Breast Cancer
Brikena Campbell, Adam El-Sayed, Kirsty Graham, Chris Noble, Natalie Riley, Aidan Slattery- Your name will be added here if you created the original content for this page.
Top Contributors - Adam El-Sayed, Kim Jackson, Lucinda hampton, Vidya Acharya, Admin, Chee Wee Tan, Ilona Malkauskaite, Candace Goh, Manisha Shrestha and 127.0.0.1
Introduction
[edit | edit source]
The evolving role of physiotherapy in breast cancer care[edit | edit source]
There is a growing evidence base reporting the physiological and psychological benefits of physiotherapy as a safe and effective adjunct to breast cancer treatment (Eyigor et al. 2014).
With survival rates at an all time high the National Cancer Survivorship Initiative (NCSI) Vision (Department of Health) has stated that health professionals must now focus on meeting the unique needs of breast cancer survivors and improve accessibility to specialist services, including physiotherapy. Services ideally will be able to deliver physiotherapy interventions to better empower patients in the management of their symptoms, side-effects of treatment or recovery from surgery. (link to effects of cancer section)
Recent novel physiotherapy programs such as “The Specialist Breast Care Physiotherapy Service (2010)” are now being developed and implemented by the NHS to provide support to the growing population of survivors. It is therefore imperative that physiotherapists are prepared to deliver a high standard of care through such initiatives.
Recent developments in Scotland[edit | edit source]
(WAITING FOR CONSENT), a physiotherapist based at the (WAITING FOR CONSENT) is one such individual who is actively promoting and evolving the role of the physiotherapist in breast cancer care. As Project Manager for (WAITING FOR CONSENT), she is tackling the issue of cancer survivorship through promotion of physical activity after cancer and investigating what community services are available to support patients partaking in physical activity. Ellen's project has developed a guidance document, a policy about physical activity and cancer as well as a patient leaflet to provide basic information about physical activity. The plan next is to do educate staff to tell them about what message to give patients regarding physical activity during and after treatment and to put together resources to tell staff about community services that are available.
“My ultimate hope is that we might be able to consider something like a pulmonary rehab or like a cardiac rehab program for cancer survivors.” - CONSENT
The need for physiotherapist education in breast cancer patient care[edit | edit source]
This educational resource was inspired by the biopsychosocial model of health care proposed by the World Health Organisation and the NCSI's recent call for greater support and services for cancer survivors. Breast cancer patients face an array of problems and have specific needs which must be addressed in order to prevent long term functional limitations and disability (see Adams section). The physiological and psychological benefits from physiotherapy for breast cancer patients are well documented, with improvements observed in terms of morbidity, mortality and importantly, quality of life (Pidlyskyj et al. 2014). Thus, the potential role for physiotherapists in this area is clear to see and highlights the importance of training for physiotherapists to develop the skills required to meet patient needs and maximise their contribution to the MDT.
Audience[edit | edit source]
The resource was produced for use by Band 6 physiotherapists may be of benefit to other health professionals seeking background knowledge.
Learning Outcomes[edit | edit source]
- To devise and discuss a long-term management strategy for breast cancer patients, including return to work and prevention of cancer recurrence.
- To practice effective communication methods when treating breast cancer patients.
- To justify the key role of the physiotherapist in a breast cancer patient multidisciplinary team.
- To value a healthy life style approach to the prevention of breast cancer and care of breast cancer patients and implement this in patient-centred care
- To facilitate contemporary skills development in the field of physiotherapy with breast cancer patients.
- To inspire autonomous engagement in the emerging role of physiotherapy in breast cancer.
- To promote and display a biopsychosocial approach to the care of breast cancer patients.
- To acquire the necessary knowledge and skills to display effective behaviours and values of contemporary physiotherapy practice.
Breast cancer epidemiology and pathophysiology [edit | edit source]
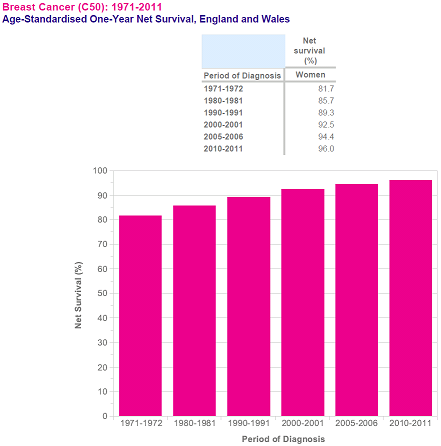
Breast cancer prevalence and survival rates [edit | edit source]
Breast cancer is the most common cancer in the UK. An estimated 1 in 8 women in the UK will develop breast cancer in their lifetime and the incidence of breast cancer has risen by 7% in the last 10 years. In part this may reflect the effectiveness of NHS screening programs (16,500 cases were detected in 2009 alone) however increasing incidence is also a global issue with an estimated 1.68 million diagnoses made in 2012 worldwide (Cancer Research UK).
Survival rates are also increasing. Today, more women are surviving breast cancer than ever before. Most recent figures reported by Information Services Division Scotland showed that high percentages of women diagnosed with breast cancer in Scotland between 2003 and 2007 were surviving 1 year (93.8%) and 5 years post diagnosis (81.4%). Similar trends have been reported for the rest of the UK (Cancer Research UK).
([Cancer Research UK][1])
Cellular mechanism of cancer development[edit | edit source]
Cancer cells differ from normal cells in the (dis)regulation of cell division and growth. As a normal cell develops into a neoplastic state, the cell undergoes changes in six forms.
- Sustaining proliferation: cancer cells change growth promoting signals by altering pro-ocogenes to oncogenes thereby disrupting the homeostasis of cell structure and function. This results in sustained chronic proliferation without external stimulation.
- Evading growth suppressors: by overcoming the effects of tumour suppressing genes that prevent cell growth, tumours are able to grow uninhibited.
- Resisting cell death (apoptosis): the spread of cancer cells may be escalated due to a rise in gene mutations leading to ineffective programmed cell death.
- Enabling replicative immortality: in normal cells telomere shortening causes cell division to stop. Cancer cells enable widespread self-replication using the enzyme telomerase to prevent telomere shortening, allowing repeated cell division without DNA shortening.
- Sustained angiogenesis: as in normal cells angiogenesis allows cancer cells to acquire nutrients and oxygen with the elimination of metabolic waste and carbon dioxide. Subsequently a vascular system is created to maintain tumour growth and metastasis.
- Activating invasion and metastasis: the spread of cancer cells is made possible when cells break free from the primary tumour and enter the blood and lymphatic vessels. Subsequently the development of a second tumour may occur in different site of the body to the primary tumour (Langthorne et al. 2007).
Pathophysiology in breast cancer[edit | edit source]
- Non-invasive breast cancers are present in the ducts or lobules.
- Invasive cancers are found in the surrounding breast tissue.
- Cell Grade: Cells are graded in a system where grade 1 cancer cells present slightly differently to normal cells, progressing to grade 3 cancer cells which demonstrate major differences to a normal cells.
- Tumour Necrosis: tumour necrosis may be present in aggressive forms of breast cancer where cells are seen to grow at a rapid rate.
- This is often a sign of a rapidly growing aggressive form of breast cancer.
- Vascular or Lymphatic Invasion: - these types of invasion describe whether or not cancerous cells are evident in the vascular and lymphatic vessels supplying the breast tissue.
- Hormone Receptor Status: - Hormone receptor status determines if hormone therapy would be appropriate.
- HER2 Status: - HER2 is a gene that when dysfunctional can play a role in the development of breast cancer. Breast cancers that are HER2 positive tend to grow faster and are more likely to spread that those that are HER2 negative.
Physical effects of breast cancer treatment and physiotherapy intervention[edit | edit source]
Musculoskeletal problems experienced in breast cancer patients[edit | edit source]
- Subacromial Impingement Syndrome.
- Adhesive Capsulitis (frozen shoulder) – idiopathic or traumatic (post-surgery).
- Rotator Cuff pathology (e.g Symptomatic Rotator Cuff Disease)
- Myofascial Dysfunction Lateral epicondylitis.
- Scapular winging secondary to damage of long thoracic nerve during surgery.
- Pain
Symptomatic Rotator Cuff Disease[edit | edit source]
The breast cancer patient is also quite susceptible to the development of symptomatic rotator cuff disease, which can be brought on through intrinsic factors such as age related physiological changes to the tendons, or through extrinsic factors brought on from cancer treatment such as lymphedema as well as shoulder girdle resting alignment. Tension overload on the rotator cuff tendons may be increased secondary to increased volume and weight of the effected limb with the presence of lymphedema. Due to pain, or fear of movement, for example, the breast cancer patient may adapt to a new resting position for their shoulder, and may tend to avoid using the limb, resulting in shortening of the muscles, and tightening of the joint capsule (Ebaugh, Spinelli, and Schmitz, 2011). Moreover, patients tend to adapt a flexed and protective posture following surgery, further increasing the likelihood of muscle shortening. Pectoralis major is commonly effected. Tightness of these muscles tend to lead to a pull on the scapula, causing it to become protracted and depressed, leading to scapular winging, as well as shoulder impingement (Păcurar et. al, 2011).
Post Mastectomy Pain Syndrome (PMPS)[edit | edit source]
Pain which lasts longer than what is usually expected following various breast cancer surgery types. Generally neuropathic in nature, and can be due but not limited to:
- Brachial nerve damage,
- Intra-operative compromise of cutaneous innervating,
- Neuroma formation,
- Fibrotic entrapment.
Patients often report neurological symptoms such as numbness or pins and needles, stabbing and burning pain to the same side as surgery in or around the surgical sites. These symptoms can be exacerbated through a lack of pacing, or by lying on the side of surgery. Therefore, patient education, soft tissue massage, and other desensitising techniques are essential (Păcurar et. Al, 2011).
Associated Neuromusculoskeletal Conditions following treatment[edit | edit source]
Neuromusculoskeletal conditions are common following surgery, some of which are illustrated in figure 1.4. Treatment protocols shall not be discussed, and the reader should refer to the basic principles of rehabilitation of musculoskeletal conditions. In light of this, it is important to briefly discuss a few points to consider.
- Depending on the type of surgery that the patient needs to undertake, radiotherapy may be necessary following surgery.
- A typical radiotherapy session will require the patient to position the treated arm to 90° flexion and abduction, as well as maximal external rotation, for up to 30 minutes (Johnson & Musa, 2004).
- Shoulder mobility is commonly affected post-surgery (Dahl et. al, 2011; Freitas-Silva et. al, 2010; Harrington et. al, 2011; Hardie et al, 2011 ) so it is vital that physiotherapy aims to restore this to improve patient functional ability and to be able to place the shoulder in the required positions for radiotherapy.
- Active, active assisted, and passive ROM exercises for the shoulder girdle are therefore good practice. Physiotherapy should aim to restore full shoulder ROM as well as minimising associated upper extremity morbidity (Todd & Topping, 2005).
- Manual therapy techniques with the aim of further increasing available ROM have been shown to not be of any significant benefit when used in conjunction with active upper limb exercises (do Amaral et. al, 2012).
“We see people post mastectomy and people who have had axillary node clearances. We give them lymphodema advice, prevention advice at the beginning and we see them for shoulder ROM exercises. We might then follow up with them as an out patients if they've got limited shoulder ROM or they develop cording.” – (AWAITING CONSENT)
Musculoskeletal Physiotherapy Interventions Post Surgery[edit | edit source]
Most commonly patients will undergo radiotherapy after surgery. An adequate ROM of 140°-150° shoulder flexion is required in order for radiotherapy to commence.
A physiotherapists treatment plan should include:
- Motion exercises to improve tissue extensibility and facilitate normal movement patterns.
- Myofascial release for enhancing mobility and enhancing tissue extensibility.
(McAnaw and Harris 2002; Levangie and Drouin 2009; Ebaugh et al. 2011 and Păcurar et al. 2011
Reduced range of motion and lymphedema[edit | edit source]
The two most common complications that are evident in breast cancer patients are restricted arm motion and lymphedema. These result in the occurrence of pain at the place of operation and muscle spasms are quite common. It is very important that early rehabilitation is implemented to promote functional movement to the patient’s previous level of activity. Subsequent to operation arm mobilisations are implemented first or second day post-op. Mobilisations are performed using joint rotations to tolerance but abduction and flexion are limited to 40°. At day 4 post-op flexion and abduction are gradually increased to 45°, this can be increased furthermore by 10-15° per day dependent on the patient’s pain tolerance. The technique performed by holding the patients arm in 45° flexion or abduction until the drains are removed. Secondary lymphedema is a common occurrence in the breast cancer population following surgery and has a long term negative effect on patient quality of life. Risk factors that are prevalent in the breast cancer population are age, obesity and the growing survival rate. The growing risk factors make secondary lymphedema a challenging complication in the breast cancer population.
Physiotherapy strategies for lymphedema[edit | edit source]
Complex decongestive physiotherapy for lymphedema[edit | edit source]
This is a treatment that incorporates skin hygiene, manual lymph drainage, bandaging, exercises and support garments.
Manual lymphoedema drainage is a massage technique that involves the skin surface only. This follows the anatomical lymphatic pathway. Generally the manual lymph drainage technique will begin centrally in the neck and trunk to alleviate any lymphedema in the main lymphatic pathway, so that drainage in the arm is facilitated.
Complex decongestive physiotherapy has been suggested as the primary treatment for breast cancer patients. This treatment includes skin care, exercises, compression and manual lymphedema treatment. Complex decongestive physiotherapy has shown to be an effective method for the treatment of lymphedema when standard elastic compression has been unsuccessful. One study showed consistent results of the reduction in volume of the effected extremity in 95% of 400 patients. A follow-up showed that these therapeutic results were maintained at 3 years.
Elevation[edit | edit source]
Elevation has been described as a non-effective treatment when performed solely in breast cancer treatment for arm related oedema. Elevation is commonly used together with other treatments to provide the most effective treatment. Most commonly in breast cancer treatment a multidisciplinary approach is taken where the patient will undergo massage and exercise. A specific technique of massage is commonly implemented named manual lymphatic drainage. Manual lymphatic drainage is a type of massage used to mobilise oedema fluid from distal to proximal areas and from areas of stasis to healthy lymphatics.
Compression[edit | edit source]
One form of lymphedema treatment which has proved most effective in the treatment of breast cancer patients is the use of standard elastic compression garments. Studies have shown significant improvements using simple elastic compression treatment for lymphedema, where 34% of patients showed a substantial reduction in arm oedema at 2 months and 39% of patients at 6 months. This conclusion was also seen in patients older than 65 years old (Torres et al, 2010).
Physiotherapy to prevent secondary lymphedema arising[edit | edit source]
- Stretching for muscles of the shoulder: Levator scapulae; upper trapezius; pectoralis major and the medial and lateral rotators of the shoulder
- Progressive active and active assisted shoulder exercises.
- Functional exercise activities.
- Proprioceptive neuromuscular facilitation exercises.
Breast cancer treatments involving the MDT[edit | edit source]
Multi-Disciplinary Teams (MDTs)[edit | edit source]
Due to the complex nature of cancer and the treatment process that accompanies the condition, the condition requires expert input across of wide range of health professionals (Saini et. al, 2012). In light of this, there is potential for miscommunication on occasion. A solid MDT should improve communication between health professionals, which should optimize the treatment process for the breast cancer patient (Fleissig, Jenkins, Catt, and Fallowfield, 2006).
“There's quite a lot of people that we have to know about and know how to access their services and know what their skills are.”, “We quite often will communicate with medical staff, nursing staff, nurse practitioners, the clinic nurse specialists...” – (AWAITING CONSENT)
Surgery[edit | edit source]
Surgery is performed in order to remove as many cancer cells as possible, to investigate where the cancer cells have spread to, for reconstruction, or to reduce symptoms in the later stages of cancer. Below is a brief outline of the common procedures.
Selection criteria for surgery:
- The size of the tumour present and the location
- Whether or not the cancer cells have spread
- Breast size
- Personal wishes of the patient
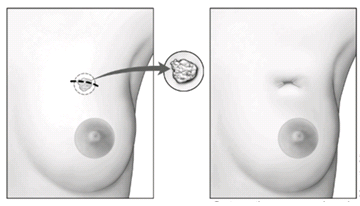
Excisional Breast Biopsy (Lumpectomy)[edit | edit source]
- A lumpectomy, otherwise known as a wide local excision, tends to be used in early stage cancer or when the tumour is of small size.
- The surgeon will remove the cancer cells, as well as some of the healthy tissue which surrounds the affected area.
- This can be done with general or local anaesthetic, with the aim of determining the mass of the tumour and to rule out any carcinoma.
- Due to the conserving nature of this procedure, it is one that is favoured by the breast cancer population, and has even been shown to have no significant difference in survival rate when compared with a mastectomy (Fisher et. al, 2002).
- The excised tumour is examined further for cancerous cells, if which are found around the edges, may lead to further surgery or mastectomy.
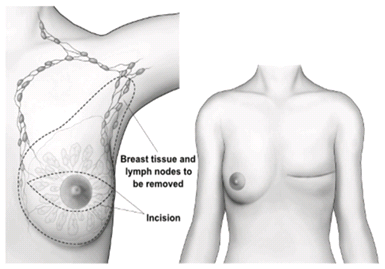
Subcutaneous Mastectomy (Complete Mastectomy)[edit | edit source]
- This procedure results in complete removal of the breast tissue only (>99% of breast tissue), where a carcinoma is in situ.
- When the size of the tumour is large in proportion to the rest of the breast tissue, or is wide spread, a mastectomy is performed.
- As previously mentioned, a mastectomy may be performed if a lumpectomy is unsuccessful in the removal of all cancer cells.
- It may also be performed if cancer cells were to recur following other treatments such as radiotherapy.
- Occasionally, complete removal of the pectoralis muscle group can occur if cancer cells were to spread into the musculature.
Modified Radical Mastectomy (MRM)[edit | edit source]
- MRM indicated where:
- Tumour location, size, and presence of multiple cancer cells in the breast tissue.
- Where radiotherapy is contraindicated.
- Dissection and removal of the lymph nodes within the axilla occurs. The likeliness of morbidity in the arm (Beurskens, van Uden, Strobbe, Oostendorp, and Wobbes, 2007) is increased and can even lead to permanent lymphedema depending on the amount of lymph nodes removed.
- Dissection sites:
- Lateral edge of the sternum, clavicle, within latissimus dorsi, rectus sheath
- Breast tissue’s usually dissected from the pectoralis muscle; occasionally compromised.
- Strain injuries to the brachial plexus are common, but usually resolve over time.
- Injuries to the long thoracic nerve are quite common following this particular surgery.
- Loss of range of motion (ROM) in the glenohumeral joint (GHJ) is quite common following this procedure, physiotherapy has been shown to manage this (Beurskens et. al, 2007).
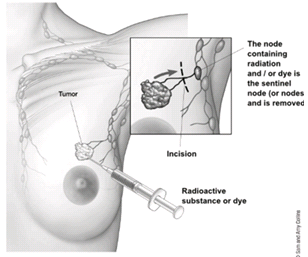
Sentinel Lymph Node Biopsy[edit | edit source]
- Radioactive dye is injected into the breast tissue as a further diagnostic measure to evaluate whether the cancer cells have entered the lymph nodes or not.
- Once identified, the lymph nodes containing the cancer cells, i.e. the sentinel lymph nodes, are then removed surgically.
Referrals to physiotherapy[edit | edit source]
Referral process[edit | edit source]
PT and the future of Ca Rx[edit | edit source]
Also include opinions about research that is going both directions (trends that are dying)[edit | edit source]
Tying it all together[edit | edit source]
Self-assessment quiz[edit | edit source]
Reflection[edit | edit source]
Recent Related Research[edit | edit source]
References[edit | edit source]
References will automatically be added here, see adding references tutorial.