Brachial Plexus
Original Editor - Matt Anderson
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Introduction[edit | edit source]
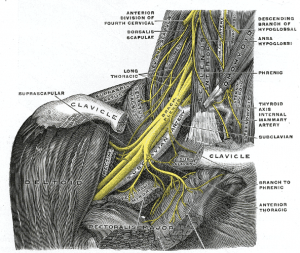
The Brachial Plexus is a network of nerve fibers that run from the spine, passing through the cervico-axillary canal to reach axilla. It is formed by the ventral rami of the lower four cervical and first thoracic nerve roots (C5-C8, T1).
Function[edit | edit source]
The brachial plexus is responsible for cutaneous and muscular innervation of the entire upper limb, with two exceptions: the trapezius muscle innervated by the spinal accessory nerve (CN XI) and an area of skin near the axilla innervated by the intercostobrachial nerve.
Description[1]
[edit | edit source]
The long thoracic nerve has an origin from C5-C7, with the dorsal scapular nerve branching off the C5 distribution of the long thoracic nerve. The trunks are formed by the joining of C5 and C6 (Upper Trunk), C7 alone (Middle Trunk), and C8 and T1 joining (Lower Trunk). Each of the three trunks divide.. The two anterior divisions originating from the upper and middle trunks combine to form the Lateral Cord. The three posterior divisions combine, one from each trunk, to form the Posterior Cord. The lower trunk splits to provide one of the posterior divisions and one anterior division. The anterior division becomes the Medial Cord. The cords then branch to become the main branches. The lateral cord branches to become the Musculocutaneous Nerve (C4,5,6). The lateral and medial cord branch to become the Median Nerve (C5-8, T1). The medial cord also branches to for the Ulnar Nerve (C8-T1) and the Medial antebrachial cutaneous nerve (C8-T1). Other smaller nerves originate from the roots, trunks and cords.
The brachial plexus is divided into Roots, Trunks, Divisions, Cords, and Branches. There are five "terminal" branches and numerous other "pre-terminal" or "collateral" branches that leave the plexus at various points along its length.
- The five Roots are the five anterior rami of the of the lower four cervical and first thoracic nerve roots (C5-C8, T1), after they have given off their segmental supply to the muscles of the neck.
- These Roots merge to form three Trunks:
- Upper Trunk (C5-C6)
- Middle Trunk (C7)
- Lower Trunk (C8, T1)
- Each Trunk then splits into anterior and posterior divisions, to form six Divisions. The anterior/ posterior divisions innervate flexor groups versus extensor groups:
- anterior divisions of the upper, middle, and lower trunks
- posterior divisions of the upper, middle, and lower trunks
- These six Divisions will regroup to become the three Cords. The Cords are named by their position with respect to the axillary artery.
- The Posterior Cord is formed from the three posterior divisions of the trunks (C5-C8,T1)
- The Lateral Cord is the anterior divisions from the upper and middle trunks (C5-C7)
- The Medial Cord is simply a continuation of the anterior division of the lower trunk (C8,T1)
The branches are listed below. Most branch from the cords, but a few branch (indicated in italics) directly from earlier structures. The five on the left are considered "terminal branches".
Injuries[1]
[edit | edit source]
Injury to the brachial plexus can be very problematic because the nerves branching off of the plexus provide innervation to the upper extremity. Clinical signs and symptoms vary with which area of the plexus is involved, and can generally result in paralysis or anesthesia. Brachial plexus injury can occur in a variety of ways. During birth, excessive stretching of the neck or pulling the upper extremity can result in an upper brachial plexus injury or inferior trunk, respectively. An adult can injury the brachial plexus by landing on the neck in a way that separates the neck from the shoulder, or from a traction injury.
The most common forms of injury include Erb Palsy (upper brachial plexus palsy) and Klumpke’s Palsy (lower brachial plexus injury). The characteristics of Erb Palsy include a waiter’s tip position (arm lies in internal rotation, elbow extended, forearm pronated, wrist and fingers flexed). The characteristics of Klumpke’s Palsy include paralysis and atrophy of the hand muscles and flexors of the wrist.
Brachial Plexus Block[2]
[edit | edit source]
A brachial plexus block allows a surgeon to operate on an upper extremity without the use of a general anesthetic, when combined with a tourniquet. The location of the injection is between the posterior border of the sternocleidomastoid and the clavicle. The axillary sheath surrounds the axillary vein, axillary artery, and three cords of the brachial plexus. When the injection takes effect, the muscles and skin innervated by the cords found in the sheath are anesthetized.
Other Important Information
[edit | edit source]
A useful mnemonic to remember the path of the brachial plexus is Randy (Roots) Travis (Trunks) Drinks (Divisions) Cold (Cords) Beer (Branches).
Resources
[edit | edit source]
Useful websites/ more information: Learning the Brachial Plexus, BP Video 1, BP Video 2, Brachial Plexus Block
Recent Related Research
[edit | edit source]
Saliba S, Saliba EN, Pugh KF, Chhabra A, Diduch D. Rehabilitation considerations of a brachial plexus injury with complete avulsion of C5 and C6 nerve roots in a colege football player: A Case Study. Sports Health. 2009:1(5): 370-375.
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=16U1R_35YgGiuNEE5Ycf1OMjgO66h04I-HXl5pgJbptPkJYUuz|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.