
| |
| | |
| #Stasis of bile in the gallbladder- this may occur when insoluble or supersaturated cholesterol is absorbed into the wall of the gallbladder. This leads to difficulty contracting the smooth muscles. This commonly seen in pregnancy, after a period of weight loss, RA patients, and patients receiving total parenteral nutrition (TPN).
| |
| #Changes in mucin glycoproteins- there are several proteins that interact with the miced micelles during the tranport process from the liver to the gallbladder, mucin glycoproteins are shown to form cholesterol stones. Patients who experience rapid weight loss may have an increase in mucin glycoprotein production
| |
| #Processes that may increase the amount of cholesterol or reduce the amount of bile salts or phospholipids that are secreted into bile
| |
| | |
| Pigmented stones:
| |
| | |
| Black stones are caused by an increase in the production of unconjugated bilirubin. This type of stone occurs in the patient population who have chronic hemolysis (i.e. sickle cell anemia) or have end-stage liver disease.
| |
| | |
| Brown stones are less common. These occur in geographic areas where biliary infections are prevalent. Brown stones can form in the gallbladder or in the ducts and form secondary to anaerobic bacterial infections.
| |
| | |
| Cholecystitis, if left untreated, can result in infectious complications, extreme inflammation, tissue necrosis, gangrenous gallbladder, absceses, or perforation.<ref name="p6" />
| |
| | |
| == Clinical Presentation<br> ==
| |
| | |
| *Colicky Right Upper Quadrant Pain and tenderness especially near the right subcostal region especially after the person has eaten fatty foods. <ref name="p7" />
| |
| *Symptoms worse immediately after eating (inflammation of the gall bladder)<ref name="p7" />
| |
| *Low grade fever to high grade fever <ref name="Merck Manual" /><ref name="G&S" />
| |
| *Chills <ref name="Merck Manual" /><ref name="G&S" />
| |
| *Pain and nausea 1-3 hours after eating (gallstones)<ref name="p7" /><br>
| |
| *Vomiting <ref name="Merck Manual" />
| |
| *Abdominal Pain- may be intermittent or steady <ref name="G&B" />
| |
| *Rigors with rebound tenderness or ileus
| |
| *Interscapular pain <ref name="G&B" />
| |
| *Heartburn, belching, flatulence, epigastric discomfort, and food intolerance (especially to fats and cabbage) <ref name="G&B" /><ref name="G&S" />.
| |
| *Jaundice- this is a result of blockage of the common bile duct <ref name="G&S" />.
| |
| *Green hued skin
| |
| *Persistent pruritis or skin itching can occur at peripheral sites that are innervated by the same spinal cord level as the gallbladder <ref name="G&S" /><ref name="p7" /><br>
| |
| *Anterior rib pain (tip of 10th rib; can also affect ribs 11 and 12) <ref name="G&S" />.
| |
| *Dark Urine, Light Stools
| |
| *Bleeding from skin and mucous membranes and weight loss- late signs of gall bladder cancer
| |
| *Feeling of fullness or indigestion<ref name="p7" />
| |
| *Referred viscerogenic heart pain<ref name="p7" />
| |
| | |
| If a patient presents with any of the following they should be advised to see their doctor immediately:<br>
| |
| | |
| *prolonged pain—more than 5 hours
| |
| *nausea and vomiting
| |
| *fever—even low-grade—or chills
| |
| *yellowish color of the skin or whites of the eyes
| |
| *clay-colored stools <ref name="NDDIC" />
| |
| | |
| <br>
| |
| | |
| *Referred pain: R upper trapezius and shoulder, R interscapular (T4-T8), R subscapular region
| |
| *Celiac (abdominal) and splanchnic (visceral) connect the sympathetic fibers of the biliary system in turn producing the referral of interscapular radiating pain primarily right sided. The splanchnic nerves intertwine with the phrenic nerve (diaphragm) producing referral pain to the right shoulder. <ref name="p7" />
| |
| | |
| <br>
| |
| | |
| Most gallstones are asymptomatic: approximately 30% cause symptoms of cholecystitis. Gallstones in the older population may not cause pain, fever, or jaundice. Mental confusion and shakiness may be the only symptoms the elderly patient may present with <ref name="G&B" />.
| |
| | |
| == Associated Co-morbidities <ref name="NDDIC" /><ref name="TACG" /> ==
| |
| | |
| The development of pigmented stones is not fully understood. People who develop pigmented stones often have liver cirrhosis, biliary tract infections, or hereditary blood disorders—such as sickle cell anemia—in which the liver makes too much bilirubin. If a person already has gallstones present this may lead to the formation of more gallstones. Secondary complications from untreated AC include sepsis, peritonitis, and cholecystoenteric fistulas. <ref name="p9">ASİLTÜRK LÜLLECİ Z, BAŞYİĞİT S, PİRİNÇÇİ SAPMAZ F, UZMAN M, KEFELİ A, NAZLIGÜL Y, et al. Comparison of ultrasonographic and laboratory findings of acute cholecystitis between elderly and nonelderly patients. Turkish Journal Of Medical Sciences [serial on the Internet]. (2016, Oct), [cited March 21, 2017]; 46(5): 1428-1433. Available from: Academic Search Complete.</ref>
| |
| | |
| == Medications ==
| |
| | |
| Actigall, Ursodiol
| |
| | |
| *Naturally ocurring bile acid<ref name="p6" />
| |
| *Gallstone dissolution therapy used for radiolucent stones <20 mm. Patients need to be monitored every 6 months with ultrasound. This should also be used for 3 months after dissolution and must be given with food. It is not recommended for children. May cause diarrhea, dyspepsia, abdominal pain, nausea, vommiting, dizziness, and constipation. Actigall woks by decreasing cholesterol synthesis, secretion, and absorption. It also works by altering bile cholesterol composition<ref>Online. https://online.epocrates.com/noFrame/showPage.do?method=diseases&MonographId=78&ActiveSectionId=35. Accessed April 10, 2010.</ref>.
| |
| | |
| Ursodeoxycholic Acid<ref name="p6" />
| |
| | |
| *decreases cholesterol saturation Ezetimide, Zetia
| |
| *Cholesterol absorption inhibitor
| |
| *Antihyperlipidemic
| |
| | |
| == Diagnostic Tests/Lab Tests/Lab Values ==
| |
| | |
| Cholecystitis is most often diagnosed with the use of '''ultrasound '''with 88% sensitivity and 80% specificity<ref>Gastroenterology. http://www.acg.gi.org/patients/gihealth.asp#GI. Last accessed April 11, 2010.</ref><ref name="p1" />. An abdominal ultrasound examination is a quick, sensitive, and relatively inexpensive method of detecting gallstones in the gallbladder or common bile duct. This is the test most often used <ref name="TACG" /><br>
| |
| | |
| <u>'''Murphy's Sign '''</u>is a screening test performed by clinicians to assess for cholecystitis.<ref name="Cook Examination Tests Textbook">Cook C., Hegedus E. Orthopaedic Physical Examination Tests: an evidence based approach. 2nd ed. Upper Saddle River NJ, Pearson Education Inc. 2013</ref><ref>Bree RL. Further observations on the usefullness of the sonographic Murphy Sign in the evaluation of suspected acute cholecystitis. J Clin Ultrasound. 1995; 23: 169-172</ref><ref>Singer AJ. McCracken G, Henry Mc, et al. Correlation among clinical , laboratory and hepatobiliary scanning findings in patients with suspected acute cholecystitis. Ann Emerg Med. 1996; 28; 267-272</ref><ref>Ralls PW, Halls J, Lapin Sa, et al. Prospective evaluation of the sonographic Murphy Sign in supspected acute cholectystis. J Clin Ultrasound. 1982; 10; 113-115</ref>
| |
| | |
| *Patient lies supine with relaxed abdomen
| |
| *Therapist places one hand on the right, posterior, inferior costal margin.
| |
| *Therapist places the other hand on the right upper abdominal quadrant (subcostal).
| |
| *Therapist applies slight pressure (palpates deeply) while patient inspires<br>+ sign if pain is reproduced or client stops inspiration<br>
| |
| | |
| Sensitivity: 86%, 63%, 97% <ref name="Cook Examination Tests Textbook" /><br> Specificity: 35%, 94%, 48%<br> +LR (1.32, 9.84, 1.88)
| |
| | |
| {{#ev:youtube|-14qBaTck6Q}}
| |
| | |
| <br>
| |
| | |
| <br><u>'''Right upper quadrant pain<ref name="p5">Jain A, Mehta N, Secko M, Schecter J, Papanagnou D, Pandya S, Sinert R. History, Physical Exam. Laboratory Testing and Emergency Department Ultrasonography for the Diagnosis of Acute Cholecystitis. Academic Emergency Medicine. 2016 Nov 1.</ref>'''</u>
| |
| | |
| Sensitivity: 56% to 93%
| |
| | |
| Specificity: 0% to 96%
| |
| | |
| +LR: 0.92 to 14.02
| |
| | |
| -LR: 0.46 to 7.86<br><br>
| |
| | |
| Cholescintigraphy <ref name="Merck Manual" />- the patient is injected with a small amount of radioactive material and is absorbed by the gallbladder. Then the gall bladder is stimulated to see how well it contracts or if there is an obstruction within the bile ducts <ref name="NDDIC" />.
| |
| | |
| Abdominal CT scan
| |
| | |
| Early diagnosis of AC with hepatobiliary scintigraphy (HIDA), which is superior to US, can reduce length of stay, overall costs and time to surgery<ref name="p2">Rodriguez L, Santaliz-Ruiz L, De La Torre-Bisot G, Gonzalez G, Serpa M, Bolanos-Avila G, et al. Clinical implications of hepatobiliary scintigraphy and ultrasound in the diagnosis of acute cholecystitis. International Journal Of Surgery (London, England) [serial on the Internet]. (2016, Nov), [cited March 22, 2017]; 35196-200. Available from: MEDLINE.</ref>.
| |
| | |
| Magnetic Resonance Imaging (MRI) is comparable to the use of HIDA when measuring cystic duct patency<ref name="p3">Corwin M, Malutich S, Salcedo E, Fananapazir G, Brock J, McGahan J. Evaluation of cystic duct patency: comparison of functional MR cholangiography with gadoxetate disodium and hepatobiliary scintigraphy in suspected acute cholecystitis. Clinical Imaging [serial on the Internet]. (2016, Sep), [cited March 22, 2017]; 40(5): 973-978. Available from: MEDLINE.</ref>.
| |
| | |
| Complete Blood Cell Count (CBC): the presence of an elevated white blood count to 12,000-15,000 per microL.
| |
| | |
| Liver Function Test <ref name="Merck Manual" />- total serum bilirubin levels, serum amniotransferase, and alkaline phosphotase levels are commonly elevated in acute cholecystitis, but normal or minimally elevated in the chronic form <ref name="G&B" />.
| |
| | |
| X-Rays of the abdomen may show radiopaque gallstones in only 15% of all cases <ref name="G&F" />.
| |
| | |
| The diagnosis of gallstones is suspected when symptoms of right upper quadrant abdominal pain, nausea or vomiting occur. The location, duration and “character” (stabbing, gnawing, cramping) of the pain help to determine the likelihood of gallstone disease. Abdominal tenderness and abnormally high liver function blood tests, fever, elevated WBC count, elevated C-reactive protein, or imaging indicating thickening of the gallbladder or pericholecystic fluid<ref name="p9" /><ref name="p0">Yuzbasioglu Y, Duymaz H, Tanrikulu C, Halhalli H, Koc M, Coskun F, et al. Role of Procalcitonin in Evaluation of the Severity of Acute Cholecystitis. Eurasian Journal Of Medicine [serial on the Internet]. (2016, Oct), [cited March 22, 2017]; 48(3): 162-166. Available from: Academic Search Complete.</ref>.<br>
| |
| | |
| == Causes <ref name="NDDIC" />, <ref name="TACG" />, <ref name="G&S" /> ==
| |
| | |
| {| width="40%" cellspacing="1" cellpadding="1" border="0" align="right" class="FCK__ShowTableBorders"
| |
| |-
| |
| | align="right" |
| |
| {{#ev:youtube|WmcOAb9e-5Y|250}} <ref>livestrong. Gallstones Health Byte. Available from: http://www.youtube.com/watch?v=WmcOAb9e-5Y[last accessed 09/03/13]</ref>
| |
| | |
| |}
| |
| | |
| <br> The following are other risk factors that may contribute to the formation of gallstones, particularly cholesterol stones:
| |
| | |
| *Sex: Women are more likely to develop gallstones than men <60 years of age<ref name="p7" />. This is due to an excess amount of estrogen from pregnancy, hormone replacement therapy, and birth control pills appears to increase cholesterol levels in bile. This then decreases the motility in the gallbladder, which then can lead to gallstones.
| |
| *Family history: Other family members tend to develop gall stones, which leads researchers to believe that people are genetically inclined to develop gall stones.
| |
| * Weight: People who are moderately overweight have an increased risk for developing gallstones. The most likely reason is that the amount of bile salts in the bile is reduced, leading to an increase in cholesterol. The increase in cholesterol reduces the gallbladders ability to empty. Obesity is a major risk factor for gallstones, especially in women.
| |
| * Diet: Diets that are high in fat and cholesterol and low in fiber increases the risk of gallstones due to increased cholesterol in the bile and reduced gallbladder emptying.
| |
| * Rapid weight loss: As the body metabolizes fat during prolonged fasting and rapid weight loss—such as “crash diets" leads to the liver secreting extra cholesterol into the bile, which then can cause gallstones. In addition, the gallbladder does not empty properly. If a patient has had gastric bypass surgery to help loose weight this puts them at risk for developing gallstones.
| |
| * Age: People over the age 60 are more likely to develop gallstones than younger people. As people age, the body tends to secrete more cholesterol into bile. With this increase in secretion of cholesterol there is a simulatneous decrease in bile salt production. <br>
| |
| * Ethnicity: American Indians are genetically predisposed to secrete high levels of cholesterol in bile. Mexican American men and women of all ages also have high rates of gallstone formation.
| |
| * Cholesterol-lowering drugs: Drugs that lower cholesterol levels in the blood actually increase the amount of cholesterol secreted into bile. This then leads to an increased risk of gallstones.
| |
| * Diabetes: People with diabetes generally have high levels of fatty acids called triglycerides. These fatty acids may increase the risk of gallstone formation.<br>
| |
| *Drugs: Estrogen is one of the most common studied drug that leads to gallstones. Other drugs that have been shown to cause the formation of gallstones are ceftriaxone, clofibrate, and octreotide.
| |
| *Liver disease<ref name="p7" />.
| |
| | |
| == Systemic Involvement <ref name="G&S" /> ==
| |
| | |
| Shoulder pain can be from any of the following:
| |
| | |
| Cancer-metastases to nodes of axilla or mediastinum, metastases to lungs from the bone, breast, kidney, colorectal, pancreas, and uterus, metastases to thoracic spine from breast, lung, and thyroid, Breast Cancer, Pancreatic Cancer.
| |
| | |
| Cardiovascular- Thoracic Outlet Syndrome, Myocardial Infarct, Post CABG, Bacterial Endocarditis, Aortic Aneurysm, Empyema and lung abscess, Dissecting aortic aneurysm.
| |
| | |
| Pulmonary- Pulmonary TB, PE, Spontaneous Pneumothorax, Pancoast's tumor, Pneumonia.
| |
| | |
| Renal/urologic- Kidney stones, Obstruction, inflammation or infection of the upper urinary tract.
| |
| | |
| Gastrointestinal/Hepatic- Hiatal Hernia, Peptic/duodenal ulcer, Ruptured Spleen, Liver/gallbladder disease, Pancreatic Disease, Ectopic pregnancy.
| |
| | |
| Gynecologic- Mastodynia, Subphrenic abscess.
| |
| | |
| Other- Mononucleosis, Osteomyelitis, Syphillis, Herpes Zoster, Diabetes, Sickle Cell Anemia, Hemophilia, Diaphragmatic hernia, Anterior spinal surgery.
| |
| | |
| == Medical Management (current best evidence)<ref name="NDDIC" />,<ref name="TACG" /> ==
| |
| | |
| {| width="100%" cellspacing="1" cellpadding="1"
| |
| |-
| |
| | {{#ev:youtube|7tTGfYCqH5w|300}}
| |
| | {{#ev:youtube|Pr3Md9XlLvw|300}}
| |
| |}
| |
| | |
| ==== Surgical Treatment<br> ====
| |
| | |
| A patient may present with diagnosed but untreated gallstones in the case where they are asymptomatic. However, if a patient has had several frequent attacks, they need to see their doctor. The doctor may recommend removing the gallbladder, an operation called cholecystectomy. The gold standard for treating symptomatic cholecystitis is laparoscopic cholecystectomy. Research supports that early surgery is safe for acute cholecystitis and reduces morbidity, hospital stay, fewer ICU admissions and fewer injuries to the main bile duct when compared to delayed cholecystectomy<ref name="p6" /><ref name="p8">Sánchez-Carrasco M, Rodríguez-Sanjuán J, Martín-Acebes F, Llorca-Díaz F, Gómez-Fleitas M, Sánchez-Manuel F, et al. Evaluation of Early Cholecystectomy versus Delayed Cholecystectomy in the Treatment of Acute Cholecystitis. HPB Surgery [serial on the Internet]. (2016, Oct 10), [cited March 21, 2017]; 1-8. Available from: Academic Search Complete.</ref><ref name="p4">Terho P, Leppäniemi A, Mentula P. Laparoscopic cholecystectomy for acute calculous cholecystitis: a retrospective study assessing risk factors for conversion and complications. World Journal Of Emergency Surgery [serial on the Internet]. (2016, Nov 16), [cited March 22, 2017]; 111-9. Available from: Academic Search Complete.</ref>. Recovery after the surgery usually involves only one night in the hospital, and normal ADL's can be resumed a few days later. Due to the abdominal muscles not being cut during the surgery, their is less pain and fewer complications than after an “open” surgery. This type of surgery requires a 5- to 8-inch incision across the abdomen.<br>If the tests ordered by the physician show an abnormal amount of inflammation, infections and or scarring secondary to other operations, the physician may choose to do an "open surgery" for removal of the gallbladder. If during the laproscopic procedure the surgeon finds the above mentioned problems a larger incision is made. Recovery from the open procedure requires a 3-5 day stay in the hospital. This type of surgery is onle needed in about five percent of all gallbladder operations performed.
| |
| | |
| Mortality rate increases 30% in geriatrics with comorbities who receive surgery. Percutaneous cholecystectomy (PC) is an alternate treatment in which the gallbladder is surgically emptied while under local anesthetic. PC should be used as a quick and temporary life-saving measure or to delay the need for more complex surgery<ref name="p7"/><ref name="p1" />.<br>One of the most common complications with gallbladder surgery is that there is an increased risk for injury to the bile ducts. Injury to the common bile duct will cause bile to leak out and cause and extreme amount of pain and a potentially dangerous infection. Mild injuries to the bile ducts can sometimes be treated without surgery. However, major injuries, are more serious and leads to more surgery. Other surgical complications may include bleeding or surgical site infection<ref name="p8" />.<br>
| |
| | |
| {| width="40%" cellspacing="1" cellpadding="1" border="0" align="right" class="FCK__ShowTableBorders"
| |
| |-
| |
| | align="right" |
| |
| {{#ev:youtube|qFM6j-RkESA|250}} <ref>emedtv. ERCP with Balloon Dilation. Available from: http://www.youtube.com/watch?v=qFM6j-RkESA[last accessed 09/03/13]</ref>
| |
| | |
| |}
| |
| | |
| If gallstones are found to be in the bile ducts, the gastroenterologist may use endoscopic retrograde cholangiopancreatography (ERCP) to locate and remove the stones before or during gallbladder surgery. A person on occasion, who has had a cholecystectomy, may be diagnosed with gallstones in the bile ducts weeks or years after. The ERCP procedure is successful in removing the stone in these cases. If performing an ERCP the surgeon finds gallstones in the gallbladder itself a cholecystectomy has to be performed. This procedure does not remove stones from the gallbladder.<br>
| |
| | |
| ==== Nonsurgical Treatment<br> ====
| |
| | |
| Nonsurgical approaches are mainly used when a patient has serious medical conditions that prevent surgery. Nonsurgical treatments are used also only on cholesterol stones. Stones can reocur within 5 years if a patient has been treated nonsurgically.<br>
| |
| | |
| Some types of nonsurgical treatment are:
| |
| | |
| #'''Oral dissolution therapy'''. This is where drugs made from bile acids are used to help dissolve the gallstones. The most common drugs used for small stones are ursodiol (Actigall) and chenodiol (Chenix). However, this type of treatment take a really long time for the stone to completely dissolve.<br>
| |
| #'''Contact dissolution therapy'''. This is an experimental procedure that involves injecting a drug directly into the gallbladder that will help dissolve cholesterol stones. The most common drug that is used in this type of treatment is, methyl tert-butyl ether. This is a fast acting treatment that dissolves the stone in 1-3 days.
| |
| | |
| == Physical Therapy Management (current best evidence) <ref name="G&B" /><ref name="G&F" /> ==
| |
| | |
| *Systemic screen indicated if mid back, scapular, or right shoulder pain with no trauma<ref name="p7" />.
| |
| *Immediate referral: new onset myopathy (especially older adult) with a history of statin use<ref name="p7" />.<br> | |
| *Physician referral: Hx of cancer or risk factors for hepatitis with obvious signs of hepatic disease, unknown cause arthralgias with hx or risk factors for hepatitis, bilateral carpal tunnel syndrome or asterixis, unknown sensory neuropathy with associated hepatic signs and symptoms<ref name="p7" />. | | *Physician referral: Hx of cancer or risk factors for hepatitis with obvious signs of hepatic disease, unknown cause arthralgias with hx or risk factors for hepatitis, bilateral carpal tunnel syndrome or asterixis, unknown sensory neuropathy with associated hepatic signs and symptoms<ref name="p7" />. |
| *Screen for hepatic diseases if: R shoulder/scapular/midback pain with unknown cause, unable to localize shoulder pain that is not limited by painful symptoms, GI symptoms especially associated with eating, bilateral carpal or tarsal tunnel syndrome, personal hx of hepatitis, cancer, liver, gallbladder disease, recent hx of statin usage, recent operation (post-operative jaundice), injection drug use <6mo, skin or eye color changes, alcohol consumption, contact with others with jaundice<ref name="p7" />. | | *Screen for hepatic diseases if: R shoulder/scapular/midback pain with unknown cause, unable to localize shoulder pain that is not limited by painful symptoms, GI symptoms especially associated with eating, bilateral carpal or tarsal tunnel syndrome, personal hx of hepatitis, cancer, liver, gallbladder disease, recent hx of statin usage, recent operation (post-operative jaundice), injection drug use <6mo, skin or eye color changes, alcohol consumption, contact with others with jaundice<ref name="p7" />. |
| Line 260: |
Line 73: |
| *wound splinting | | *wound splinting |
| *compressive stockings | | *compressive stockings |
| *lower extremity exercises<br> | | *lower extremity exercises<ref name="G&B">Goodman CC, Boissonnault W. Pathology Implications for the Physical Therapist. Saunders: Philadelphia; 1998.</ref><ref name="G&F">Goodman CC, Fuller K. Pathology Implications for the Physical Therapist Third Edition. Saunders Elsevier: St. Louis; 2009.</ref> |
| | |
| <br> {{#ev:youtube|SKxl_6QPMHY}}
| |
| | |
| == Differential Diagnosis<ref name="G&S" /> ==
| |
| | |
| Obstruction of the gallbladder can lead to:
| |
| | |
| *biliary stasis
| |
| *delayed gallbladder emptying
| |
| *These two combined can occur with any pathological condition of the liver, hormonal influencse, and pregnancy.
| |
| | |
| Cholelithiasis- stones (calculus) that form in the gallbladder as a result of changes in bile<ref name="p7" />
| |
| | |
| Biliary Colic- stone is lodged in the cystic duct; gallbladder contracts to push stone through. Pain increases to a peak then fades<ref name="p7" />
| |
| | |
| Cholangitis- this is where the gallstone get lodged further down into the common bile duct. If bile flow is blocked at the biliary tree this can lead to jaundice.<ref name="p7" />
| |
| | |
| Primary Biliary Cirrhosis- this is a chronic progressive, inflammatory disease of the liver that involves primarily the intrahepatic bile duct and results in the impairment of bile secretion.
| |
| | |
| Gallbladder Cancer- this is closely associated with gallstone disease. If this is diagnosed it is usually in later stages and often has a poor outcome.
| |
| | |
| Gallstone Pancreatitis- this is the inflammation of the pancreas secondary to blockage of the pancreatic duct via a gallstone. The blockage occurs at the sphincter of Oddi. If a stone from the gallbladder travels down the common bile duct and gets stuck in the sphincter, it will block the flow of all material from the liver and pancreas. This leads to inflammation of the pancreas and can be quite severe. Gallstone pancreatitis can be a life-threatening disease and evaluation by a physician urgently is needed if someone with gallstones suddenly develops severe abdominal pain <ref name="TACG" /><br>
| |
| | |
| Sphincter of Oddi Dysfunction- Sphincter of Oddi Dysfunction (SOD) is a symptom complex of intermittent upper abdominal pain and may be accompanied by nausea and vommitting. This is thought to be caused from scarring or spasm of the sphincter of Oddi muscle. This is a small circular muscle that is a ½ inch in length, located at the end of the bile duct and pancreas duct. This muscle works to keep the bile duct and pancreatic duct muscles closed; this prevents reflux of intestinal contents into the bile duct and pancreas duct. If this muscle should spasm or scar, drainage of the bile duct and/or pancreas duct may be hindered. Abnormal dilation of the bile duct and/or pancreas duct is often associated with an increase in the products and enzymes made by the liver, gallbladder and pancreas, which can be tested for with blood tests (serum liver tests, amylase, lipase). If the ducts are blocked this may result in pain <ref name="TACG" /><br>
| |
| | |
| Peptic Ulcer Disease- characterized by burning, epigastric pain that occurs after meals. This often wakes patients up at night and pain improves with eating <ref name="epoc">Epocrates Online. https://online.epocrates.com/noFrame/showPage.do?method=diseases&MonographId=78&ActiveSectionId=35. Accessed April 10, 2010.</ref>.<br>
| |
| | |
| Acute Pancreatitis- this is characterized by epigastric or periumbilical abdominal pain radiating to the back <ref name="epoc" />.
| |
| | |
| Sickle Cell Crises- this is typically associated with gallstone disease. A patient may experience pain anywhere in the body, which can be unrelated to the formation of gallstones <ref name="epoc" />.
| |
| | |
| Appendicitis- a patient may experience pain in the right lower quadrant near the iliac crest. To rule this out look for rebound tenderness at McBurney's point. Pain a patient experiences with appendicitis may complain that it started in the periumbilical region <ref name="epoc" />.
| |
| | |
| Right Lower Lobe Pneumonia- a patient who presents with this will have a productive cough and fever. Listen to a patients breath sounds to help rule this out, in doing so one will hear bronchial breath sounds <ref name="epoc" />. <br>
| |
| | |
| Acute Coronary Syndrome- a person will typically experience central chest pain that radiates to the left arm or jaw. A patient may experience pain the epigastrum region. One thing to be listening for in the history is previous history of chest pain and or look for risk factors for coronary artery disease <ref name="epoc" />.
| |
| | |
| GERD- a patient who presents with thsi will have a burning sensation in chest after meals. This sensation is made worse on bending over or lying down. A patient may also have acid reflux and dysphagia <ref name="epoc" />. <br>
| |
| | |
| Gynecological- women with lower abdominal pain should include gynecological causes such as torsion of hydrosalpinx as a differential diagnosis<ref name="p1" />.
| |
| | |
| Other causes of lower abdominal pain may include pyelonephritis, cystitis, biliary ro renal colic, perforated or obstructed intestine, mesenteric lymphadenitis, hernia, inflammatory bowel disease or diverticulitis<ref name="p1" />
| |
| | |
| == Prognosis == | | == Prognosis == |
|
| |
|
| The prognosis for acute and chronic cholecystitis is good if the patient seeks medical treatment. An increase in serum WBC count, ESR, C-reactive protein, and procalcitonin levels indicate an increase in severity of cholecystitis. Also, gangrene and abscess increase the risk of conversion<ref name="p0" />. All of these factors increase the risk of post-operative complication<ref name="p4" />. Acute attacks should resolve spontaneously, but a person may experience reoccurences. This may lead to the patient having their gallbladder removed. Old age is a poor prognostic factor as mortality secondary to acute cholecystitis is 5 to 10 percent for clients that are older than 60 and have serious associated diseases<ref>Goodman CC, Fuller K. Pathology Implications for the Physical Therapist Third Edition. Saunders Elsevier: St. Louis; 2009.</ref><ref>ASİLTÜRK LÜLLECİ Z, BAŞYİĞİT S, PİRİNÇÇİ SAPMAZ F, UZMAN M, KEFELİ A, NAZLIGÜL Y, et al. Comparison of ultrasonographic and laboratory findings of acute cholecystitis between elderly and nonelderly patients. Turkish Journal Of Medical Sciences [serial on the Internet]. (2016, Oct), [cited March 21, 2017]; 46(5): 1428-1433. Available from: Academic Search Complete.</ref>. | | The prognosis for acute and chronic cholecystitis is good if the patient seeks medical treatment. An increase in serum WBC count, ESR, C-reactive protein, and procalcitonin levels indicate an increase in severity of cholecystitis. Also, gangrene and abscess increase the risk of conversion<ref name="p0">Yuzbasioglu Y, Duymaz H, Tanrikulu C, Halhalli H, Koc M, Coskun F, et al. Role of Procalcitonin in Evaluation of the Severity of Acute Cholecystitis. Eurasian Journal Of Medicine [serial on the Internet]. (2016, Oct), [cited March 22, 2017]; 48(3): 162-166. Available from: Academic Search Complete.</ref>. All of these factors increase the risk of post-operative complication<ref name="p4">Terho P, Leppäniemi A, Mentula P. Laparoscopic cholecystectomy for acute calculous cholecystitis: a retrospective study assessing risk factors for conversion and complications. World Journal Of Emergency Surgery [serial on the Internet]. (2016, Nov 16), [cited March 22, 2017]; 111-9. Available from: Academic Search Complete.</ref>. Acute attacks should resolve spontaneously, but a person may experience reoccurences. This may lead to the patient having their gallbladder removed. Old age is a poor prognostic factor as mortality secondary to acute cholecystitis is 5 to 10 percent for clients that are older than 60 and have serious associated diseases<ref>Goodman CC, Fuller K. Pathology Implications for the Physical Therapist Third Edition. Saunders Elsevier: St. Louis; 2009.</ref><ref>ASİLTÜRK LÜLLECİ Z, BAŞYİĞİT S, PİRİNÇÇİ SAPMAZ F, UZMAN M, KEFELİ A, NAZLIGÜL Y, et al. Comparison of ultrasonographic and laboratory findings of acute cholecystitis between elderly and nonelderly patients. Turkish Journal Of Medical Sciences [serial on the Internet]. (2016, Oct), [cited March 21, 2017]; 46(5): 1428-1433. Available from: Academic Search Complete.</ref>. |
| | |
| == Case Reports<ref name="p7" /> ==
| |
| | |
| add links to case studies here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br>
| |
| | |
| Title<br>Cholecystitis Case Report<br> <br>Keywords<br>Cholecystitis, Murphy’s Sign, Musculoskeletal Origin, Systemic Origin, Physical Therapist, Referral<br> <br>Author/s<br>Laura Matrisciano and Spencer Fuehne<br> <br>Abstract<br>A patient is complaining of a musculoskeletal problem (RUE), but has signs and symptoms that could indicate the pain is systemic in origin. This is an example of how physical therapists can effectively handle situations that are not within our scope of practice.<br> <br>Introduction<br>Systemic problems can present with symptoms that are similar to musculoskeletal problems. Sometimes patients have trouble correlating their systemic signs and symptoms to their musculoskeletal signs and symptoms. For example, sometimes a patient may not realize that their stomach pain may be related to their recent onset of shoulder pain. As physical therapists, we are responsible for recognizing if a patient’s pain is coming from a musculoskeletal structure or a visceral source. If it doesn’t follow a musculoskeletal pattern, we need to be able to refer the patient to the proper medical professional. Asking appropriate questions and recognizing clusters of symptoms are an important skill for physical therapists to develop in order to ensure each patient receives the medical attention he or she requires.<br> <br>Case Presentation<br>45-year-old Native American woman reports to your clinic with complaints of an achy pain in her right shoulder. She reports that she also feels the pain along her right scapula and in between her scapulas. Her current pain level is 4/10. The patient can’t remember a specific incident that started causing her shoulder pain, but has been experiencing the pain off and on for the past 3 months. At worst her pain is an 8/10. When asked, she notes that she does tend to experience discomfort in her abdomen with eating. She has had a few episodes of fever, nausea, and vomiting over the past 3 months, but credits that to the “bug that has been going around.” When asked if she saw her PCP for her flu-like symptoms, she said she did not because she didn’t think it was necessary. Pt. reports that she has been feeling full lately, but denies jaundice. She also fails to report on whether or not there have been changes in her stool.<br> <br>Her PMHx include Type 2 Diabetes (diagnosed 5 years ago), she takes a statin to manage her cholesterol levels, and she reports her mother had her gall bladder removed.<br> <br>Objective:<br>• Ht: 5’4”<br>• Wt: 175 pounds<br>• HR: 85bpm<br>• BP: 146/92<br>• Temperature: 99.7 F<br>• Positive Murphy’s Sign<br>• Quick DASH score: 50<br>• FABQ: 10<br>• Shoulder ROM measurements are all normal, movement fails to replicate symptoms<br>• Shoulder strength 5/5 all planes<br> <br>Clinical Impression<br>The physical therapist notices that the patient’s symptoms don’t seem to point toward a musculoskeletal origin. After finding the associated risk factors coupled with a positive Murphy’s Sign, the physical therapist is lead to believe the patient’s pain is originating from a visceral source.<br> <br>Intervention<br>Send clinical findings to patient’s PCP and educate patient on pain management and importance of seeking care from primary provider promptly. <br> <br>Outcomes<br>Patient was suspected of having cholecystitis. Physical therapist will schedule visits for physical therapy pending physician’s assessment of systemic symptoms. <br> <br>Discussion<br>Cholecystitis has symptoms that can mimic musculoskeletal problems, but requires referral to other health professionals before further treatment by physical therapy. Failure to improve with physical therapy may indicate a possible underlying systemic issue. It is important that physical therapists ask prying questions to reveal underlying systemic symptoms that can help determine whether or not a referral is necessary. <br>
| |
|
| |
|
| == Resources <br> == | | == Differential Diagnosis == |
|
| |
|
| The American College of Gastroenterology-www.acg.gi.org<br>National Digestive Disease International Clearinghouse-digestive.niddk.nih.gov<br><br>
| | * Appendicitis |
| | * Biliary colic |
| | * Cholangitis |
| | * Mesenteric ischemia |
| | * Gastritis |
| | * Peptic ulcer disease<ref name=":1" /> |
|
| |
|
| | <br> |
| == References == | | == References == |
|
| |
|