Biopsychosocial Model
Introduction[edit | edit source]
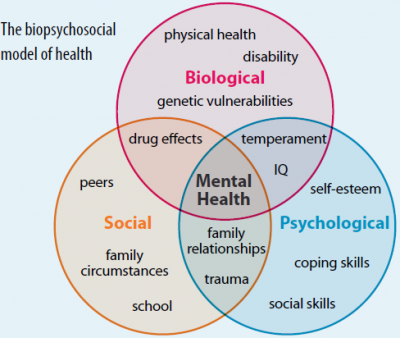
The Biopsychosocial model is a conceptual model that suggests that in understanding a person's medical condition it is not simply the biological factors to consider, but also the psychological and social factors [1].
- Bio (physiological pathology)
- Psycho (thoughts emotions and behaviours such as psychological distress, fear/avoidance beliefs, current coping methods and attribution)
- Social (socio-economical, socio-environmental, and cultural factors suchs as work issues, family circumstances and benefits/economics)
This model is commonly used in chronic pain, with the view that the pain is a psychophysiological behaviour pattern that cannot be categorised into biological, psychological, or social factors alone. There are suggestions that physiotherapy should integrate psychological treatment to address all components comprising the experience of chronic pain.
The diagram below shows an example of this model.
Diagram of the Biopsychosocial model. [2]
Physiotherapists must know how biopsychosocial factors interact in patients with chronic pain to explain the perpetuation of this condition and use it as a basis for planning the intervention program. The evidence has suggested a clinical biopsychosocial assessment for the physiotherapeutic management of patients with chronic pain in order to understand and explain the predominant mechanism of pain and psychosocial factors that may or may not be modified for the patient to improve their condition.
This clinical evaluation is carried out during the data collection at the patient's entrance. The article bla bla proposes a practical guide to take biopsychosocial data using the PSCEBSM (Pain–Somatic and medical factors–Cognitive factors–Emotional factors–Behavioral factors–Social factors–Motivation) model.
- P- Type of pain: Clinical identification and differentiation of the dominant pain type: nociceptive, neuropathic or non-neuropathic pain of central sensitization. Using using the following tools:
- Classification criteria for differentiating predominant pain proposed by Nijs et al.
- Widespread pain index/Body Diagram : ≥ 7 score suggesting generalized pain, therefore, non-neuropathic pain of central sensitization
- Central Sensitization Inventory (CSI) : 40 score suggesting non-neuropathic pain of central sensitization
- S- Somatic and medical factors: ask about current or previous health conditions, disuse of body parts, changes in movement patterns, exercise capacity, strength and muscle tone during movement, drug action in the CNS For physical therapist the physical examination is a very important part of his intervention, therefore it is essential to be aware that some findings of clinical examinations such as mobility, strength, neurodynamics, coordination, etc. could be altered because there is greater sensitivity to mechanical stimulation and modified movement patterns in patients with non-neuropathic pain of central sensitization. The main goal in this stage is to evaluate the quality of movement, if the pattern of movement causes the pain to persist and if there is kinesiofobia
- C- Cognition / Perceptions; both influence biologically on hypersensitivity in the brain by activating neuromatrix pain and also influence the emotional and behavioral factors. :
- Ask about perceptions: expectations of the intervention, expectations of the prognosis of their pain, understanding of their situation and the strategies they have available to face their situation, what the pain represents emotionally
- Brief Illness Perception Questionnaire (Brief IPQ)
- Pain Catastrophizing Scale (PCS)
- E- Emotional factors: ask if there is fear of specific movements, avoidance behaviors, psychological traumatic appearance of pain, psychological problems at work, family, finances, society, etc. It is also suggested to use the following scales:
- State-Trait Axiety Inventory (STAI)
- Tampa-Scale of Kinesiophobia (TSK)
- Injustice Experience Questionnaire (IEQ)
- Patient Health Questionnaire-2 (PHQ-2), or Patient Health Questionnaire-9 (PHQ-9), or Center of Epidemiologic Studies Depression Scale (CES-D)
- B- Behavioral Factors:
- ↑ Gatchel, Robert J., Peng, Yuan Bo, Peters, Madelon, L.; Fuchs, Perry, N.; Turk, Dennis C. 2007 The biopsychosocial approach to chronic pain: Scientific advances and future directionsfckLR Psychological Bulletin, Vol 133(4), 581-624
- ↑ http://savvywillingandable.wordpress.com/2013/09/25/the-biopsychosocial-model-explained/