Bronchiolitis: Difference between revisions
No edit summary |
Candace Goh (talk | contribs) (updated evidence) |
||
| (4 intermediate revisions by 3 users not shown) | |||
| Line 6: | Line 6: | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
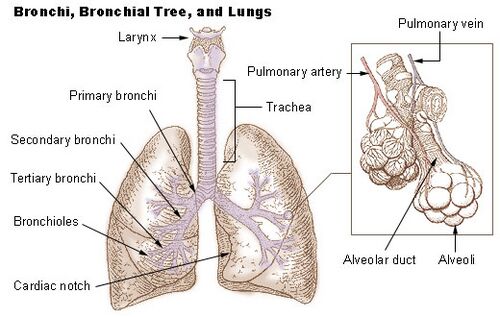
The bronchioles do not have cartilage<ref name=":1">Leslie KO, Wick MR. Bronchiole [Internet]. Bronchiole - an overview | ScienceDirect Topics. [cited 2023Jan14]. Available from: https://www.sciencedirect.com/topics/immunology-and-microbiology/bronchiole</ref> where the bronchi have a firbrocartilaginous framework<ref name=":2">Lust RM. Bronchiole [Internet]. Bronchiole - an overview | ScienceDirect Topics. [cited 2023Jan14]. Available from: https://www.sciencedirect.com/topics/immunology-and-microbiology/bronchiole</ref>. They are the final air conductors and do not have alveoli.<ref name=":1" />There are about 30000 terminal bronchioles, each of which directs air to about 10000 alveoli.<ref name=":1" /> Bronchioles have a continuous circular layer of smooth muscle and the bronchi mucosa is continuous with the mucosa of the bronchioles.<ref name=":2" /> The mucociliary blanket of the bronchioles is a watery fluid that accumulates muscous as it ascends the airway.<ref name=":2" />[[Image:Lung anatomy.jpg|thumb|500x500px|alt=]] | |||
== Epidemiology == | == Epidemiology == | ||
Bronchiolitis | In the first year of life, bronchiolitis is the most common lower respiratory tract infection.<ref name=":3">Ricci V, Nunes VD, Murphy MS, Cunningham S. [http://dickyricky.com/Medicine/Papers/2015_06_06%20BMJ%20Bronchiolitis%20in%20children%20summary%20of%20NICE%20guideline.pdf Bronchiolitis in children: summary of NICE guidance.] Bmj. 2015 Jun 2;350.</ref><ref name=":8">O'Brien S, Borland ML, Cotterell E, Armstrong D, Babl F, Bauert P, Brabyn C, Garside L, Haskell L, Levitt D, McKay N. [http://medi-guide.meditool.cn/ymtpdf/43941565-9A53-1747-9C85-181A2E95DFF7.pdf Australasian bronchiolitis guideline. Journal of paediatrics and child health.] 2019 Jan;55(1):42-53.</ref>. It affects one in five infants and 2%-3% require admission to hospital.<ref name=":3" /> It also has a seasonal predilection, with more infections during the winter.<ref name=":0">Bronchiolitis. nhs.uk. [cited 13 April 2020]. Available from: https://www.nhs.uk/conditions/bronchiolitis/</ref><ref name=":4">Florin TA, Plint AC, Zorc JJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6765220/ Viral bronchiolitis]. The Lancet. 2017 Jan 14;389(10065):211-24.</ref> | ||
== Etiology == | == Etiology == | ||
Bronchiolitis is usually caused by the ''Respiratory Syncytial Virus (RSV)''. Other pathogens can also cause bronchiolitis such as human rhinovirus, influenza virus, coronavirus, human metapneumovirus (hMPV) and parainfluenza virus.<ref>Miller EK, Gebretsadik T, Carroll KN, et al. Viral etiologies of infant bronchiolitis, croup and upper respiratory illness during 4 consecutive years. ''Pediatr Infect Dis J''. 2013;32(9):950–955. doi:10.1097/INF.0b013e31829b7e43 Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3880140/</ref> | Bronchiolitis is usually caused by the ''Respiratory Syncytial Virus (RSV)''.<ref name=":5" /><ref name=":4" /> Other pathogens can also cause bronchiolitis such as human rhinovirus, influenza virus, coronavirus, human metapneumovirus (hMPV) and parainfluenza virus.<ref name=":5">Miller EK, Gebretsadik T, Carroll KN, et al. Viral etiologies of infant bronchiolitis, croup and upper respiratory illness during 4 consecutive years. ''Pediatr Infect Dis J''. 2013;32(9):950–955. doi:10.1097/INF.0b013e31829b7e43 Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3880140/</ref> | ||
== | == Pathogenesis due to RSV == | ||
Inoculation of the conjunctival or nasal mucosa by contaminated secretions or inhalation of large respiratory droplets that contain the virus leads to infection. There is an incubation period of 4 - 6 days and then viral replication in the nasal epithelium leads to symptoms. Once the virus has spread to the lower respiratory tract, the alveolar pneumocytes and the ciliated epithelial cells of the mucosa of the bronchioles become infected. Impaired ciliary beating and the sloughing of the infected epithelium causes intraluminal obstruction. The bronchiolar epithelium starts to regenerate within 3 to 4 days after symptom resolution.<ref name=":6">Meissner HC. [http://81.143.226.227/Medicine/Papers/2016_01_07%20NEJM%20Viral%20Bronchiolitis%20in%20Children.pdf Viral bronchiolitis in children.] New England Journal of Medicine. 2016 Jan 7;374(1):62-72.</ref> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
*Rhinorrhea (early presentation)<ref name=":4" /><ref name=":6" /> | |||
*Nasal congestion<ref name=":6" /> | |||
* | *Cough<ref name=":4" /><ref name=":6" /> | ||
* | *Tachypnoea<ref name=":4" /><ref name=":6" /> | ||
* | *Increased work of breathing<ref name=":4" /><ref name=":6" /> | ||
* | *Crackles and wheezing on auscultation<ref name=":4" /><ref name=":6" /><br> | ||
* | |||
== Diagnosis == | == Diagnosis == | ||
Diagnosis can be made through physical examination and history taking. | Diagnosis can be made through physical examination and history taking.<ref name=":6" /><ref name=":4" /> Clinical practice guidelines indicate that chest x-rays and laboratory studies should not be routine<ref name=":6" /><ref name=":4" />. Pulse oximetry has received increased attention in studies and clinical guidelines.<ref name=":4" /> Chest x-rays should only be done in severe cases, if complications are suspected, if the diagnosis un unclear and if the child does not respond to treatment.<ref name=":7" />Blood tests should only be done in severe cases.<ref name=":7" /> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* Pertussis<ref name=":4" /><ref name=":7">White DA, Zar HJ, Madhi SA, Jeena P, Morrow B, Masekela R, Risenga S, Green RJ. [http://www.scielo.org.za/pdf/samj/v106n4/12.pdf Acute viral bronchiolitis in South Africa: Diagnostic flow.] SAMJ: South African Medical Journal. 2016 Apr;106(4):328-9.</ref> | |||
* [[ | *[[Pneumonia]]<ref name=":4" /><ref name=":7" /> | ||
* [[ | * Myocarditis<ref name=":7" /> | ||
* [[ | * [[Cystic Fibrosis]]<ref name=":7" /> | ||
* [[Human Immunodeficiency Virus (HIV)|HIV]]/ [[Tuberculosis]]<ref name=":7" /> | |||
== Management / Interventions == | == Management / Interventions == | ||
*Hydration | *Bronchodilators - not advised routinely and if it is used, careful monitoring should occur.<ref name=":4" /> | ||
* | *Nebulised hypertonic saline - not advised.<ref name=":4" /><ref name=":8" /> | ||
*Nasal | *Corticosteroids - not advised.<ref name=":4" /><ref name=":8" /> | ||
* | *High-flow oxygen - only needed when oxygen saturation is below 90% (some studies say below 92%)<ref name=":4" /><ref name=":8" /> | ||
*Hydration<ref name=":4" /> | |||
*Suctioning - not routinely recommended <ref name=":4" /><ref name=":8" /> | |||
*Antibiotics - not to be used unless confirmed infection<ref name=":4" /><ref name=":8" /> | |||
*Nasal CPAP<ref name=":8" /> | |||
*Chest physiotherapy - not recommended<ref name=":4" /><br> | |||
== Key Evidence regarding physiotherapy == | |||
In the Cochrane review titled "Chest physiotherapy for acute bronchiolitis in children younger than two years of age", it was concluded that none of the chest physiotherapy techniques (vibrations, percussions, slow passive expiratory techniques or forced expiratory techniques) have demonstrated a reduction in the severity of disease. Hence, these techniques cannot be used as standard clinical practice for hospitalised patients with severe bronchiolitis.<ref>Roqué i Figuls M, Giné-Garriga M, Granados Rugeles C, Perrotta C, Vilaró J. Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database of Systematic Reviews 2016, Issue 2. Art. No.: CD004873. DOI: 10.1002/14651858.CD004873.pub5.</ref> | |||
A state-of-art review suggests avoiding repeated airway clearance in infants and children with acute pulmonary disease.<ref>Morrow BM. [https://www.ncbi.nlm.nih.gov/pubmed/31309166 Airway clearance therapy in acute paediatric respiratory illness: A state-of-the-art review.] South African Journal of Physiotherapy. 2019 Jun 25;75(1):12.</ref> | |||
An RCT was conducted in ninety-one non-hospitalised infants (mean age 7.9 ± 2.6 months) with mild to moderate bronchiolitis, the results showed that high-frequency chest wall compression (HFCWC) was effective and safe in reducing the severity of respiratory symptoms<ref>González-Bellido V, Velaz-Baza V, Blanco-Moncada E, Esteo MD, Cuenca-Zaldívar JN, Colombo-Marro A, Donadio MV, Torres-Castro R. Immediate effects and safety of high-frequency chest wall compression compared to airway clearance techniques in non-hospitalized infants with acute viral bronchiolitis. Respiratory Care. 2021 Mar 1;66(3):425-33.</ref> | |||
According to the Italian guidelines on the management of bronchiolitis in infants, it was recommended that gentle nasal aspiration, O2 therapy, adequate feeding and hydration are the main essential treatment techniques in handling infants with bronchiolitis<ref>Manti S, Staiano A, Orfeo L, Midulla F, Marseglia GL, Ghizzi C, Zampogna S, Carnielli VP, Favilli S, Ruggieri M, Perri D. UPDATE-2022 Italian guidelines on the management of bronchiolitis in infants. Italian Journal of Pediatrics. 2023 Feb 10;49(1):19.</ref>. The authors concluded that deep nasal aspiration, chest physiotherapy, inhaled bronchodilators, nebulised adrenaline, nebulised and systemic corticosteroids, antibiotics, and other therapies are not routinely recommended in treating bronchiolitis. Preventive measures through parental education and de-implementation of low quality evidence-based treatment should be emphasised to reduce morbidity in these cases. | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Paediatrics]] | |||
[[Category:Paediatrics - Conditions]] | |||
[[Category:Cardiopulmonary]] | |||
[[Category:Acute Respiratory Disorders - Conditions]] | [[Category:Acute Respiratory Disorders - Conditions]] | ||
Latest revision as of 07:09, 30 April 2023
Original Editor - Jerome Ng
Top Contributors - Jerome Ng, Kim Jackson, Donald John Auson, Wendy Snyders, Naomi O'Reilly, WikiSysop, Adam Vallely Farrell, Vidya Acharya and Candace Goh
Clinically Relevant Anatomy[edit | edit source]
The bronchioles do not have cartilage[1] where the bronchi have a firbrocartilaginous framework[2]. They are the final air conductors and do not have alveoli.[1]There are about 30000 terminal bronchioles, each of which directs air to about 10000 alveoli.[1] Bronchioles have a continuous circular layer of smooth muscle and the bronchi mucosa is continuous with the mucosa of the bronchioles.[2] The mucociliary blanket of the bronchioles is a watery fluid that accumulates muscous as it ascends the airway.[2]
Epidemiology[edit | edit source]
In the first year of life, bronchiolitis is the most common lower respiratory tract infection.[3][4]. It affects one in five infants and 2%-3% require admission to hospital.[3] It also has a seasonal predilection, with more infections during the winter.[5][6]
Etiology[edit | edit source]
Bronchiolitis is usually caused by the Respiratory Syncytial Virus (RSV).[7][6] Other pathogens can also cause bronchiolitis such as human rhinovirus, influenza virus, coronavirus, human metapneumovirus (hMPV) and parainfluenza virus.[7]
Pathogenesis due to RSV[edit | edit source]
Inoculation of the conjunctival or nasal mucosa by contaminated secretions or inhalation of large respiratory droplets that contain the virus leads to infection. There is an incubation period of 4 - 6 days and then viral replication in the nasal epithelium leads to symptoms. Once the virus has spread to the lower respiratory tract, the alveolar pneumocytes and the ciliated epithelial cells of the mucosa of the bronchioles become infected. Impaired ciliary beating and the sloughing of the infected epithelium causes intraluminal obstruction. The bronchiolar epithelium starts to regenerate within 3 to 4 days after symptom resolution.[8]
Clinical Presentation[edit | edit source]
- Rhinorrhea (early presentation)[6][8]
- Nasal congestion[8]
- Cough[6][8]
- Tachypnoea[6][8]
- Increased work of breathing[6][8]
- Crackles and wheezing on auscultation[6][8]
Diagnosis[edit | edit source]
Diagnosis can be made through physical examination and history taking.[8][6] Clinical practice guidelines indicate that chest x-rays and laboratory studies should not be routine[8][6]. Pulse oximetry has received increased attention in studies and clinical guidelines.[6] Chest x-rays should only be done in severe cases, if complications are suspected, if the diagnosis un unclear and if the child does not respond to treatment.[9]Blood tests should only be done in severe cases.[9]
Differential Diagnosis[edit | edit source]
Management / Interventions[edit | edit source]
- Bronchodilators - not advised routinely and if it is used, careful monitoring should occur.[6]
- Nebulised hypertonic saline - not advised.[6][4]
- Corticosteroids - not advised.[6][4]
- High-flow oxygen - only needed when oxygen saturation is below 90% (some studies say below 92%)[6][4]
- Hydration[6]
- Suctioning - not routinely recommended [6][4]
- Antibiotics - not to be used unless confirmed infection[6][4]
- Nasal CPAP[4]
- Chest physiotherapy - not recommended[6]
Key Evidence regarding physiotherapy[edit | edit source]
In the Cochrane review titled "Chest physiotherapy for acute bronchiolitis in children younger than two years of age", it was concluded that none of the chest physiotherapy techniques (vibrations, percussions, slow passive expiratory techniques or forced expiratory techniques) have demonstrated a reduction in the severity of disease. Hence, these techniques cannot be used as standard clinical practice for hospitalised patients with severe bronchiolitis.[10]
A state-of-art review suggests avoiding repeated airway clearance in infants and children with acute pulmonary disease.[11]
An RCT was conducted in ninety-one non-hospitalised infants (mean age 7.9 ± 2.6 months) with mild to moderate bronchiolitis, the results showed that high-frequency chest wall compression (HFCWC) was effective and safe in reducing the severity of respiratory symptoms[12]
According to the Italian guidelines on the management of bronchiolitis in infants, it was recommended that gentle nasal aspiration, O2 therapy, adequate feeding and hydration are the main essential treatment techniques in handling infants with bronchiolitis[13]. The authors concluded that deep nasal aspiration, chest physiotherapy, inhaled bronchodilators, nebulised adrenaline, nebulised and systemic corticosteroids, antibiotics, and other therapies are not routinely recommended in treating bronchiolitis. Preventive measures through parental education and de-implementation of low quality evidence-based treatment should be emphasised to reduce morbidity in these cases.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Leslie KO, Wick MR. Bronchiole [Internet]. Bronchiole - an overview | ScienceDirect Topics. [cited 2023Jan14]. Available from: https://www.sciencedirect.com/topics/immunology-and-microbiology/bronchiole
- ↑ 2.0 2.1 2.2 Lust RM. Bronchiole [Internet]. Bronchiole - an overview | ScienceDirect Topics. [cited 2023Jan14]. Available from: https://www.sciencedirect.com/topics/immunology-and-microbiology/bronchiole
- ↑ 3.0 3.1 Ricci V, Nunes VD, Murphy MS, Cunningham S. Bronchiolitis in children: summary of NICE guidance. Bmj. 2015 Jun 2;350.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 O'Brien S, Borland ML, Cotterell E, Armstrong D, Babl F, Bauert P, Brabyn C, Garside L, Haskell L, Levitt D, McKay N. Australasian bronchiolitis guideline. Journal of paediatrics and child health. 2019 Jan;55(1):42-53.
- ↑ Bronchiolitis. nhs.uk. [cited 13 April 2020]. Available from: https://www.nhs.uk/conditions/bronchiolitis/
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 6.18 6.19 Florin TA, Plint AC, Zorc JJ. Viral bronchiolitis. The Lancet. 2017 Jan 14;389(10065):211-24.
- ↑ 7.0 7.1 Miller EK, Gebretsadik T, Carroll KN, et al. Viral etiologies of infant bronchiolitis, croup and upper respiratory illness during 4 consecutive years. Pediatr Infect Dis J. 2013;32(9):950–955. doi:10.1097/INF.0b013e31829b7e43 Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3880140/
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 Meissner HC. Viral bronchiolitis in children. New England Journal of Medicine. 2016 Jan 7;374(1):62-72.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 White DA, Zar HJ, Madhi SA, Jeena P, Morrow B, Masekela R, Risenga S, Green RJ. Acute viral bronchiolitis in South Africa: Diagnostic flow. SAMJ: South African Medical Journal. 2016 Apr;106(4):328-9.
- ↑ Roqué i Figuls M, Giné-Garriga M, Granados Rugeles C, Perrotta C, Vilaró J. Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database of Systematic Reviews 2016, Issue 2. Art. No.: CD004873. DOI: 10.1002/14651858.CD004873.pub5.
- ↑ Morrow BM. Airway clearance therapy in acute paediatric respiratory illness: A state-of-the-art review. South African Journal of Physiotherapy. 2019 Jun 25;75(1):12.
- ↑ González-Bellido V, Velaz-Baza V, Blanco-Moncada E, Esteo MD, Cuenca-Zaldívar JN, Colombo-Marro A, Donadio MV, Torres-Castro R. Immediate effects and safety of high-frequency chest wall compression compared to airway clearance techniques in non-hospitalized infants with acute viral bronchiolitis. Respiratory Care. 2021 Mar 1;66(3):425-33.
- ↑ Manti S, Staiano A, Orfeo L, Midulla F, Marseglia GL, Ghizzi C, Zampogna S, Carnielli VP, Favilli S, Ruggieri M, Perri D. UPDATE-2022 Italian guidelines on the management of bronchiolitis in infants. Italian Journal of Pediatrics. 2023 Feb 10;49(1):19.