Calgary-Cambridge Guide to Communication in the Physical Examination: Difference between revisions
No edit summary |
No edit summary |
||
| (37 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Mariam Hashem|Mariam Hashem]] | '''Original Editor '''- [[User:Mariam Hashem|Mariam Hashem]] based on the course by [https://members.physio-pedia.com/course_tutor/marissa-fourie/ Marissa Fourie]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== Why is communication important? == | |||
</ | [[File:Communication pic.jpg|thumb|225x225px]] | ||
< | Clinical examination is facing a challenge concerning its accuracy and importance. The advancement in research has proven low reliability and validity of many clinical tests with higher rates of accuracy associated with imaging and diagnostic scans. <ref name=":1">Fourie M. Communication in the Physical Examination. Plus Course 2021</ref> However, the perspective changes when the subject is approached from the cost-effectiveness and availability point of view. Restricted geographical access to advanced medical diagnostic tools and the lack of affordability impose limitations on such technologies. Therefore, clinical examination is still a valuable tool in clinical practice. Another issue is the growing use of Clinical video telehealth (CVT), which offers the opportunity to improve access to healthcare providers in medically underserved areas. Still, patients express concerns about CVT hindering their communication with the doctor or physiotherapist.<ref>Gordon HS, Solanki P, Bokhour BG, Gopal RK. [https://link.springer.com/article/10.1007/s11606-020-05673-w “I’m not feeling like I’m part of the conversation” patients’ perspectives on communicating in clinical video telehealth visits.] Journal of general internal medicine. 2020 Jun;35(6):1751-8.</ref> | ||
Despite being the golden standard, laboratory testing and imaging, if misused, could be harmful<ref name=":0">Asif T, Mohiuddin A, Hasan B, Pauly RR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5453739/ Importance of thorough physical examination: a lost art]. Cureus. 2017 May;9(5).</ref> could contribute to overdiagnosis, leading to further psychological and behavioural harms. <ref>Singh H, Dickinson JA, Thériault G, Grad R, Groulx S, Wilson BJ, Szafran O, Bell NR. [https://www.cfp.ca/content/cfp/64/11/816.full.pdf Overdiagnosis: causes and consequences in primary health care]. Canadian Family Physician. 2018 Sep 1;64(9):654-9.</ref> The power of careful hands performing systematic physical examinations still surpasses the technological era.<ref>van Galen LS, Bos PP. [https://sci-hub.se/https://www.ejinme.com/article/S0953-6205(18)30099-2/pdf You can keep your shirt on: A physician's auscultating s(k)in]. European journal of internal medicine. 2018 Jun 1;52:e39-40.</ref> | |||
A thorough and effective physical examination is considered an art that is important for proper diagnosis and builds the patient-physician relationship. Omitting the physical examination is perceived by the patients as insufficient attention. <ref name=":0" /> Interpersonal aspects and good communication increase the patient's satisfaction. <ref>Jalil A, Zakar R, Zakar MZ, Fischer F. [https://link.springer.com/article/10.1186/s12913-017-2094-6 Patient satisfaction with doctor-patient interactions: a mixed-methods study among diabetes mellitus patients in Pakistan.] BMC health services research. 2017 Dec 1;17(1):155.</ref> It is an essential practice that has improved the patient's willingness to engage in treatment. <ref>Kourkouta L, Barsamidis K, Lavdaniti M. [https://www.umb.edu.pl/photo/pliki/progress-file/phs/phs_2013_1/119_-122_kourkouta.pdf Communication skills during the clinical examination of the patients.] Progress in Health Sciences. 2013;3(1):119.</ref> A study by Hinchliffe and Lavin <ref>Hinchliffe NC, Lavin N. [https://www.umb.edu.pl/photo/pliki/progress-file/phs/phs_2013_1/119_-122_kourkouta.pdf Why do patients with low back pain choose not to engage with physiotherapy following assessment?] International Journal of Therapy & Rehabilitation. 2018 Mar 2;25(3): 120-127.</ref> found the physiotherapist's communication with the ''patient to be a key factor in patients' satisfaction and compliance with the management plan.'' | |||
[[File:Benefits of Effective Communication Table.jpg|center|thumb|600x600px]] | |||
Communicating effectively with patients improves the effectiveness of the consultation, shows supportiveness and collaboration, and reduces conflicts and complaints. Health Care professionals, including physiotherapists, recognise that good communication skills can improve adherence, patient confidence and other psychosocial patient outcomes. <ref>Soundy A, Hemmings L, Gardiner L, Rosewilliam S, Heneghan NR, Cronin K, Reid K. E-learning communication skills training for physiotherapy students: A two-phased sequential mixed methods study. Patient education and counselling. 2021 Aug 1;104(8):2045-53.</ref> The advantages of good communication are not exclusive to patients. Clinician satisfaction, understanding and recall are also enhanced when the clinician engages in well-intentioned communication. <ref name=":3" /> | |||
'''Communication is a set of procedures for improving care outcomes. Good communication is a learned skill rather than a personality trait.''' <ref name=":3">Kurtz SM. [https://www.cambridge.org/core/services/aop-cambridge-core/content/view/23808049F33114BFA988142C35910AA8/S0317167100001906a.pdf/div-class-title-doctor-patient-communication-principles-and-practices-div.pdf Doctor-patient communication: principles and practices.] Canadian Journal of Neurological Sciences. 2002;29(S2):S23-9.</ref> | |||
Learning to communicate effectively is similar to becoming a professional tennis player. Mastering the sport requires being specific and focusing on skills and strategies. Like any other skill, patient-centred communication will deteriorate if you stop practising it. Experience, although a habit reinforcer, tends not to discern very carefully between good and bad habits. <ref name=":3" /> | |||
== Calgary–Cambridge Model == | |||
The [[Calgary-Cambridge Guide to the Medical Interview - Initiating the Session|Calgary–Cambridge model]] was developed in 1996. <ref>Kurtz, S.M., Silverman, J.D.. [https://psycnet.apa.org/record/1996-04140-001 The Calgary-Cambridge Referenced Observation Guides: an aid to defining the curriculum and organizing the teaching in communication training programmes]. Med. Educ. 1996 30, 83–89.</ref> It is a practical model that incorporates the consultation's physical, psychological and social aspects. The model encourages note-taking in a way that does not interfere with demonstrating interest and empathy. This model is not an assessment tool but a guide to assess specific communication skills and provide feedback.<ref>Iversen ED, Wolderslund MO, Kofoed PE, Gulbrandsen P, Poulsen H, Cold S, Ammentorp J. [https://link.springer.com/article/10.1186/s12909-020-02050-3 Codebook for rating clinical communication skills based on the Calgary-Cambridge Guide]. BMC Medical Education. 2020 Dec;20(1):1-9.</ref> | |||
The model also encourages sharing thoughts with the patient by thinking aloud and accepting the patient's narrative. | |||
[[File:Layout of the Calgary-Cambridge Model- Detailed, with objectives.png|thumb|500x500px]] | |||
It provides a structure to ensure a smooth consultation flow by placing the patient at the centre to make them feel in control. <ref name=":5">Denness C. [https://www.frontiersin.org/articles/10.3389/fneur.2020.00465/full What are consultation models for?]. InnovAit. 2013 Sep;6(9):592-9.</ref> | |||
''' | '''Stages of consultation according to the Calgary-Cambridge model:''' | ||
* ''' Initiating the Session''': this stage aims to establish a rapport and understand the reasons for the consultation. | |||
* '''Gathering Information''': asking open and closed questions, picking up on cues and exploring the patient’s ideas, concerns and expectations. In this stage, the clinician develops a structure of the consultation that runs to the end of the session and ensures the flow of the process | |||
* ''' Physical Examination''': will be discussed in more depth later in this article. | |||
* ''' Explanation and Planning''': discuss the treatment plan and check the patient's understanding. Written materials, infographics and related information leaflets are recommended to ensure clarity of explanation. | |||
* ''' Close the Session''' by summarising and ensuring that the agreed plan is clear. <ref name=":5" /> | |||
[[File:Relationship between content and process Calgary.gif|thumb|500x500px]] | |||
== How to Become a Good Communicator? == | |||
An effective communicator is "proactive, polite, imaginative, innovative, creative, constructive, professional, progressive, energetic, enabling, transparent and technology friendly".<ref>Reddy BV, Gupta A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7586512/pdf/JFMPC-9-3793.pdf Importance of effective communication during COVID-19 infodemic. Journal of Family Medicine and Primary Care.] 2020 Aug;9(8):3793.</ref> Five essential elements have been described for enhancing communication skills: <ref name=":3" /> | |||
* Learn the systematic delineation and definition of skills | |||
* Observe learners performing skills (e.g. clinical supervision, shadowing colleagues and experts) | |||
* Ask for detailed feedback | |||
* Practice and rehearse your learned skills | |||
* Repeat the process | |||
A study by King & Hoppe<ref>King A, Hoppe RB. [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-020-02123-3 “Best practice” for patient-centred communication: a narrative review.] Journal of graduate medical education. 2013 Sep;5(3):385-93.</ref> described the best practice for patient-centred care in the following table (adapted from [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5874557/ Patient-Centred Communication study by Naughton:]<ref name=":4" /> | |||
{| class="wikitable" | {| class="wikitable" | ||
|'''Goal''' | |'''Goal''' | ||
|''' | |'''Clinician's Responsibility''' | ||
|'''Communication Skills''' | |'''Communication Skills''' | ||
|- | |- | ||
|Foster the | |Foster the clinician-patient | ||
relationship | |||
|Build rapport | |Build rapport | ||
Appear open | Appear open | ||
Demonstrate respect | Demonstrate respect, caring and commitment | ||
Acknowledge feelings and emotions | Acknowledge feelings and emotions | ||
|Greet patient warmly and appropriately | |Greet the patient warmly and appropriately | ||
Maintain eye contact | Maintain eye contact | ||
| Line 46: | Line 68: | ||
|- | |- | ||
|Gather Information | |Gather Information | ||
|Determine purpose of | |Determine the purpose of the visit | ||
Explore physiological symptoms (disease) | |||
Understand patient perspective (illness) | Understand the patient perspective (illness) | ||
|Ask open-ended questions | |Ask open-ended questions | ||
Allow patient to complete responses | Allow the patient to complete responses (listen) | ||
Clarify and summarize information | Clarify and summarize information | ||
Explore impact of illness on patient | Explore the impact of illness on the patient | ||
|- | |- | ||
|Provide Information | |Provide Information | ||
| Line 66: | Line 88: | ||
Overcome health literacy barriers | Overcome health literacy barriers | ||
|Speak plainly and avoid jargon | |Speak plainly and avoid jargon | ||
Encourage questions | Encourage questions | ||
| Line 73: | Line 93: | ||
Check for understanding | Check for understanding | ||
|- | |- | ||
| | |Shared Decision-Making | ||
|Identify patient goals | |Identify patient goals | ||
Outline collaborative treatment plan | Outline a collaborative treatment plan | ||
|Explore patient preferences | |Explore patient preferences | ||
Identify barriers to treatment choices | Identify barriers to treatment choices. | ||
Negotiate agreement | Negotiate agreement | ||
| Line 88: | Line 108: | ||
Arrange for needed support | Arrange for needed support | ||
Advocate for and assist | Advocate for and assist patients with the health system | ||
|Summarize treatment plan | |Summarize the treatment plan | ||
Elicit patient understanding | Elicit patient understanding | ||
Discuss follow-up | Discuss follow-up | ||
|} | |} | ||
== Efficient Communication in the Physical Examination == | |||
Unlike [[Gathering Information - Underpinning Biomedical History|subjective history taking]], where the patient plays an active role, the patient's role changes during the physical examination. <ref name=":1" /> The clinician can make this process easier by guiding the patients throughout, knowing that patients start the examination with some uncertainty. Your patient needs to understand the process and follow your train of thought. | |||
'''The followings are considerations and tips on good communication skills to guide you through the physical examination process:''' <ref name=":1" /> | |||
==== Signposting ==== | |||
Signposting involves informing the patient of what you are about to say or do to help them feel less anxious and give them a sense of control. This is achieved by providing a concise summary of the last step and the following step of the assessment<ref>Nursing on the Move. [https://www.goinginternational.eu/wp/de/communication-tips-directive-skills-signposting/#:~:text=A%20signpost%20is%20an%20explicit,what%20is%20going%20to%20happen. Communication Tips- Directive Skills: Signposting]. 2016. </ref>, for example, following the subjective history taking of a Musculoskeletal (MSK) condition, the clinician can signpost by saying:<ref name=":1" /> | |||
''"With all the information you have given me, I have some ideas about what might cause your discomfort. We will now move on to the physical examination to try and narrow down the underlying structures responsible for your symptoms. I first want to assess how you move in general and then simultaneously check for the possible involvement of your vertebral joints, muscles, and nerves in your back pain. I'm going to guide you into doing a couple of movements, and whenever you feel your familiar pain, I would like you to tell me and then move out of the uncomfortable position."'' | |||
With all the information you have given me, I have | |||
This gives a framework for the patient, informing them of what information we gained from the interview, what should they expect next and what feedback is expected from them. | This gives a framework for the patient, informing them of what information we gained from the interview, what should they expect next and what feedback is expected from them. | ||
==== Touch ==== | |||
Touch involves a professional feel and is an expression of care and sympathy. <ref name=":2">Kelly MA, Nixon L, McClurg C, Scherpbier A, King N, Dornan T. [https://journals.sagepub.com/doi/epub/10.1177/1049732317707726 Experience of touch in health care: a meta-ethnography across the health care professions.] Qualitative health research. 2018 Jan;28(2):200-12.</ref> Palpation has always been considered a powerful diagnostic tool. In physiotherapy, touch provides a safe space and empowers exercises and symptom modification. Touching provides professionals with the means to communicate “beyond words”. <ref>Mengshoel AM, Bjorbækmo WS, Sallinen M, Wahl AK. [https://www.tandfonline.com/doi/epdf/10.1080/09593985.2019.1616343?needAccess=true&role=button 'It takes time, but recovering makes it worthwhile'- A qualitative study of long-term users' experiences of physiotherapy in primary health care.] Physiother Theory Pract. 2021 Jan;37(1):6-16. </ref> It benefits patients in distress, particularly if verbal communication is limited, and for some patients, it has emotional and spiritual meaning. Touch, however, also involves potential complications if perceived as improper and unprofessional, imposing challenges to a core clinical skill. <ref>Feilchenfeld Z, Dornan T, Whitehead C, Kuper A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7045541/pdf/BC-6-38.pdf Ultrasound in undergraduate medical education: a systematic and critical review.] Medical education. 2017 Apr;51(4):366-78.</ref> Palpation of sensitive areas, such as the genitals, or when the examined area is not directly correlated with the main area of complaint, can make patients feel uncomfortable and protective of their personal space. Caution should be observed to respect cultural sensitivities and approach certain populations, such as paediatrics and patients from the opposite sex, especially in the case of a male clinician with a female patient. <ref name=":1" /> | |||
Clinicians should be mindful of the personal space of their patients, show respect and remain cautious of the patient's preference in terms of personal preference, culture, gender, age, etc. They must decide if, when, and how to touch as they negotiate personal and professional boundaries specific to each patient. <ref name=":2" /> | |||
[https://physio-pedia.com/Informed_Consent?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Ask for permission to touch,] even if the patient expects you to touch them. It is ethical and humane to respect the patient's personal space. | |||
==== Undressing ==== | |||
While most patients might be comfortable and understand undressing for the examination, some might be reserved. Informing patients ahead of the interview that they might need to undress is advisable to help ease the process. You might also want to inform patients verbally and get them to agree before starting the examination. | |||
' | Before asking the patient to undress, determine the need for undressing and how much should be exposed. If you sense their discomfort, you can offer a towel or a gown to minimise exposed areas. All patients have the right to privacy and dignity<ref name=":6">Johnson GM, Little R, Staufenberg A, McDonald A, Taylor KG. [https://www.researchgate.net/profile/Rebekah-Little/publication/308006344_How_do_they_feel_Patients%27_perspectives_on_draping_and_dignity_in_a_physiotherapy_outpatient_setting_A_pilot_study/links/5d898223a6fdcc8fd61b02e2/How-do-they-feel-Patients-perspectives-on-draping-and-dignity-in-a-physiotherapy-outpatient-setting-A-pilot-study.pdf How do they feel? Patients' perspectives on draping and dignity in a physiotherapy outpatient setting: A pilot study]. Manual therapy. 2016 Dec 1;26:192-200.</ref> and therefore have the right to refuse to undress. In this case, it is unethical to put pressure on or insist that patients undress but explain to them, with respect, that insufficient exposure of the body can lead to clinical error and increases the risk of a faulty diagnosis or substandard management. <ref name=":1" /> Properly draping patients and providing gowns or shorts are good alternatives to undressing and help patients feel more comfortable. <ref name=":6" /> | ||
==== Briefly summarising ==== | |||
Briefly summarise the preliminary clinical hypothesis using easily understood terminology while considering that the summary is inconclusive. Following the interview, discuss the preliminary hypothesis with your patient to inform them what you need to test and do you need to rule out using short, uncomplicated sentences. | |||
Refrain from using jargon. | Patients have the right to discontinue the process at any time, and it's a good practice to inform them that they have the right to do so. They can take a more active role by asking you questions or adding more information during the examination. Refrain from using jargon. The specific movement command should be clear and easy to understand using verbal instruction, physical demonstration, manual facilitation, or a combination. | ||
The tone used to communicate is also essential, and the therapist should refrain from using an authoritative parental tone. Give your patient the space to ask for clarifications if they don't understand the command. This is particularly relevant in remote consultations done over the phone. | |||
According to the National Assessment of Adult Literacy, only 12% of adults have proficient health literacy. In other words, 9 out of 10 adults may lack the skills to manage their health and prevent disease. Healthcare professionals tend to overestimate the patients´ health literacy, and the information thane share with patients may be difficult for them to understand. <ref>Voigt-Barbarowicz M, Brütt AL. [https://www.mdpi.com/1660-4601/17/7/2372 The agreement between patients and healthcare professionals’ assessment of patient’s health literacy—A systematic review.] International journal of environmental research and public health. 2020 Apr;17(7):2372.</ref> It might help to assume all patients as having low health literacy and slow down, speak in plain, non-medical language and use appropriate communication techniques that ensure understanding. | |||
Allow time for patients and their families to ask questions by asking, “What questions do you have?” instead of “Do you have any questions?”. Check the understanding of a patient by asking them to rephrase it in their own words, not just repeat it, to ensure the message is understood. <ref name=":4">Naughton CA. [https://www.frontiersin.org/articles/10.3389/fneur.2020.00465/full Patient-centred communication.] Pharmacy. 2018 Mar;6(1):18.</ref> | |||
For example, a patient performing lumbar side flexion but instead they do a combination of forward | ==== Avoid the negating mode ==== | ||
Avoid the negating mode when correcting a patient's pattern of movement. Avoid using statements like "no, not like that!". Instead, employ positive affirmations and provide feedback. For example, a patient is performing lumbar side flexion, but instead of side flexion, they do a combination of forward and side flexion. To boost your patient's confidence and enhance their motivation, your response might be: "Good job, I want you to repeat the movement, this time focusing on going more sideways. Yes, that looks better." | |||
Using positive affirmation while giving feedback without highlighting the error enhances the patient's confidence in the performance of the movement<ref name=":1" />You might need to rephrase your command or describe in simpler terms to facilitate the patient's understanding of the performance of the correct movement. For example | Using '''positive affirmation''' while giving feedback without highlighting the error enhances the patient's confidence in the performance of the movement<ref name=":1" />. You might need to rephrase your command or describe it in simpler terms to facilitate the patient's understanding of the performance of the correct movement. For example, instead of telling the patient to move purely sideways, you might ask the patient to repeat the movement, sliding the hand down the side of the leg as far as possible. This technique is particularly helpful with patients who are showing some anxiety or low levels of cognition. | ||
==== Treating Minors ==== | |||
Parental consent is a legal requirement for the treatment of children. <ref>Alderson P. [https://discovery.ucl.ac.uk/id/eprint/1544062/1/Alderson_Children%27s_consent.pdf Children’s consent and the zone of parental discretion]. Clinical Ethics. 2017 Jun;12(2):55-62.</ref> Parents are invaluable in facilitating the approach and treatment delivery. They can be engaged in the session by asking the parent to assist the child and explain the commands so the child can understand. | |||
Feedback | ==== Feedback ==== | ||
Continuous feedback throughout the assessment is another way to practice good communication. Some patients might feel embarrassed and exposed, especially when they don't understand the relevance of their movements during the examination. Providing feedback and explaining the findings can ease the patient's discomfort. It is good practice to share positive findings instead of only focusing on problems. This lowers the anxiety factor and gives the patient some positive affirmation regarding their movement and body while breaking down the idea of frailty.{{#ev:youtube|S4wWClQhZaA|300}}<ref>Communication Skills: A Patient-Centered Approach . Available from:https://www.youtube.com/watch?v=S4wWClQhZaA[last accessed 18/01/2021]</ref> | |||
== References == | == References == | ||
| Line 176: | Line 167: | ||
[[Category:Assessment]] | [[Category:Assessment]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Plus Content]] | |||
[[Category:Professional Issues]] | [[Category:Professional Issues]] | ||
[[Category:Communication]] | [[Category:Communication]] | ||
Latest revision as of 21:07, 6 January 2023
Original Editor - Mariam Hashem based on the course by Marissa Fourie
Why is communication important?[edit | edit source]
Clinical examination is facing a challenge concerning its accuracy and importance. The advancement in research has proven low reliability and validity of many clinical tests with higher rates of accuracy associated with imaging and diagnostic scans. [1] However, the perspective changes when the subject is approached from the cost-effectiveness and availability point of view. Restricted geographical access to advanced medical diagnostic tools and the lack of affordability impose limitations on such technologies. Therefore, clinical examination is still a valuable tool in clinical practice. Another issue is the growing use of Clinical video telehealth (CVT), which offers the opportunity to improve access to healthcare providers in medically underserved areas. Still, patients express concerns about CVT hindering their communication with the doctor or physiotherapist.[2]
Despite being the golden standard, laboratory testing and imaging, if misused, could be harmful[3] could contribute to overdiagnosis, leading to further psychological and behavioural harms. [4] The power of careful hands performing systematic physical examinations still surpasses the technological era.[5]
A thorough and effective physical examination is considered an art that is important for proper diagnosis and builds the patient-physician relationship. Omitting the physical examination is perceived by the patients as insufficient attention. [3] Interpersonal aspects and good communication increase the patient's satisfaction. [6] It is an essential practice that has improved the patient's willingness to engage in treatment. [7] A study by Hinchliffe and Lavin [8] found the physiotherapist's communication with the patient to be a key factor in patients' satisfaction and compliance with the management plan.
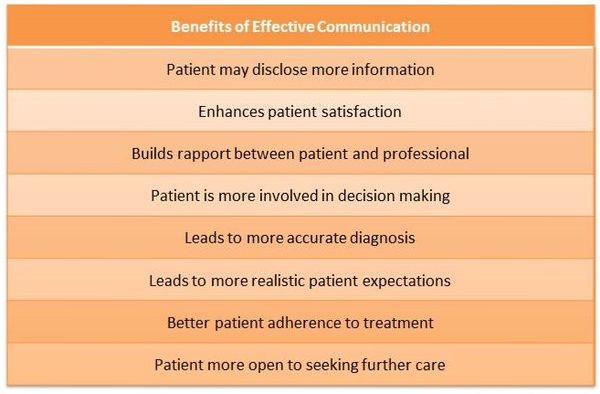
Communicating effectively with patients improves the effectiveness of the consultation, shows supportiveness and collaboration, and reduces conflicts and complaints. Health Care professionals, including physiotherapists, recognise that good communication skills can improve adherence, patient confidence and other psychosocial patient outcomes. [9] The advantages of good communication are not exclusive to patients. Clinician satisfaction, understanding and recall are also enhanced when the clinician engages in well-intentioned communication. [10]
Communication is a set of procedures for improving care outcomes. Good communication is a learned skill rather than a personality trait. [10]
Learning to communicate effectively is similar to becoming a professional tennis player. Mastering the sport requires being specific and focusing on skills and strategies. Like any other skill, patient-centred communication will deteriorate if you stop practising it. Experience, although a habit reinforcer, tends not to discern very carefully between good and bad habits. [10]
Calgary–Cambridge Model [edit | edit source]
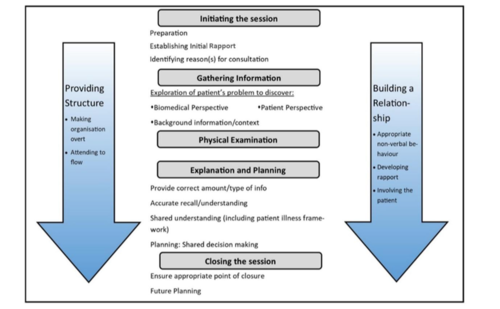
The Calgary–Cambridge model was developed in 1996. [11] It is a practical model that incorporates the consultation's physical, psychological and social aspects. The model encourages note-taking in a way that does not interfere with demonstrating interest and empathy. This model is not an assessment tool but a guide to assess specific communication skills and provide feedback.[12]
The model also encourages sharing thoughts with the patient by thinking aloud and accepting the patient's narrative.
It provides a structure to ensure a smooth consultation flow by placing the patient at the centre to make them feel in control. [13]
Stages of consultation according to the Calgary-Cambridge model:
- Initiating the Session: this stage aims to establish a rapport and understand the reasons for the consultation.
- Gathering Information: asking open and closed questions, picking up on cues and exploring the patient’s ideas, concerns and expectations. In this stage, the clinician develops a structure of the consultation that runs to the end of the session and ensures the flow of the process
- Physical Examination: will be discussed in more depth later in this article.
- Explanation and Planning: discuss the treatment plan and check the patient's understanding. Written materials, infographics and related information leaflets are recommended to ensure clarity of explanation.
- Close the Session by summarising and ensuring that the agreed plan is clear. [13]
How to Become a Good Communicator?[edit | edit source]
An effective communicator is "proactive, polite, imaginative, innovative, creative, constructive, professional, progressive, energetic, enabling, transparent and technology friendly".[14] Five essential elements have been described for enhancing communication skills: [10]
- Learn the systematic delineation and definition of skills
- Observe learners performing skills (e.g. clinical supervision, shadowing colleagues and experts)
- Ask for detailed feedback
- Practice and rehearse your learned skills
- Repeat the process
A study by King & Hoppe[15] described the best practice for patient-centred care in the following table (adapted from Patient-Centred Communication study by Naughton:[16]
| Goal | Clinician's Responsibility | Communication Skills |
| Foster the clinician-patient
relationship |
Build rapport
Appear open Demonstrate respect, caring and commitment Acknowledge feelings and emotions |
Greet the patient warmly and appropriately
Maintain eye contact Show interest Listen actively Express empathy |
| Gather Information | Determine the purpose of the visit
Explore physiological symptoms (disease) Understand the patient perspective (illness) |
Ask open-ended questions
Allow the patient to complete responses (listen) Clarify and summarize information Explore the impact of illness on the patient |
| Provide Information | Identify patient informational needs
Share information Overcome health literacy barriers |
Speak plainly and avoid jargon
Encourage questions Check for understanding |
| Shared Decision-Making | Identify patient goals
Outline a collaborative treatment plan |
Explore patient preferences
Identify barriers to treatment choices. Negotiate agreement |
| Enable Treatment Success | Assess the patient’s capacity for self-management
Arrange for needed support Advocate for and assist patients with the health system |
Summarize the treatment plan
Elicit patient understanding Discuss follow-up |
Efficient Communication in the Physical Examination[edit | edit source]
Unlike subjective history taking, where the patient plays an active role, the patient's role changes during the physical examination. [1] The clinician can make this process easier by guiding the patients throughout, knowing that patients start the examination with some uncertainty. Your patient needs to understand the process and follow your train of thought.
The followings are considerations and tips on good communication skills to guide you through the physical examination process: [1]
Signposting[edit | edit source]
Signposting involves informing the patient of what you are about to say or do to help them feel less anxious and give them a sense of control. This is achieved by providing a concise summary of the last step and the following step of the assessment[17], for example, following the subjective history taking of a Musculoskeletal (MSK) condition, the clinician can signpost by saying:[1]
"With all the information you have given me, I have some ideas about what might cause your discomfort. We will now move on to the physical examination to try and narrow down the underlying structures responsible for your symptoms. I first want to assess how you move in general and then simultaneously check for the possible involvement of your vertebral joints, muscles, and nerves in your back pain. I'm going to guide you into doing a couple of movements, and whenever you feel your familiar pain, I would like you to tell me and then move out of the uncomfortable position."
This gives a framework for the patient, informing them of what information we gained from the interview, what should they expect next and what feedback is expected from them.
Touch[edit | edit source]
Touch involves a professional feel and is an expression of care and sympathy. [18] Palpation has always been considered a powerful diagnostic tool. In physiotherapy, touch provides a safe space and empowers exercises and symptom modification. Touching provides professionals with the means to communicate “beyond words”. [19] It benefits patients in distress, particularly if verbal communication is limited, and for some patients, it has emotional and spiritual meaning. Touch, however, also involves potential complications if perceived as improper and unprofessional, imposing challenges to a core clinical skill. [20] Palpation of sensitive areas, such as the genitals, or when the examined area is not directly correlated with the main area of complaint, can make patients feel uncomfortable and protective of their personal space. Caution should be observed to respect cultural sensitivities and approach certain populations, such as paediatrics and patients from the opposite sex, especially in the case of a male clinician with a female patient. [1]
Clinicians should be mindful of the personal space of their patients, show respect and remain cautious of the patient's preference in terms of personal preference, culture, gender, age, etc. They must decide if, when, and how to touch as they negotiate personal and professional boundaries specific to each patient. [18]
Ask for permission to touch, even if the patient expects you to touch them. It is ethical and humane to respect the patient's personal space.
Undressing[edit | edit source]
While most patients might be comfortable and understand undressing for the examination, some might be reserved. Informing patients ahead of the interview that they might need to undress is advisable to help ease the process. You might also want to inform patients verbally and get them to agree before starting the examination.
Before asking the patient to undress, determine the need for undressing and how much should be exposed. If you sense their discomfort, you can offer a towel or a gown to minimise exposed areas. All patients have the right to privacy and dignity[21] and therefore have the right to refuse to undress. In this case, it is unethical to put pressure on or insist that patients undress but explain to them, with respect, that insufficient exposure of the body can lead to clinical error and increases the risk of a faulty diagnosis or substandard management. [1] Properly draping patients and providing gowns or shorts are good alternatives to undressing and help patients feel more comfortable. [21]
Briefly summarising[edit | edit source]
Briefly summarise the preliminary clinical hypothesis using easily understood terminology while considering that the summary is inconclusive. Following the interview, discuss the preliminary hypothesis with your patient to inform them what you need to test and do you need to rule out using short, uncomplicated sentences.
Patients have the right to discontinue the process at any time, and it's a good practice to inform them that they have the right to do so. They can take a more active role by asking you questions or adding more information during the examination. Refrain from using jargon. The specific movement command should be clear and easy to understand using verbal instruction, physical demonstration, manual facilitation, or a combination.
The tone used to communicate is also essential, and the therapist should refrain from using an authoritative parental tone. Give your patient the space to ask for clarifications if they don't understand the command. This is particularly relevant in remote consultations done over the phone.
According to the National Assessment of Adult Literacy, only 12% of adults have proficient health literacy. In other words, 9 out of 10 adults may lack the skills to manage their health and prevent disease. Healthcare professionals tend to overestimate the patients´ health literacy, and the information thane share with patients may be difficult for them to understand. [22] It might help to assume all patients as having low health literacy and slow down, speak in plain, non-medical language and use appropriate communication techniques that ensure understanding.
Allow time for patients and their families to ask questions by asking, “What questions do you have?” instead of “Do you have any questions?”. Check the understanding of a patient by asking them to rephrase it in their own words, not just repeat it, to ensure the message is understood. [16]
Avoid the negating mode[edit | edit source]
Avoid the negating mode when correcting a patient's pattern of movement. Avoid using statements like "no, not like that!". Instead, employ positive affirmations and provide feedback. For example, a patient is performing lumbar side flexion, but instead of side flexion, they do a combination of forward and side flexion. To boost your patient's confidence and enhance their motivation, your response might be: "Good job, I want you to repeat the movement, this time focusing on going more sideways. Yes, that looks better."
Using positive affirmation while giving feedback without highlighting the error enhances the patient's confidence in the performance of the movement[1]. You might need to rephrase your command or describe it in simpler terms to facilitate the patient's understanding of the performance of the correct movement. For example, instead of telling the patient to move purely sideways, you might ask the patient to repeat the movement, sliding the hand down the side of the leg as far as possible. This technique is particularly helpful with patients who are showing some anxiety or low levels of cognition.
Treating Minors[edit | edit source]
Parental consent is a legal requirement for the treatment of children. [23] Parents are invaluable in facilitating the approach and treatment delivery. They can be engaged in the session by asking the parent to assist the child and explain the commands so the child can understand.
Feedback[edit | edit source]
Continuous feedback throughout the assessment is another way to practice good communication. Some patients might feel embarrassed and exposed, especially when they don't understand the relevance of their movements during the examination. Providing feedback and explaining the findings can ease the patient's discomfort. It is good practice to share positive findings instead of only focusing on problems. This lowers the anxiety factor and gives the patient some positive affirmation regarding their movement and body while breaking down the idea of frailty.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Fourie M. Communication in the Physical Examination. Plus Course 2021
- ↑ Gordon HS, Solanki P, Bokhour BG, Gopal RK. “I’m not feeling like I’m part of the conversation” patients’ perspectives on communicating in clinical video telehealth visits. Journal of general internal medicine. 2020 Jun;35(6):1751-8.
- ↑ 3.0 3.1 Asif T, Mohiuddin A, Hasan B, Pauly RR. Importance of thorough physical examination: a lost art. Cureus. 2017 May;9(5).
- ↑ Singh H, Dickinson JA, Thériault G, Grad R, Groulx S, Wilson BJ, Szafran O, Bell NR. Overdiagnosis: causes and consequences in primary health care. Canadian Family Physician. 2018 Sep 1;64(9):654-9.
- ↑ van Galen LS, Bos PP. You can keep your shirt on: A physician's auscultating s(k)in. European journal of internal medicine. 2018 Jun 1;52:e39-40.
- ↑ Jalil A, Zakar R, Zakar MZ, Fischer F. Patient satisfaction with doctor-patient interactions: a mixed-methods study among diabetes mellitus patients in Pakistan. BMC health services research. 2017 Dec 1;17(1):155.
- ↑ Kourkouta L, Barsamidis K, Lavdaniti M. Communication skills during the clinical examination of the patients. Progress in Health Sciences. 2013;3(1):119.
- ↑ Hinchliffe NC, Lavin N. Why do patients with low back pain choose not to engage with physiotherapy following assessment? International Journal of Therapy & Rehabilitation. 2018 Mar 2;25(3): 120-127.
- ↑ Soundy A, Hemmings L, Gardiner L, Rosewilliam S, Heneghan NR, Cronin K, Reid K. E-learning communication skills training for physiotherapy students: A two-phased sequential mixed methods study. Patient education and counselling. 2021 Aug 1;104(8):2045-53.
- ↑ 10.0 10.1 10.2 10.3 Kurtz SM. Doctor-patient communication: principles and practices. Canadian Journal of Neurological Sciences. 2002;29(S2):S23-9.
- ↑ Kurtz, S.M., Silverman, J.D.. The Calgary-Cambridge Referenced Observation Guides: an aid to defining the curriculum and organizing the teaching in communication training programmes. Med. Educ. 1996 30, 83–89.
- ↑ Iversen ED, Wolderslund MO, Kofoed PE, Gulbrandsen P, Poulsen H, Cold S, Ammentorp J. Codebook for rating clinical communication skills based on the Calgary-Cambridge Guide. BMC Medical Education. 2020 Dec;20(1):1-9.
- ↑ 13.0 13.1 Denness C. What are consultation models for?. InnovAit. 2013 Sep;6(9):592-9.
- ↑ Reddy BV, Gupta A. Importance of effective communication during COVID-19 infodemic. Journal of Family Medicine and Primary Care. 2020 Aug;9(8):3793.
- ↑ King A, Hoppe RB. “Best practice” for patient-centred communication: a narrative review. Journal of graduate medical education. 2013 Sep;5(3):385-93.
- ↑ 16.0 16.1 Naughton CA. Patient-centred communication. Pharmacy. 2018 Mar;6(1):18.
- ↑ Nursing on the Move. Communication Tips- Directive Skills: Signposting. 2016.
- ↑ 18.0 18.1 Kelly MA, Nixon L, McClurg C, Scherpbier A, King N, Dornan T. Experience of touch in health care: a meta-ethnography across the health care professions. Qualitative health research. 2018 Jan;28(2):200-12.
- ↑ Mengshoel AM, Bjorbækmo WS, Sallinen M, Wahl AK. 'It takes time, but recovering makes it worthwhile'- A qualitative study of long-term users' experiences of physiotherapy in primary health care. Physiother Theory Pract. 2021 Jan;37(1):6-16.
- ↑ Feilchenfeld Z, Dornan T, Whitehead C, Kuper A. Ultrasound in undergraduate medical education: a systematic and critical review. Medical education. 2017 Apr;51(4):366-78.
- ↑ 21.0 21.1 Johnson GM, Little R, Staufenberg A, McDonald A, Taylor KG. How do they feel? Patients' perspectives on draping and dignity in a physiotherapy outpatient setting: A pilot study. Manual therapy. 2016 Dec 1;26:192-200.
- ↑ Voigt-Barbarowicz M, Brütt AL. The agreement between patients and healthcare professionals’ assessment of patient’s health literacy—A systematic review. International journal of environmental research and public health. 2020 Apr;17(7):2372.
- ↑ Alderson P. Children’s consent and the zone of parental discretion. Clinical Ethics. 2017 Jun;12(2):55-62.
- ↑ Communication Skills: A Patient-Centered Approach . Available from:https://www.youtube.com/watch?v=S4wWClQhZaA[last accessed 18/01/2021]