Brachial Plexus: Difference between revisions
No edit summary |
No edit summary |
||
| Line 12: | Line 12: | ||
The brachial plexus is responsible for cutaneous and muscular innervation of the entire upper limb, with two exceptions: the trapezius muscle innervated by the spinal accessory nerve (CN XI) and an area of skin near the axilla innervated by the intercostobrachial nerve. | The brachial plexus is responsible for cutaneous and muscular innervation of the entire upper limb, with two exceptions: the trapezius muscle innervated by the spinal accessory nerve (CN XI) and an area of skin near the axilla innervated by the intercostobrachial nerve. | ||
== Description<ref name="Dutton">Dutton M. Orthopaedic Examination, Evaluation and Intervention.&amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;nbsp; New York, NY: McGraw-Hill;2004.</ref><br> == | == Description<ref name="Dutton">Dutton M. Orthopaedic Examination, Evaluation and Intervention.&amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;nbsp; New York, NY: McGraw-Hill;2004.</ref><br> == | ||
=== Path === | === Path === | ||
| Line 152: | Line 152: | ||
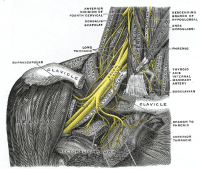
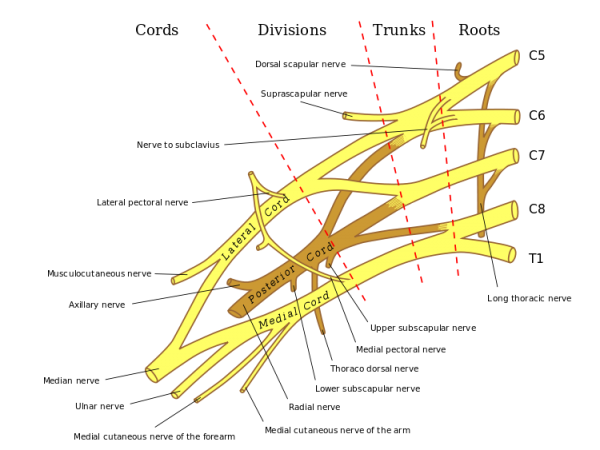
Specific branches can be visualised on the diagram below: | Specific branches can be visualised on the diagram below: | ||
[[Image:Brachplx.gif|center]]<br> | [[Image:Brachplx.gif|center]]<br> | ||
== Injuries<ref name="Dutton" /><br> == | == Injuries<ref name="Dutton" /><br> == | ||
| Line 173: | Line 173: | ||
A brachial plexus block allows a surgeon to operate on an upper extremity without the use of a general anesthetic, when combined with a tourniquet. The location of the injection is between the posterior border of the sternocleidomastoid and the clavicle. The axillary sheath surrounds the axillary vein, axillary artery, and three cords of the brachial plexus. When the injection takes effect, the muscles and skin innervated by the cords found in the sheath are anesthetized. <br> | A brachial plexus block allows a surgeon to operate on an upper extremity without the use of a general anesthetic, when combined with a tourniquet. The location of the injection is between the posterior border of the sternocleidomastoid and the clavicle. The axillary sheath surrounds the axillary vein, axillary artery, and three cords of the brachial plexus. When the injection takes effect, the muscles and skin innervated by the cords found in the sheath are anesthetized. <br> | ||
== Other | == Other Information<br> == | ||
A useful mnemonic to remember the path of the brachial plexus: | A useful mnemonic to remember the path of the brachial plexus: | ||
| Line 190: | Line 190: | ||
== Resources <br> == | == Resources <br> == | ||
== Presentations == | [http://www.jbppni.com Journal of Brachial Plexus and Peripheral Nerve Injury] | ||
== Presentations == | |||
<div class="coursebox"> | <div class="coursebox"> | ||
{| width="100%" cellspacing="4" cellpadding="4" border="0" class="FCK__ShowTableBorders" | |||
|- | |||
| align="center" | <imagemap> | |||
Image:Learn-Brachial-Plexus.png|200px|border|left| | |||
rect 0 0 220 126 [http://www.ama-assn.org/ama1/pub/upload/mm/15/brachial_plex_how_to.pdf] | |||
desc none | |||
</imagemap> | |||
| [http://www.ama-assn.org/ama1/pub/upload/mm/15/brachial_plex_how_to.pdf '''Learn the Brachial Plexus in Five Minutes or Less'''] | |||
This is a great little presentation to teach you the brachial plexus through simplified drawing. | |||
[http://www.ama-assn.org/ama1/pub/upload/mm/15/brachial_plex_how_to.pdf Have a go!] | |||
|} | |||
</div> <div class="coursebox"> | |||
{| width="100%" cellspacing="4" cellpadding="4" border="0" class="FCK__ShowTableBorders" | {| width="100%" cellspacing="4" cellpadding="4" border="0" class="FCK__ShowTableBorders" | ||
|- | |- | ||
Revision as of 11:54, 27 December 2012
Original Editor - Matt Anderson
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Introduction[edit | edit source]
The Brachial Plexus is a network of nerve fibers that run from the spine, passing through the cervico-axillary canal to reach axilla. It is formed by the ventral rami of the lower four cervical and first thoracic nerve roots (C5-C8, T1).
Function[edit | edit source]
The brachial plexus is responsible for cutaneous and muscular innervation of the entire upper limb, with two exceptions: the trapezius muscle innervated by the spinal accessory nerve (CN XI) and an area of skin near the axilla innervated by the intercostobrachial nerve.
Description[1]
[edit | edit source]
Path[edit | edit source]
The brachial plexus is divided into Roots, Trunks, Divisions, Cords, and Branches. There are five "terminal" branches and numerous other "pre-terminal" or "collateral" branches that leave the plexus at various points along its length.
- The five Roots are the five anterior rami of the of the lower four cervical and first thoracic nerve roots (C5-C8, T1), after they have given off their segmental supply to the muscles of the neck.
- These Roots merge to form three Trunks:
- Upper Trunk (C5-C6)
- Middle Trunk (C7)
- Lower Trunk (C8, T1)
- Each Trunk then splits into anterior and posterior divisions, to form six Divisions. The anterior/ posterior divisions innervate flexor groups versus extensor groups:
- anterior divisions of the upper, middle, and lower trunks
- posterior divisions of the upper, middle, and lower trunks
- These six Divisions will regroup to become the three Cords. The Cords are named by their position with respect to the axillary artery.
- The Posterior Cord is formed from the three posterior divisions of the trunks (C5-C8,T1)
- The Lateral Cord is the anterior divisions from the upper and middle trunks (C5-C7)
- The Medial Cord is simply a continuation of the anterior division of the lower trunk (C8,T1)
Specific Branches[edit | edit source]
The branches are listed below. Most branch from the cords, but a few branch (indicated in italics) directly from earlier structures.
Bold indicates primary spinal root component of nerve. Italics indicate spinal roots that frequently, but not always, contribute to the nerve.
| From | Nerve | Roots | Muscles | Cutaneous |
| roots | Dorsal scapular nerve | C4, C5 | Rhomboid muscles and Levator scapulae | - |
| roots | Long thoracic nerve | C5, C6, C7 | Serratus anterior | - |
| upper trunk | Nerve to the subclavius | C5, C6 | Subclavius muscle | - |
| upper trunk | Suprascapular nerve | C5, C6 | Supraspinatus and Infraspinatus | - |
| lateral cord | Lateral pectoral nerve | C5, C6, C7 | Pectoralis major and Pectoralis minor (by communicating with the Medial pectoral nerve) | - |
| lateral cord | Musculocutaneous nerve | C5, C6, C7 | Coracobrachialis, Brachialis and Biceps brachii | becomes the Lateral cutaneous nerve of the forearm |
| lateral cord | lateral root of the Median nerve | C6, C7 | fibres to the median nerve | - |
| posterior cord | Upper subscapular nerve | C5, C6 | Subscapularis (upper part) | - |
| posterior cord | Thoracodorsal nerve (middle subscapular nerve) | C6, C7, C8 | Latissimus dorsi | - |
| posterior cord | Lower subscapular nerve | C5, C6 | subscapularis (lower part ) and Teres major | - |
| posterior cord | Axillary nerve | C5, C6 | anterior branch: deltoid and a small area of overlying skin posterior branch: Teres minor and deltoid muscles |
posterior branch becomes Upper lateral cutaneous nerve of the arm |
| posterior cord | Radial nerve | C5, C6, C7, C8, T1 | Triceps brachii, Supinator, Anconeus, the extensor muscles of the Forearm, and Brachioradialis | skin of the posterior arm as the Posterior cutaneous nerve of the arm |
| medial cord | Medial pectoral nerve | C8, T1 | Pectoralis major and Pectoralis minor | - |
| medial cord | medial root of the Median nerve | C8, T1 | fibres to the median nerve | portions of hand not served by ulnar or radial |
| medial cord | Medial cutaneous nerve of the arm | C8, T1 | - | front and medial skin of the Arm |
| medial cord | Medial cutaneous nerve of the forearm | C8, T1 | - | medial skin of the forearm |
| medial cord | Ulnar nerve | C8, T1 | Flexor carpi ulnaris, the medial two bellies of Flexor digitorum profundus, the intrinsic hand muscles except the Thenar muscles and the two most lateral lumbricals | the skin of the medial side of the hand and medial one and a half fingers on the palmar side and medial two and a half fingers on the dorsal side |
Specific branches can be visualised on the diagram below:
Injuries[1]
[edit | edit source]
Injury to the brachial plexus can be very problematic because the nerves branching off of the plexus provide innervation to the upper extremity. Clinical signs and symptoms vary with which area of the plexus is involved, and can generally result in paralysis or anesthesia. Brachial plexus injury can occur in a variety of ways and can occur as a result of shoulder trauma, tumours, or inflammation. The rare Parsonage-Turner Syndrome causes brachial plexus inflammation without obvious injury, but with nevertheless disabling symptoms. But in general, brachial plexus lesions can be classified as either traumatic or obstetric. Obstetric injuries may occur from mechanical injury involving shoulder dystocia during difficult childbirth. During birth, excessive stretching of the neck or pulling the upper extremity can result in an upper brachial plexus injury or inferior trunk, respectively. Traumatic injury may arise from several causes including landing on the neck in a way that separates the neck from the shoulder, or from a traction injury. The severity of nerve injuries may vary from a mild stretch to the nerve root tearing away from the spinal cord (avulsion).
Brachial plexus lesions can be divided into three types:
- An upper brachial plexus lesion, which occurs from excessive lateral neck flexion away from the shoulder. Most commonly, forceps delivery or falling on the neck at an angle causes upper plexus lesions leading to Erb's Palsy. This type of injury produces a very characteristic sign called Waiter's tip deformity due to loss of the lateral rotators of the shoulder, arm flexors, and hand extensor muscles.
- Less frequently, the whole brachial plexus lesion occurs;
- Most infrequently, sudden upward pulling on an abducted arm (as when someone breaks a fall by grasping a tree branch) produces a lower brachial plexus lesion, in which the eighth cervical (C8) and first thoracic (T1) nerves are injured "either before or after they have joined to form the lower trunk. The subsequent paralysis affects, principally, the intrinsic muscles of the hand and the flexors of the wrist and fingers". This results in a form of paralysis known as Klumpke's Paralysis.
The cardinal signs of brachial plexus injury then, are weakness in the arm, diminished reflexes, and corresponding sensory deficits.
- Erb's palsy. "The position of the limb, under such conditions, is characteristic: the arm hangs by the side and is rotated medially; the forearm is extended and pronated. The arm cannot be raised from the side; all power of flexion of the elbow is lost, as is also supination of the forearm".
- In Klumpke's paralysis, a form of paralysis involving the muscles of the forearm and hand, a characteristic sign is the clawed hand, due to loss of function of the ulnar nerve and the intrinsic muscles of the hand it supplies.
Brachial Plexus Block[2]
[edit | edit source]
A brachial plexus block allows a surgeon to operate on an upper extremity without the use of a general anesthetic, when combined with a tourniquet. The location of the injection is between the posterior border of the sternocleidomastoid and the clavicle. The axillary sheath surrounds the axillary vein, axillary artery, and three cords of the brachial plexus. When the injection takes effect, the muscles and skin innervated by the cords found in the sheath are anesthetized.
Other Information
[edit | edit source]
A useful mnemonic to remember the path of the brachial plexus:
- Randy (Roots) Travis (Trunks) Drinks (Divisions) Cold (Cords) Beer (Branches).
Some mnemonics for remembering the branches:
- Posterior cord branches
- STAR - subscapular (upper and lower), thoracodorsal, axillary, radial
- ULTRA - upper subscapular, lower subscapular, thoracodorsal, radial, axillary
- Lateral Cord Branches
- LLM "Lucy Loves Me" - lateral pectoral, lateral root of the median nerve, musculocutaneous
- Medial Cord Branches
- MMMUM "Most Medical Men Use Morphine" - medial pectoral, medial cutaneous nerve of arm, medial cutaneous nerve of forearm, ulnar, medial root of the median nerve
Resources
[edit | edit source]
Journal of Brachial Plexus and Peripheral Nerve Injury
Presentations[edit | edit source]
 |
Learn the Brachial Plexus in Five Minutes or Less
This is a great little presentation to teach you the brachial plexus through simplified drawing. |
 |
Brachial Plexus Block and Translational Manipulation for Adhesive Capsulitis
Created by Tom Denninger & Ben Hando as part of the Evidence in Motion, OMPT Fellowship, 2011 |
Case Studies
[edit | edit source]
Dahlin LB, Blackman C, Duppe H, Saito H, Chemnitz A, Abul-Kasim K, Maly P. Compression of the lower trunk of the brachial plexus by a cervical rib in two adolescent girls: case reports and surgical treatment. J Brachial Plex Peripher Nerve Inj. 2009;4(14).] - FREE FULL TEXT
Saliba S, Saliba EN, Pugh KF, Chhabra A, Diduch D. Rehabilitation considerations of a brachial plexus injury with complete avulsion of C5 and C6 nerve roots in a colege football player: A Case Study. Sports Health. 2009:1(5): 370-375. - FREE FULL TEXT
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=18_r98JPP6yYzovbV2nZozjYjkI_E0zChf9qZDYnFkBWagLIqg|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.