Cauda Equina Syndrome
Original Editor - Laurie Fiegle and Tabitha Korona
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.Clinically Relevant Anatomy
[edit | edit source]
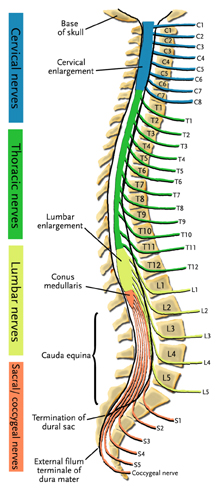
The central nervous system (CNS) includes the brain and spinal cord. The spinal cord allows transmission of signals to and from the brain to allow for movement, sensation, and visceral function. Nerves exiting the spinal cord are divided into sections based on their location of exit, for example, cervical nerves exit the cervical spine and thoracic nerves exit the thoracic spine. The conus medullaris is the distal end of the spinal cord and is usually located at the L1-L2 vertebral level.[1] Nerve roots continue to down the vertebral column after the conus medullaris and are referred to as the cauda equina. The cauda equina includes nerves from lumbar, sacral, and coxxcygeal origins. Being a bundle of nerves, the cauda equina is named for it's resemblance to a horse's tail.
Mechanism of Injury / Pathological Process[edit | edit source]
Cauda equina syndrome can be caused by a number of etiologies but the most common relate to compression of the cauda equina such as a herniated lumbosacral disc, spinal stenosis, and spinal neoplasm. Non-compressive causes include ishemia, infection, and inflammatory conditions. [2]
Ruptured disc, tumor, or fracture can also lead to Cauda equina syndrome. [3]
Clinical Presentation[edit | edit source]
Since the cauda equina nerve roots supply most of the lower extremity (including the pelvic region) sensory and motor innervations, cauda equina syndrome results in multiple motor and sensory signs. [2]
The most common signs and symptoms include bilateral sciatica, saddle region anesthesia, loss of bowel and bladder control, bilateral foot weakness, quadriceps weakness, severe back pain.[4] Other signs and symptoms include decreased sensation between the legs, buttocks, or feet. [3]
Diagnostic Procedures[edit | edit source]
If cauda equina syndrome is expected, medical referral is a necessity to decrease the possibility of permanent damage. Diagnostic procedures used to confirm cauda equina syndrome may include an MRI or myelogram. [5]
Management / Interventions
[edit | edit source]
Cauda equina syndrome is a medical emergency and requires immediate medical referral.
Treatment of cauda equina syndrome is going to vary based on the cause of the symptoms. Surgical decompression may be used if necessary.
Differential Diagnosis
[edit | edit source]
- Conus medullaris syndrome
- Mechanical back pain
- Spinal cord compression
- Spinal tumor
- Lumbar vertebrae fracture
- Peripheral neuropathy
- Herniated Nucleus Pulposis
Key Evidence[edit | edit source]
Cauda equina syndrome is a rare but serious disorder. Prevalence in patients with low back pain is about 4 in 10,000. [6]
Resources
[edit | edit source]
For more information regarding the emergency medical treatment of cauda equina syndrome please see the article entitled "Orthopedic pitfalls:cauda equina syndrome." [6]
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Dutton, M. (2008). Orthopaedic: Examination, evaluation, and intervention (2nd ed.). New York: The McGraw-Hill Companies, Inc.
- ↑ 2.0 2.1 Orendacova J, Cizkova D, Kafka J, Lukacova N, Marsala M, Sulla I, Marsala J, Katsube N. Cauda Equina Syndrome. Progress in Neurobiology 2001;64:613-37.
- ↑ 3.0 3.1 American Academy of Orthopaedic Surgeons, Your Orthopaedic Connection. Cauda Equina Syndrome. http://orthoinfo.aaos.org/topic.cfm?topic=A00362 (accessed 28 May 2009)
- ↑ Shapiro S. Medical Realities of Cauda Equina Syndrome Secondary to Lumbar Disc Herniation. SPINE 2000;25:3, 348-52
- ↑ Ogilvie J. Complications in Spondylolisthesis Surgery. SPINE 2005;30:65 S97-S101
- ↑ 6.0 6.1 Small S, Perron A, Brady W. Orthopedic pitfalls: cauda equina syndrome. The American Journal of Emergency Medicine 2005;23:159-63