Bronchiolitis: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Categorisation) |
||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Clinically Relevant Anatomy | == Clinically Relevant Anatomy == | ||
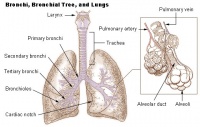
Bronchiolitis is inflammation of the [https://en.wikipedia.org/wiki/Bronchiole bronchioles], the smallest air passages of the lungs, in which air passes through the nose or mouth to the alveoli of the lungs where gas exchange takes place.[[Image:Lung anatomy.jpg|thumb|right|200px]] | Bronchiolitis is inflammation of the [https://en.wikipedia.org/wiki/Bronchiole bronchioles], the smallest air passages of the lungs, in which air passes through the nose or mouth to the alveoli of the lungs where gas exchange takes place.[[Image:Lung anatomy.jpg|thumb|right|200px]] | ||
== Mechanism of Injury / Pathological Process | == Mechanism of Injury / Pathological Process == | ||
Bronchiolitis typically occurs with primary infection or reinfection with a viral pathogen, but occasionally is caused by bacteria (eg, Mycoplasma pneumoniae). In young children, the clinical syndrome of bronchiolitis may overlap with recurrent virus-induced wheezing and acute viral-triggered asthma.<br> | Bronchiolitis typically occurs with primary infection or reinfection with a viral pathogen, but occasionally is caused by bacteria (eg, Mycoplasma pneumoniae). In young children, the clinical syndrome of bronchiolitis may overlap with recurrent virus-induced wheezing and acute viral-triggered asthma.<br> | ||
| Line 21: | Line 21: | ||
*Acute respiratory failure<br> | *Acute respiratory failure<br> | ||
== Management / Interventions | == Management / Interventions == | ||
*Hydration | *Hydration | ||
| Line 37: | Line 37: | ||
== Key Evidence == | == Key Evidence == | ||
In the Cochrane review titled "Chest physiotherapy for acute bronchiolitis in children younger than two years of age", it was concluded that none of the chest physiotheray techniques (vibrations, percussions, slow passive expiratory techniques or forced expiratory techniques) have demonstrated a reduction in the severity of disease. Hence, these tecniques cannot be used as standard clinical practice for hospitalised patients with severe bronchiolitis.<ref>Roqué i Figuls M, Giné-Garriga M, Granados Rugeles C, Perrotta C, Vilaró J. Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database of Systematic Reviews 2016, Issue 2. Art. No.: CD004873. DOI: 10.1002/14651858.CD004873.pub5.</ref><br | In the Cochrane review titled "Chest physiotherapy for acute bronchiolitis in children younger than two years of age", it was concluded that none of the chest physiotheray techniques (vibrations, percussions, slow passive expiratory techniques or forced expiratory techniques) have demonstrated a reduction in the severity of disease. Hence, these tecniques cannot be used as standard clinical practice for hospitalised patients with severe bronchiolitis.<ref>Roqué i Figuls M, Giné-Garriga M, Granados Rugeles C, Perrotta C, Vilaró J. Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database of Systematic Reviews 2016, Issue 2. Art. No.: CD004873. DOI: 10.1002/14651858.CD004873.pub5.</ref><br> | ||
== References == | |||
== References | |||
<references /> | <references /> | ||
[[Category:Cardiopulmonary]] | [[Category:Cardiopulmonary]] | ||
[[Category:Conditions - Acute Respiratory Disorders]] | |||
Revision as of 14:07, 13 April 2019
Original Editor - Jerome Ng
Top Contributors - Jerome Ng, Kim Jackson, Donald John Auson, Wendy Snyders, WikiSysop, Adam Vallely Farrell, Vidya Acharya, Candace Goh and Naomi O'Reilly
Clinically Relevant Anatomy[edit | edit source]
Bronchiolitis is inflammation of the bronchioles, the smallest air passages of the lungs, in which air passes through the nose or mouth to the alveoli of the lungs where gas exchange takes place.
Mechanism of Injury / Pathological Process[edit | edit source]
Bronchiolitis typically occurs with primary infection or reinfection with a viral pathogen, but occasionally is caused by bacteria (eg, Mycoplasma pneumoniae). In young children, the clinical syndrome of bronchiolitis may overlap with recurrent virus-induced wheezing and acute viral-triggered asthma.
Clinical Presentation[edit | edit source]
Bronchiolitis is a major cause of illness and hospitalization in infants and children younger than two years. Symptoms include:
- Persistently increased respiratory effort (tachypnea, nasal flaring, intercostal or suprasternal retractions, accessory muscle use, grunting)
- Hypoxemia
- Apnea
- Acute respiratory failure
Management / Interventions[edit | edit source]
- Hydration
- Respiratory support
- Nasal suctioning
- Supplemental oxygen
The following are interventions that may be used, but not as a routine intervention:
- Trial of inhaled bronchodilator
- Nebulized hypertonic saline
- Glucocorticoids
- Chest physiotherapy
Key Evidence[edit | edit source]
In the Cochrane review titled "Chest physiotherapy for acute bronchiolitis in children younger than two years of age", it was concluded that none of the chest physiotheray techniques (vibrations, percussions, slow passive expiratory techniques or forced expiratory techniques) have demonstrated a reduction in the severity of disease. Hence, these tecniques cannot be used as standard clinical practice for hospitalised patients with severe bronchiolitis.[1]
References[edit | edit source]
- ↑ Roqué i Figuls M, Giné-Garriga M, Granados Rugeles C, Perrotta C, Vilaró J. Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database of Systematic Reviews 2016, Issue 2. Art. No.: CD004873. DOI: 10.1002/14651858.CD004873.pub5.