Calcaneal Fractures: Difference between revisions
Kim Jackson (talk | contribs) m (Text replacement - "''' ==" to "==") |
(Added photos) |
||
| (28 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> '''Original Editor '''- [[User:Hajar Abdelhadji, Roxann Musimu, Dylan Van Calck|Hajar Abdelhadji, Roxann Musimu, Dylan Van Calck]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
'''Original Editor '''- | |||
== Definition / Description == | == Definition / Description == | ||
[[File:Radiological image of calcaneus fracture( lateral view).png|thumb|Radiological image of calcaneus fracture( lateral view)]] | |||
A calcaneus fracture is a heel bone fracture. | A [[calcaneus]] fracture is a heel bone fracture. It is a rare type of fracture but has potentially debilitating results. Traditionally, a burst fracture of the calcaneus was known as '''"Lovers Fracture"''' as the injury would occur as a suitor would jump off a lover's balcony (axial loading) to avoid detection.<ref name=":2">Davis D, Newton EJ. [https://www.ncbi.nlm.nih.gov/books/NBK430861/ Calcaneus Fractures.]</ref> <br> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
A | A good understanding of the anatomy of the calcaneus is essential in determining the patterns of injury and treatment goals and options. | ||
Calcaneus is the largest talar bone out of 7 [[Foot Anatomy|tarsal]] bones which together with the talus form hind-foot. The calcaneus has a relatively thin cortex. It has 4 facets: 1 anteriorly which articulate with cuboid forming calcaneocuboid joint and 3 superiorly (anterior, middle, and posterior, with the posterior facet representing the major weight-bearing surface) which articulate with talus forming talocalcaneal joint (subtalar joint). Subtalar joint allows inversion and eversion of the foot.<ref name=":6" /><ref name=":2" /> | |||
< | The interosseous ligament and medial, lateral, and posterior talocalcaneal ligaments provide additional support for the joint. The sustentaculum tali is a medial bony projection supporting the neck of the talus. The tibial artery, nerve, [[Tibialis Posterior|posterior tibial tendon]], and [[flexor hallucis longus]] tendon are located medially to the calcaneus and are at risk for impingement with a calcaneal fracture and, as are the [[Peroneus (Fibularis) Longus Muscle|peroneal]] tendons located on the lateral aspect of the calcaneus. This also makes surgical approach challenging. The lateral side of the calcaneus and its flat nature is highlighted as the most advantageous for internal fixation, but the poor soft tissue cover challenges wound healing.<ref name=":1">Daftary A, Haims AH, Baumgaertner MR. [https://pubs.rsna.org/doi/full/10.1148/rg.255045713 Fractures of the calcaneus: a review with emphasis on CT.] Radiographics. 2005 Sep;25(5):1215-26.</ref>These anatomic landmarks are important because fractures associated with these areas may cause involve joint involvement, tendon and neurovascular injury.<ref name=":1" /> | ||
== | The calcaneus has four important functions: | ||
# Acts as a foundation and support for the body’s weight | |||
# Supports the lateral column of the foot and acts as the main articulation for inversion/eversion | |||
# Acts as a lever arm for the gastrocnemius muscle complex | |||
# Makes normal walking possible | |||
== Epidemiology/Etiology == | |||
* Calcaneal fractures account for 1-2% of all fractures<ref name=":8">Galluzzo M, Greco F, Pietragalla M, De Renzis A, Carbone M, Zappia M, Maggialetti N, D'andrea A, Caracchini G, Miele V. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6179077/ Calcaneal fractures: radiological and CT evaluation and classification systems.] Acta Biomed. 2018 Jan 19;89(1-S):138-150.</ref> and 60% of tarsal fractures<ref name=":8" />. | |||
* Less than 10% present as open fractures. | |||
* Earlier, calcaneum fracture was predominately in male as they used to do more industrial work. But recent studies suggest regional variation in male and female predominance.<ref name=":2" /> | |||
* 75% of the calcaneus fracture is intra-articular and the prognosis of intra-articular fracture is poor<ref name=":8" />. | |||
* Calcaneal fractures are rare in children.<ref name=":2" />In those 8-14 years-old, 60% of calcaneal fractures are extra-articular. This number increased to 90% for those under 7 years-old<ref name=":8" />. | |||
* 20-25% of the cases with a calcaneal fracture is associated with [[Lumbar Compression Fracture|compression fractures of the lumbar vertebrae.]] <ref>Bohl DD, Ondeck NT, Samuel AM, Diaz-Collado PJ, Nelson SJ, Basques BA, Leslie MP, Grauer JN. [https://journals.sagepub.com/doi/abs/10.1177/1938640016679703 Demographics, mechanisms of injury, and concurrent injuries associated with calcaneus fractures: a study of 14 516 patients in the American College of Surgeons National Trauma Data Bank.] Foot & ankle specialist. 2017 Oct;10(5):402-10.</ref> | |||
* Most patients with calcaneus fractures are young, with the 20-39 age group the most common. | |||
* Risk factors for calcaneal fractures include: [[osteoporosis]], [[Diabetes|diabetes mellitus]], [[Neuropathies|peripheral neuropathy]], [[osteomalacia]], and [[Immunotherapy|long-term immunosuppressive therapy]]<ref name=":8" />. | |||
== Mechanism of Injury / Pathological Process == | |||
* Calcaneal fractures are mostly the result of high energy events leading to axial loading of the bone<ref name=":8" />. | |||
Mostly, | * Predominantly, falls from height and automobile accidents (a foot depressed against an accelerator, brake, or floorboard) are common mechanisms of injury. The talus acting as a wedge causes depression and thus flatten, widen, and shorten the calcaneal body. | ||
* Calcaneal fractures can also occur with less severe accidents like an ankle sprain or a stress fracture in runners. | |||
* Jumping onto hard surfaces, blunt or penetrating trauma and twisting/shearing events may also cause calcaneus fracture.<ref name=":2" /> | |||
* Mostly, injuries occur in isolation. Most seen concomitant injuries were lower limb (13.2%) or spinal injuries (6.3%).<ref name=":0">Dhillon MS. Fractures of the calcaneus. JP Medical Ltd; 2013 Apr 30.</ref> | |||
* The posterior tibial neurovascular bundle runs along the medial aspect of the calcaneal body and is shielded by the sustentaculum tali thus ''neurovascular injuries are uncommon'' with calcaneal fractures.<ref name=":2" /> | |||
{{#ev:youtube|7LKOcB-wNrM}}<ref>Fractures Of The Calcaneus - Everything You Need To Know - Dr. Nabil Ebraheim. Available from:https://www.youtube.com/watch?v=7LKOcB-wNrM [last accessed 6/24/2020]</ref> | |||
== Characteristics / Clinical Presentation == | == Characteristics / Clinical Presentation == | ||
Initially, a patient may present with an above mentioned traumatic event with the following clinical features: | |||
* Patients will present with diffuse pain, edema, and ecchymosis at the affected fracture site. | |||
* The patient is not likely able to bear weight, walk, and move the foot. | |||
* Swelling in the heel area | |||
* Plantar ecchymosis extending through the plantar arch of the foot should raise suspicion significantly. | |||
* There may be associated disability of the Achilles tendon. | |||
* Skin quality around the heel must be evaluated for tenting and/or threatened skin. This is especially important in the setting of Tongue-type calcaneus fractures.<ref name=":2" /> | |||
*Generalized pain in the heel area that usually develops slowly (over several days to weeks) - most common with stress fractures | |||
*Deformity of the heel or plantar arch: Secondary to the displacement of the lateral calcaneal border outward, there is a possible widening or broadening of the heel.<ref name=":0" /> | |||
* | == Examination == | ||
* Palpation: Tenderness over calcaneus while squeezing the heel from both sides.<ref>Green, D. P. (2010). Rockwood and Green's fractures in adults (Vol. 1). C. A. Rockwood, R. W. Bucholz, J. D. Heckman, & P. Tornetta (Eds.). Lippincott Williams & Wilkins.</ref> A squeeze test is positive in stress fracture of the calcaneus. | |||
* A thorough neurovascular examination is important. Pulse rate of ipsilateral [[Dorsalis Pedis Artery|dorsalis pedis]] or posterior tibial can be compared to the contralateral limb. If there is any suspicion of arterial injury, further investigation with angiography or Doppler scanning can be done. | |||
* Evaluation of all lower extremity tendon function is also necessary. | |||
* Examination of spine fracture as an associated fracture of calcaneus from axial loading.<ref name=":2" /> | |||
* | |||
* | |||
* | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Radiological examination: | |||
[[File:Calcaneus-fracture-1.png|thumb|X-ray of left calcaneus fracture]] | |||
'''X-ray:''' AP, lateral, and oblique plain films of the foot and ankle are needed. A harris view may be obtained which demonstrates the calcaneus in an axial orientation. | |||
* Axial - Determines primary fracture line and displays the body, tuberosity, middle and posterior facets. | |||
* Lateral - Determines Bohler angle. | |||
* Oblique/Broden’s view - Displays the degree of displacement of the primary fracture line. <ref name=":6" /> | |||
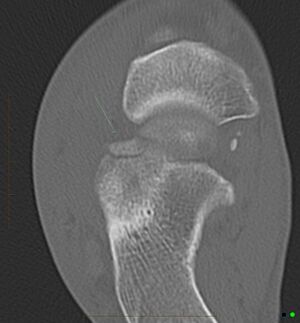
[[File:Anterior-process-of-calcaneus-fracture.jpg|thumb|CT scan of anterior process of calcaneus fracture with soft tissue swelling]] | |||
'''CT scan:''' It is gold standard for traumatic calcaneal injuries. | |||
'''Bone scan or MRI:''' are recommended in stress fracture of the calcaneus. | |||
Some of the reference angle and sign in the radiographic images are: | |||
* ''Mondor's Sign'' is a hematoma identified on CT that extends along the sole and is considered pathognomic for calcaneal fracture. | |||
* ''Bohler's Angle'' is defined as the angle between two lines drawn on plain film. The first line is between the highest point on the tuberosity and the highest point of posterior facet and the second is the highest point on the anterior process and the highest point on the posterior facet. The normal angle is between 20-40 degrees. It may be depressed on plain radiographs if it's calcaneus fracture. | |||
* The ''Critical Angle of Gissane'' is defined as the angle between two lines drawn on plain film. The first along the anterior downward slope of the calcaneus and the second along the superior upward slope. A normal angle is 130-145 degrees. It may be an increase in calcaneus fracture.<ref name=":2" /> | |||
== | == Classification == | ||
Calcaneal fractures can be classified into two general categories. | |||
* '''Extraarticular fractures:''' Accounts for 25 % of calcaneal fractures<ref name=":8" />. These typically include avulsion injuries of either the calcaneal tuberosity from the Achilles tendon, the anterior process from the bifurcate ligament, the sustentaculum tali, calcaneal body fracture, stress fracture. | |||
{{#ev:youtube|0TB0HMkgNXs }}<ref>Calcaneal Fractures Extra-articular Fractures - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: https://www.youtube.com/watch?v=0TB0HMkgNXs [last accessed 6/24/2020]</ref> | |||
* '''Intraarticular Fractures:''' Accounts for 75% of calcaneal fractures<ref name=":8" />. Fractures involving any of the three subtalar articulating surfaces are known as intra-articular fractures and are common results of high force axial loading: a combination of shearing and compression forces produces both the primary and secondary fracture lines. The talus acts as a hammer or wedge compressing the calcaneus at the angle of Gissane causing the fracture. An intra-articular fracture can be further classified based on these two classification system mentioned below:<ref name=":6" /> | |||
{{#ev:youtube|kHtWVGSlZeA}}<ref>Calcaneal IntraArticular Fractures Essex Lopresti - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: https://www.youtube.com/watch?v=kHtWVGSlZeA[last accessed 6/24/2020]</ref> | |||
<u>Essex-Lopresti classification</u>: It is based on fracture lines using lateral radiographical images. | |||
* ''Joint depression type'' with a single vertical fracture line through the angle of Gissane separating the anterior and posterior portions of the calcaneus. | |||
* ''Tongue type'' which has the same vertical fracture line as a depression type with another horizontal fracture line running posteriorly, creating a superior posterior fragment. The tuberosity fragment may then rotate superiorly.<ref name=":2" /> | |||
<u>Sander Classification:</u> It is a widely used classification system which uses coronal reconstructed CT images showing posterior facet. The Sanders classification system is useful not only in treatment planning but in helping to determine prognosis.<ref name=":1" /> there are 4 types of fracture based on the number and location of the articular fragments. | |||
* Type I fractures are nondisplaced. | |||
* Type II fractures (two articular pieces) involve the posterior facet and are subdivided into types A, B, and C, depending on the medial or lateral location of the fracture line (more medial fractures are harder to visualize and reduce intraoperatively). | |||
* Type III fractures (three articular pieces) include an additional depressed middle fragment and are subdivided into types AB, AC, and BC, depending on the position and location of the fracture lines. | |||
* Type IV fractures (four or more articular fragments) are highly comminuted.<ref name=":2" /><ref name=":1" /> | |||
{{#ev:youtube|2eOo2QxdTbs}}<ref>Calcaneal Intra-Articular Fractures, Sanders - Everything You Need To Know - Dr. Nabil Ebraheim. Available from:https://www.youtube.com/watch?v=2eOo2QxdTbs [last accessed 6/24/2020]</ref> | |||
== Management/Intervention == | |||
There is no universal treatment or surgical approach to all calcaneal fractures. Treatment of calcaneal fractures depends on the individual fracture pathoanatomy, accompanying soft-tissue damage, associated injuries, functional demand, and comorbidities of the patient.<ref name=":7">Rammelt S, Sangeorzan BJ, Swords MP. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5961258/ Calcaneal fractures—should we or should we not operate?.] Indian Journal of Orthopaedics. 2018 Jun;52:220-30.</ref> | |||
The treatment of calcaneus fracture can be divided into operative and non-operative treatment. | |||
===Non-Operative Care=== | |||
Nonoperative management is preferable when there is no impingement of the peroneal tendons and the fracture segments are not displaced (or are displaced less than 2 mm).<ref name=":7" /> Nonoperative care is also recommended when, despite the presence of a fracture, proper weight-bearing alignment has been adequately maintained and articulating surfaces are not disturbed. Extra-articular fractures are generally treated conservatively. Patients who are over the age of 65 years old or who have pre-existing health conditions, such as diabetes, neurovascular insufficiency, noncompliance (e.g., substance abuse), and severe systemic disorders with immunodeficiency and/or poor overall prognosis are also commonly treated using nonoperative techniques.<ref name=":7" /> | |||
[[RICE]] protocol for soft tissue injury can be followed with immobilization in non- operative management. | |||
= | Immobilization: A cast, splint, or brace will hold the bones in your foot in proper position while they heal. A cast needs to wear for 6 to 8 weeks — or possibly longer based on follow up radiographic images. During this time, weight-bearing is strictly prohibited.<ref name=":4">Fischer, J.S.,MD; A. J. . Lowe, MD. (2016) Calcaneus (heel bone) fractures. Geraadpleegd op 5 december 2016. </ref> | ||
=== Operative Care === | |||
For the majority of patients with the calcaneus fracture, surgery is the indicated treatment<ref name=":3">Takasaka M, Bittar CK, Mennucci FS, de Mattos CA, Zabeu JL. Comparative study on three surgical techniques for intra-articular calcaneal fractures: open reduction with internal fixation using a plate, external fixation and minimally invasive surgery. Revista Brasileira de Ortopedia (English Edition). 2016 May 1;51(3):254-60.</ref>. Intraarticular fractures are often treated operatively. The goal of surgery is to reconstruct the overall shape of the calcaneum and joint surfaces to obtain a good functional result.<ref name=":7" /> This is possible by performing an open reduction and internal fixation of the fracture. There are various approaches for performing open reduction and internal fixation. This procedure decreases the possibility of developing arthritis ( post-traumatic [[Subtalar Joint Arthritis|subtalar arthritis]]) and maximizes the potential for inversion and eversion of the foot.<ref name=":7" /> | |||
Extraarticular fractures with a substantial hindfoot varus or valgus deformity (>10°) and those with significant flattening, broadening, or shortening of the heel should also be reduced, preferably via small or percutaneous approaches. A dangerous extraarticular subtype of a tongue-type fracture with severe displacement of the superior margin of the calcaneal tuberosity (“beak fracture”) is a surgical emergency.<ref name=":7" /> | |||
== Physical Therapy Management == | |||
There are many similarities between nonoperative and operative physical therapy management of calcaneal fractures. These similarities include: periods of immobilization with restricted weightbearing, joint mobilization, range of motion exercises, pain management, strengthening, proprioception training, gait training, plyometrics, and gradual loading to resume more challenging activities. | |||
These are some outcome measures that can be used to measure the functional abilities of the patient to see the prognosis which can be used during the rehabilitation period: | |||
* [[Lower Extremity Functional Scale (LEFS)]] | |||
* [[Foot and Ankle Ability Measure|Foot and Ankle Ability Measure (FAAM)]] | |||
=== Pre-Surgery === | |||
Initial stability is essential for open reduction internal fixation of intraarticular calcaneal fractures. | |||
Preoperative revalidation consist of:<br>• Immediate elevation of the affected foot to reduce swelling.<br>• Compression such as foot pump, intermittent compression devices, or compression wraps as tolerable.<br>• Instructions for using wheelchair, bed transfers, or [[Crutches|crutch walking]].<ref name=":5">Griffin D, Parsons N, Shaw E, Kulikov Y, Hutchinson C, Thorogood M, Lamb SE. Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. Bmj. 2014 Jul 24;349:g4483.</ref><ref>Lance EM, CAREY EJ, WADE PA. 9 Fractures of the Os Calcis: Treatment by Early Mobilization. Clinical Orthopaedics and Related Research (1976-2007). 1963 Jan 1;30:76-90.</ref><br> | |||
== | === Post-Surgery === | ||
Both the progression of nonoperative and postoperative management of calcaneal fractures include traditional immobilization and early motion rehabilitation protocols. In fact, the traditional immobilization protocols of nonoperative and postoperative management are similar, and are thereby combined in the progression below. <ref name=":6">Joe Hodges PT, Robert Klingman,"Calcaneal Fracture and Rehabilitation". </ref> Phases II and III of traditional and early motion rehabilitation protocols after nonoperative or postoperative care are comparable as well and are described together below. <ref name=":0" /><ref>Hu QD, Jiao PY, Shao CS, Zhang WG, Zhang K, Li Q. Manipulative reduction and external fixation with cardboard for the treatment of distal radial fracture. Zhongguo gu shang= China journal of orthopaedics and traumatology. 2011 Nov;24(11):907-9.</ref> | |||
==== Phase I: Weeks 1-4 ==== | |||
==== | ===== Goals: ===== | ||
* Control edema and pain | |||
* Prevent extension of fracture or loss of surgical stabilization | |||
* Minimize loss of function and cardiovascular endurance | |||
===== Intervention: ===== | |||
* Cast with the ankle in neutral and sometimes slight eversion | |||
* Elevation | |||
* Toe curl and active ankle joint (dorsiflexion and plantarflexion)-encourage to do from the first post-operative day.<ref>Zhang G, Ding S, Ruan Z. [https://journals.sagepub.com/doi/full/10.1177/0300060519853402 Minimally invasive treatment of calcaneal fracture.] Journal of International Medical Research. 2019 Aug;47(8):3946-54.</ref> | |||
* After 2-4 days, instruct in non-[[weight bearing]] ambulation utilizing crutches or walker-[[Crutches|crutch walking training]] | |||
* Instruct in wheelchair use with an appropriate sitting schedule to limit time involved extremity spends in dependent-gravity position | |||
* Instruct in comprehensive exercise and cardiovascular program utilizing upper extremities and uninvolved lower extremity | |||
* Strengthening adjacent joint musculature (hip and knee)<br> | |||
==== | ==== Phase II: Weeks 5-8 ==== | ||
===== Goals: ===== | |||
* Control remaining or residual edema and pain | |||
* Prevent re-injury or complication of fracture by progressing weight-bearing safely | |||
* Prevent contracture and regain motion at ankle/foot joints | |||
* Minimize loss of function and cardiovascular endurance | |||
===== Intervention: ===== | |||
* Continued elevation, icing, and compression as needed for involved lower extremity. | |||
* After 6-8 weeks, instruct in partial-weight bearing ambulation utilizing crutches or walker | |||
* Initiate vigorous exercise and range of motion to regain and maintain motion at all joints: tibiotalar, subtalar, midtarsal, and toe joints, including active range of motion in large amounts of movement and progressive isometric or resisted exercises | |||
* Progress and monitor comprehensive upper extremity and cardiovascular program | |||
==== | ==== Phase III: Weeks 9-12 ==== | ||
===== Goals: ===== | |||
* Progress weight-bearing status | |||
* Normal gait on all surfaces | |||
* Restore full range of motion | |||
* Restore full strength | |||
* Allow return to previous work status | |||
===== Intervention: ===== | |||
* After 9-12 weeks, instruct in normal full-weight bearing ambulation with the appropriate assistive device as needed | |||
* Progress and monitor the subtalar joint’s ability to adapt for ambulation on all surfaces, including graded and uneven surfaces | |||
* Joint mobilization to all hypomobile joints including: tibiotalar, subtalar, midtarsal, and to toe joints | |||
* Soft tissue mobilization to hypomobile tissues of the gastrocnemius complex, plantar fascia, or other appropriate tissues | |||
* Progressive resisted strengthening of gastrocnemius complex through the use of pulleys, weighted exercise, toe-walking ambulation, ascending/descending stairs, skipping or other plyometric exercise, pool exercises, and other climbing activities | |||
* Work hardening program or activities to allow return to work between 13- 52 weeks. | |||
==== '''Implant Removal:''' ==== | |||
Implant removal 1 year after plate fixation is only advocated in cases of protruding hardware or massive arthrofibrosis with limited range of motion, mostly after plate fixation through extensile approaches. Implant removal is combined with intraarticular arthrolysis and debridement employing subtalar arthroscopy.<ref name=":7" /> | |||
== Resources == | == Resources == | ||
| Line 182: | Line 177: | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Calcaneal fractures can be divided | Calcaneal fractures can be divided into two groups: intra-articular and extra-articular calcaneal fractures. Intra-articular fractures have a lower prognosis. To determine the kind of fracture and if there is a fracture, medical imaging is needed. The rehabilitation program consists of 3 stages postoperatively and is very important to enhance recovery. <div class="coursebox"> | ||
{| class="FCK__ShowTableBorders" width="100%" cellspacing="4" cellpadding="4" border="0" | |||
<div class="coursebox"> | |||
{| width="100%" cellspacing="4" cellpadding="4" border="0 | |||
|- | |- | ||
| align="center" | | | align="center" | | ||
| | | | ||
|} | |} | ||
</div> | </div> | ||
== References == | == References == | ||
| Line 204: | Line 191: | ||
<br><br> | <br><br> | ||
[[Category:Foot]][[Category: | [[Category:Foot]] | ||
[[Category:Foot - Conditions]] | |||
[[Category:Conditions]] | |||
[[Category:Fractures]] | |||
Latest revision as of 16:50, 11 April 2022
Definition / Description[edit | edit source]
A calcaneus fracture is a heel bone fracture. It is a rare type of fracture but has potentially debilitating results. Traditionally, a burst fracture of the calcaneus was known as "Lovers Fracture" as the injury would occur as a suitor would jump off a lover's balcony (axial loading) to avoid detection.[1]
Clinically Relevant Anatomy[edit | edit source]
A good understanding of the anatomy of the calcaneus is essential in determining the patterns of injury and treatment goals and options.
Calcaneus is the largest talar bone out of 7 tarsal bones which together with the talus form hind-foot. The calcaneus has a relatively thin cortex. It has 4 facets: 1 anteriorly which articulate with cuboid forming calcaneocuboid joint and 3 superiorly (anterior, middle, and posterior, with the posterior facet representing the major weight-bearing surface) which articulate with talus forming talocalcaneal joint (subtalar joint). Subtalar joint allows inversion and eversion of the foot.[2][1]
The interosseous ligament and medial, lateral, and posterior talocalcaneal ligaments provide additional support for the joint. The sustentaculum tali is a medial bony projection supporting the neck of the talus. The tibial artery, nerve, posterior tibial tendon, and flexor hallucis longus tendon are located medially to the calcaneus and are at risk for impingement with a calcaneal fracture and, as are the peroneal tendons located on the lateral aspect of the calcaneus. This also makes surgical approach challenging. The lateral side of the calcaneus and its flat nature is highlighted as the most advantageous for internal fixation, but the poor soft tissue cover challenges wound healing.[3]These anatomic landmarks are important because fractures associated with these areas may cause involve joint involvement, tendon and neurovascular injury.[3]
The calcaneus has four important functions:
- Acts as a foundation and support for the body’s weight
- Supports the lateral column of the foot and acts as the main articulation for inversion/eversion
- Acts as a lever arm for the gastrocnemius muscle complex
- Makes normal walking possible
Epidemiology/Etiology[edit | edit source]
- Calcaneal fractures account for 1-2% of all fractures[4] and 60% of tarsal fractures[4].
- Less than 10% present as open fractures.
- Earlier, calcaneum fracture was predominately in male as they used to do more industrial work. But recent studies suggest regional variation in male and female predominance.[1]
- 75% of the calcaneus fracture is intra-articular and the prognosis of intra-articular fracture is poor[4].
- Calcaneal fractures are rare in children.[1]In those 8-14 years-old, 60% of calcaneal fractures are extra-articular. This number increased to 90% for those under 7 years-old[4].
- 20-25% of the cases with a calcaneal fracture is associated with compression fractures of the lumbar vertebrae. [5]
- Most patients with calcaneus fractures are young, with the 20-39 age group the most common.
- Risk factors for calcaneal fractures include: osteoporosis, diabetes mellitus, peripheral neuropathy, osteomalacia, and long-term immunosuppressive therapy[4].
Mechanism of Injury / Pathological Process[edit | edit source]
- Calcaneal fractures are mostly the result of high energy events leading to axial loading of the bone[4].
- Predominantly, falls from height and automobile accidents (a foot depressed against an accelerator, brake, or floorboard) are common mechanisms of injury. The talus acting as a wedge causes depression and thus flatten, widen, and shorten the calcaneal body.
- Calcaneal fractures can also occur with less severe accidents like an ankle sprain or a stress fracture in runners.
- Jumping onto hard surfaces, blunt or penetrating trauma and twisting/shearing events may also cause calcaneus fracture.[1]
- Mostly, injuries occur in isolation. Most seen concomitant injuries were lower limb (13.2%) or spinal injuries (6.3%).[6]
- The posterior tibial neurovascular bundle runs along the medial aspect of the calcaneal body and is shielded by the sustentaculum tali thus neurovascular injuries are uncommon with calcaneal fractures.[1]
Characteristics / Clinical Presentation[edit | edit source]
Initially, a patient may present with an above mentioned traumatic event with the following clinical features:
- Patients will present with diffuse pain, edema, and ecchymosis at the affected fracture site.
- The patient is not likely able to bear weight, walk, and move the foot.
- Swelling in the heel area
- Plantar ecchymosis extending through the plantar arch of the foot should raise suspicion significantly.
- There may be associated disability of the Achilles tendon.
- Skin quality around the heel must be evaluated for tenting and/or threatened skin. This is especially important in the setting of Tongue-type calcaneus fractures.[1]
- Generalized pain in the heel area that usually develops slowly (over several days to weeks) - most common with stress fractures
- Deformity of the heel or plantar arch: Secondary to the displacement of the lateral calcaneal border outward, there is a possible widening or broadening of the heel.[6]
Examination[edit | edit source]
- Palpation: Tenderness over calcaneus while squeezing the heel from both sides.[8] A squeeze test is positive in stress fracture of the calcaneus.
- A thorough neurovascular examination is important. Pulse rate of ipsilateral dorsalis pedis or posterior tibial can be compared to the contralateral limb. If there is any suspicion of arterial injury, further investigation with angiography or Doppler scanning can be done.
- Evaluation of all lower extremity tendon function is also necessary.
- Examination of spine fracture as an associated fracture of calcaneus from axial loading.[1]
Diagnostic Procedures[edit | edit source]
Radiological examination:
X-ray: AP, lateral, and oblique plain films of the foot and ankle are needed. A harris view may be obtained which demonstrates the calcaneus in an axial orientation.
- Axial - Determines primary fracture line and displays the body, tuberosity, middle and posterior facets.
- Lateral - Determines Bohler angle.
- Oblique/Broden’s view - Displays the degree of displacement of the primary fracture line. [2]
CT scan: It is gold standard for traumatic calcaneal injuries.
Bone scan or MRI: are recommended in stress fracture of the calcaneus.
Some of the reference angle and sign in the radiographic images are:
- Mondor's Sign is a hematoma identified on CT that extends along the sole and is considered pathognomic for calcaneal fracture.
- Bohler's Angle is defined as the angle between two lines drawn on plain film. The first line is between the highest point on the tuberosity and the highest point of posterior facet and the second is the highest point on the anterior process and the highest point on the posterior facet. The normal angle is between 20-40 degrees. It may be depressed on plain radiographs if it's calcaneus fracture.
- The Critical Angle of Gissane is defined as the angle between two lines drawn on plain film. The first along the anterior downward slope of the calcaneus and the second along the superior upward slope. A normal angle is 130-145 degrees. It may be an increase in calcaneus fracture.[1]
Classification[edit | edit source]
Calcaneal fractures can be classified into two general categories.
- Extraarticular fractures: Accounts for 25 % of calcaneal fractures[4]. These typically include avulsion injuries of either the calcaneal tuberosity from the Achilles tendon, the anterior process from the bifurcate ligament, the sustentaculum tali, calcaneal body fracture, stress fracture.
- Intraarticular Fractures: Accounts for 75% of calcaneal fractures[4]. Fractures involving any of the three subtalar articulating surfaces are known as intra-articular fractures and are common results of high force axial loading: a combination of shearing and compression forces produces both the primary and secondary fracture lines. The talus acts as a hammer or wedge compressing the calcaneus at the angle of Gissane causing the fracture. An intra-articular fracture can be further classified based on these two classification system mentioned below:[2]
Essex-Lopresti classification: It is based on fracture lines using lateral radiographical images.
- Joint depression type with a single vertical fracture line through the angle of Gissane separating the anterior and posterior portions of the calcaneus.
- Tongue type which has the same vertical fracture line as a depression type with another horizontal fracture line running posteriorly, creating a superior posterior fragment. The tuberosity fragment may then rotate superiorly.[1]
Sander Classification: It is a widely used classification system which uses coronal reconstructed CT images showing posterior facet. The Sanders classification system is useful not only in treatment planning but in helping to determine prognosis.[3] there are 4 types of fracture based on the number and location of the articular fragments.
- Type I fractures are nondisplaced.
- Type II fractures (two articular pieces) involve the posterior facet and are subdivided into types A, B, and C, depending on the medial or lateral location of the fracture line (more medial fractures are harder to visualize and reduce intraoperatively).
- Type III fractures (three articular pieces) include an additional depressed middle fragment and are subdivided into types AB, AC, and BC, depending on the position and location of the fracture lines.
- Type IV fractures (four or more articular fragments) are highly comminuted.[1][3]
Management/Intervention[edit | edit source]
There is no universal treatment or surgical approach to all calcaneal fractures. Treatment of calcaneal fractures depends on the individual fracture pathoanatomy, accompanying soft-tissue damage, associated injuries, functional demand, and comorbidities of the patient.[12]
The treatment of calcaneus fracture can be divided into operative and non-operative treatment.
Non-Operative Care[edit | edit source]
Nonoperative management is preferable when there is no impingement of the peroneal tendons and the fracture segments are not displaced (or are displaced less than 2 mm).[12] Nonoperative care is also recommended when, despite the presence of a fracture, proper weight-bearing alignment has been adequately maintained and articulating surfaces are not disturbed. Extra-articular fractures are generally treated conservatively. Patients who are over the age of 65 years old or who have pre-existing health conditions, such as diabetes, neurovascular insufficiency, noncompliance (e.g., substance abuse), and severe systemic disorders with immunodeficiency and/or poor overall prognosis are also commonly treated using nonoperative techniques.[12]
RICE protocol for soft tissue injury can be followed with immobilization in non- operative management.
Immobilization: A cast, splint, or brace will hold the bones in your foot in proper position while they heal. A cast needs to wear for 6 to 8 weeks — or possibly longer based on follow up radiographic images. During this time, weight-bearing is strictly prohibited.[13]
Operative Care[edit | edit source]
For the majority of patients with the calcaneus fracture, surgery is the indicated treatment[14]. Intraarticular fractures are often treated operatively. The goal of surgery is to reconstruct the overall shape of the calcaneum and joint surfaces to obtain a good functional result.[12] This is possible by performing an open reduction and internal fixation of the fracture. There are various approaches for performing open reduction and internal fixation. This procedure decreases the possibility of developing arthritis ( post-traumatic subtalar arthritis) and maximizes the potential for inversion and eversion of the foot.[12]
Extraarticular fractures with a substantial hindfoot varus or valgus deformity (>10°) and those with significant flattening, broadening, or shortening of the heel should also be reduced, preferably via small or percutaneous approaches. A dangerous extraarticular subtype of a tongue-type fracture with severe displacement of the superior margin of the calcaneal tuberosity (“beak fracture”) is a surgical emergency.[12]
Physical Therapy Management[edit | edit source]
There are many similarities between nonoperative and operative physical therapy management of calcaneal fractures. These similarities include: periods of immobilization with restricted weightbearing, joint mobilization, range of motion exercises, pain management, strengthening, proprioception training, gait training, plyometrics, and gradual loading to resume more challenging activities.
These are some outcome measures that can be used to measure the functional abilities of the patient to see the prognosis which can be used during the rehabilitation period:
Pre-Surgery[edit | edit source]
Initial stability is essential for open reduction internal fixation of intraarticular calcaneal fractures.
Preoperative revalidation consist of:
• Immediate elevation of the affected foot to reduce swelling.
• Compression such as foot pump, intermittent compression devices, or compression wraps as tolerable.
• Instructions for using wheelchair, bed transfers, or crutch walking.[15][16]
Post-Surgery[edit | edit source]
Both the progression of nonoperative and postoperative management of calcaneal fractures include traditional immobilization and early motion rehabilitation protocols. In fact, the traditional immobilization protocols of nonoperative and postoperative management are similar, and are thereby combined in the progression below. [2] Phases II and III of traditional and early motion rehabilitation protocols after nonoperative or postoperative care are comparable as well and are described together below. [6][17]
Phase I: Weeks 1-4[edit | edit source]
Goals:[edit | edit source]
- Control edema and pain
- Prevent extension of fracture or loss of surgical stabilization
- Minimize loss of function and cardiovascular endurance
Intervention:[edit | edit source]
- Cast with the ankle in neutral and sometimes slight eversion
- Elevation
- Toe curl and active ankle joint (dorsiflexion and plantarflexion)-encourage to do from the first post-operative day.[18]
- After 2-4 days, instruct in non-weight bearing ambulation utilizing crutches or walker-crutch walking training
- Instruct in wheelchair use with an appropriate sitting schedule to limit time involved extremity spends in dependent-gravity position
- Instruct in comprehensive exercise and cardiovascular program utilizing upper extremities and uninvolved lower extremity
- Strengthening adjacent joint musculature (hip and knee)
Phase II: Weeks 5-8[edit | edit source]
Goals:[edit | edit source]
- Control remaining or residual edema and pain
- Prevent re-injury or complication of fracture by progressing weight-bearing safely
- Prevent contracture and regain motion at ankle/foot joints
- Minimize loss of function and cardiovascular endurance
Intervention:[edit | edit source]
- Continued elevation, icing, and compression as needed for involved lower extremity.
- After 6-8 weeks, instruct in partial-weight bearing ambulation utilizing crutches or walker
- Initiate vigorous exercise and range of motion to regain and maintain motion at all joints: tibiotalar, subtalar, midtarsal, and toe joints, including active range of motion in large amounts of movement and progressive isometric or resisted exercises
- Progress and monitor comprehensive upper extremity and cardiovascular program
Phase III: Weeks 9-12[edit | edit source]
Goals:[edit | edit source]
- Progress weight-bearing status
- Normal gait on all surfaces
- Restore full range of motion
- Restore full strength
- Allow return to previous work status
Intervention:[edit | edit source]
- After 9-12 weeks, instruct in normal full-weight bearing ambulation with the appropriate assistive device as needed
- Progress and monitor the subtalar joint’s ability to adapt for ambulation on all surfaces, including graded and uneven surfaces
- Joint mobilization to all hypomobile joints including: tibiotalar, subtalar, midtarsal, and to toe joints
- Soft tissue mobilization to hypomobile tissues of the gastrocnemius complex, plantar fascia, or other appropriate tissues
- Progressive resisted strengthening of gastrocnemius complex through the use of pulleys, weighted exercise, toe-walking ambulation, ascending/descending stairs, skipping or other plyometric exercise, pool exercises, and other climbing activities
- Work hardening program or activities to allow return to work between 13- 52 weeks.
Implant Removal:[edit | edit source]
Implant removal 1 year after plate fixation is only advocated in cases of protruding hardware or massive arthrofibrosis with limited range of motion, mostly after plate fixation through extensile approaches. Implant removal is combined with intraarticular arthrolysis and debridement employing subtalar arthroscopy.[12]
Resources[edit | edit source]
http://ezinearticles.com/?Rehabilitation-After-Calcaneal-Fractures&id=4082480
http://orthopedics.about.com/od/footanklefractures/a/calcaneus.htm
http://xnet.kp.org/socal_rehabspecialists/ptr_library/09FootRegion/31Foot-CalcanealFracture.pdf
http://www.healthstatus.com/articles/Calcaneal_Fractures.html
Clinical Bottom Line[edit | edit source]
Calcaneal fractures can be divided into two groups: intra-articular and extra-articular calcaneal fractures. Intra-articular fractures have a lower prognosis. To determine the kind of fracture and if there is a fracture, medical imaging is needed. The rehabilitation program consists of 3 stages postoperatively and is very important to enhance recovery.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Davis D, Newton EJ. Calcaneus Fractures.
- ↑ 2.0 2.1 2.2 2.3 Joe Hodges PT, Robert Klingman,"Calcaneal Fracture and Rehabilitation".
- ↑ 3.0 3.1 3.2 3.3 Daftary A, Haims AH, Baumgaertner MR. Fractures of the calcaneus: a review with emphasis on CT. Radiographics. 2005 Sep;25(5):1215-26.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Galluzzo M, Greco F, Pietragalla M, De Renzis A, Carbone M, Zappia M, Maggialetti N, D'andrea A, Caracchini G, Miele V. Calcaneal fractures: radiological and CT evaluation and classification systems. Acta Biomed. 2018 Jan 19;89(1-S):138-150.
- ↑ Bohl DD, Ondeck NT, Samuel AM, Diaz-Collado PJ, Nelson SJ, Basques BA, Leslie MP, Grauer JN. Demographics, mechanisms of injury, and concurrent injuries associated with calcaneus fractures: a study of 14 516 patients in the American College of Surgeons National Trauma Data Bank. Foot & ankle specialist. 2017 Oct;10(5):402-10.
- ↑ 6.0 6.1 6.2 Dhillon MS. Fractures of the calcaneus. JP Medical Ltd; 2013 Apr 30.
- ↑ Fractures Of The Calcaneus - Everything You Need To Know - Dr. Nabil Ebraheim. Available from:https://www.youtube.com/watch?v=7LKOcB-wNrM [last accessed 6/24/2020]
- ↑ Green, D. P. (2010). Rockwood and Green's fractures in adults (Vol. 1). C. A. Rockwood, R. W. Bucholz, J. D. Heckman, & P. Tornetta (Eds.). Lippincott Williams & Wilkins.
- ↑ Calcaneal Fractures Extra-articular Fractures - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: https://www.youtube.com/watch?v=0TB0HMkgNXs [last accessed 6/24/2020]
- ↑ Calcaneal IntraArticular Fractures Essex Lopresti - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: https://www.youtube.com/watch?v=kHtWVGSlZeA[last accessed 6/24/2020]
- ↑ Calcaneal Intra-Articular Fractures, Sanders - Everything You Need To Know - Dr. Nabil Ebraheim. Available from:https://www.youtube.com/watch?v=2eOo2QxdTbs [last accessed 6/24/2020]
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 Rammelt S, Sangeorzan BJ, Swords MP. Calcaneal fractures—should we or should we not operate?. Indian Journal of Orthopaedics. 2018 Jun;52:220-30.
- ↑ Fischer, J.S.,MD; A. J. . Lowe, MD. (2016) Calcaneus (heel bone) fractures. Geraadpleegd op 5 december 2016.
- ↑ Takasaka M, Bittar CK, Mennucci FS, de Mattos CA, Zabeu JL. Comparative study on three surgical techniques for intra-articular calcaneal fractures: open reduction with internal fixation using a plate, external fixation and minimally invasive surgery. Revista Brasileira de Ortopedia (English Edition). 2016 May 1;51(3):254-60.
- ↑ Griffin D, Parsons N, Shaw E, Kulikov Y, Hutchinson C, Thorogood M, Lamb SE. Operative versus non-operative treatment for closed, displaced, intra-articular fractures of the calcaneus: randomised controlled trial. Bmj. 2014 Jul 24;349:g4483.
- ↑ Lance EM, CAREY EJ, WADE PA. 9 Fractures of the Os Calcis: Treatment by Early Mobilization. Clinical Orthopaedics and Related Research (1976-2007). 1963 Jan 1;30:76-90.
- ↑ Hu QD, Jiao PY, Shao CS, Zhang WG, Zhang K, Li Q. Manipulative reduction and external fixation with cardboard for the treatment of distal radial fracture. Zhongguo gu shang= China journal of orthopaedics and traumatology. 2011 Nov;24(11):907-9.
- ↑ Zhang G, Ding S, Ruan Z. Minimally invasive treatment of calcaneal fracture. Journal of International Medical Research. 2019 Aug;47(8):3946-54.