Basic Foot and Ankle Anatomy - Muscles and Fascia: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Flexor digitorum longus" to "[[Flexor Digitorum Longus") |
||
| (24 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Ewa Jaraczewska]] | '''Original Editor '''- [[User:Ewa Jaraczewska|Ewa Jaraczewska]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Description == | == Description == | ||
[[Muscle Cells (Myocyte)|Muscle]]<nowiki/>s are responsible for movement and the primary cause of [[Ankle and Foot|ankle and foot]] injuries is when a movement is performed excessively, repetitively, and for a long duration that exceeds tissue capabilities.<ref name=":0">Hastings MK. Movement system syndromes of the foot and ankle. In:Sahrmann S and Associates. Movement system impairment syndromes of the extremities, cervical and thoracic spine St.Louis, MO (USA): Elsevier Mosby; 2011:p.439-482</ref> [[Weight bearing|Weight-bearing]] is a primary function of the foot and ankle - each structure has a different role in ensuring that this task can be completed. These structures must be both flexible (to adapt to ground forces) and very rigid (to propel the body forwards). They must also be able to transform quickly between these two states. Other functions include maintaining [[balance]], upright [[posture]] and recognising body position in space.<ref name=":0" /> | |||
== Lower Leg Muscle == | == Lower Leg Muscle Compartments == | ||
The lower leg muscles are divided into four compartments: the superficial posterior compartment, the deep posterior compartment, the lateral compartment, and the anterior compartment. | The lower leg muscles are divided into four compartments: the superficial posterior compartment, the deep posterior compartment, the lateral compartment, and the anterior compartment. | ||
| Line 16: | Line 17: | ||
* transforming the foot into a rigid lever | * transforming the foot into a rigid lever | ||
* assisting with push-off during the gait cycle | * assisting with push-off during the [[Gait Cycle|gait cycle]] | ||
* controlling tibia progression over the foot during initial contact through the push-off gait cycle | * controlling tibia progression over the foot during initial contact through the push-off gait cycle | ||
* controlling foot pronation during initial contact through the push-off gait cycle | * controlling foot pronation during initial contact through the push-off gait cycle | ||
==== Superficial Posterior Compartment ==== | ==== Superficial Posterior Compartment ==== | ||
''[[Soleus]]'' Origin: Soleal line, medial border of tibia, head of the fibula, posterior border of the fibula | [[File: Superficial Compartment of the Muscles of the Leg.png|alt=|thumb|442x442px|Lower Leg Muscles-Superficial Posterior Compartment]]''[[Soleus]]'' | ||
* Origin: Soleal line, medial border of [[tibia]], head of the [[fibula]], posterior border of the fibula | |||
* Insertion: Posterior surface of the [[calcaneus]] (via calcaneal tendon) | |||
* Nerve supply: [[Tibial Nerve|Tibial nerve]] (S1, S2) | |||
* Vascular supply: Posterior tibial artery and vein | |||
''[[Gastrocnemius]]'' | |||
* Origin: Two heads, lateral'':'' Posterolateral aspect of lateral condyle of the [[femur]], medial'':'' Posterior surface of the medial femoral condyle, the popliteal surface of the femoral shaft | |||
* Insertion: Posterior surface of the calcaneus via the calcaneal tendon | |||
* Nerve supply: Tibial nerve (S1, S2) | |||
* Vascular supply: Medial sural artery, a branch of the popliteal artery | |||
''[[ | ''[[Plantaris]]'' | ||
* Origin: Lateral supracondylar line of the femur, oblique popliteal ligament of the knee | |||
* Insertion: Posterior surface of the calcaneus (via calcaneal tendon) | |||
* Nerve supply: Tibial nerve (S1, S2) | |||
* Vascular supply: lateral sural and popliteal arteries and superior lateral genicular artery | |||
==== Deep Posterior Compartment ==== | ==== Deep Posterior Compartment ==== | ||
''[[Flexor | ''[[Flexor Digitorum Longus]]'' | ||
* Origin: Posterior surface of the tibia (inferior to soleal line) | |||
* Insertion: Bases of distal phalanges of digits 2-5 | |||
* Nerve supply: Tibial nerve (L5, S1, S2) | |||
* Vascular supply: Posterior tibial artery | |||
''[[ | ''[[Tibialis posterior rupture|Tibialis posterior]]'' [[File:1123 Muscles of the Leg that Move the Foot and Toes c.png|thumb|382x382px|Lower Leg Muscles-Posterior and Lateral Compartments ]] | ||
* Origin: Posterior surface of the tibia, posterior surface of fibula and interosseous membrane | |||
* Insertion: Tuberosity of navicular bone, all cuneiform bones, cuboid bone, bases of metatarsal bones 2-4 | |||
* Nerve supply: Tibial nerve (L4, L5) | |||
* Vascular supply: Branches of the posterior tibial artery | |||
''[[Flexor hallucis longus]]'' | |||
''[[ | |||
* Origin: Distal 2/3 of the posterior surface of fibula, interosseous membrane, the posterior intermuscular septum of the leg, fascia of tibialis posterior muscle | |||
* Insertion: Base of distal phalanx of the great toe | |||
* Nerve supply: Tibial nerve (S2, S3) | |||
* Vascular supply: Posterior tibial artery, fibular artery | |||
''[[Popliteus Muscle|Popliteus]]'' | |||
* Origin: Lateral condyle of femur, posterior horn of lateral meniscus of the knee joint | |||
* Insertion: Posterior surface of the proximal tibia | |||
* Nerve supply: Tibial nerve (L4-S1) | |||
* Vascular supply: Inferior medial and lateral genicular arteries (popliteal artery), posterior tibial recurrent artery, posterior tibial artery, nutrient artery of the tibia | |||
=== Lateral Compartment === | |||
[[Peroneus (Fibularis) Longus Muscle|''Peroneus (Fibularis) Longus'']] | |||
* Origin: Head and superior 2/3 of the lateral surface of the fibula | |||
* Insertion: base of the 1st metatarsal and medial cuneiform | |||
* Nerve supply: Superficial fibular nerve (L5 - S1) | |||
* Vascular supply: Fibular artery | |||
* Function: | |||
** Ankle eversion and weak plantarflexion | |||
** Muscular control of the forefoot position | |||
''[[Peroneus Brevis|Peroneus (Fibularis) Brevis]]'' | |||
* Ankle eversion and | * Origin: Inferior 2/3 of the lateral surface of the fibula | ||
* Stabilises the lateral column of the foot | * Insertion: base of the 5th metatarsal | ||
* Nerve supply: superficial fibular nerve (L5 - S1) | |||
* Vascular supply: Anterior tibial artery | |||
* Function: | |||
** Ankle eversion and weak plantarflexion | |||
** Stabilises the lateral column of the foot | |||
=== Anterior Compartment === | === Anterior Compartment === | ||
| Line 60: | Line 101: | ||
* concentric control of toes clearance during swing phase | * concentric control of toes clearance during swing phase | ||
''[[Tibialis Anterior]]''[[File: Anterior compartment.png|thumb|432x432px|Lower Leg Muscles- Anterior Compartment]] | |||
* Origin: upper two-thirds of the lateral (outside) surface of the tibia | |||
* Insertion: medial cuneiform and first metatarsal bones of the foot | |||
* Nerve supply: Deep fibular nerve (L4, L5), and a branch of common fibular nerve | |||
* Vascular supply: Anterior tibial artery | |||
''[[Extensor Digitorum Longus|Extensor Digitorum Longus]]'' | |||
* Origin: Proximal 1/2 of the medial surface of fibula, lateral tibial condyle, interosseous membrane | |||
* Insertion: Distal and middle phalanges of digits 2-5 | |||
* Nerve supply: Deep fibular nerve (L5, S1) | |||
* Vascular supply: Anterior tibial, fibular, anterior lateral malleolar, lateral tarsal, metatarsal, plantar, and digital arteries | |||
''Extensor | ''[[Extensor Hallucis Longus]]'' | ||
* Origin: Middle 1/3 of the medial surface of fibula, interosseous membrane | |||
* Insertion: Base of distal phalanx of the great toe | |||
* Nerve supply: Deep fibular nerve (L5, S1) | |||
* Vascular supply: Anterior tibial artery | |||
[[Peroneus Tertius|''Peroneus (Fibularis) Tertius'']] | |||
* Origin: Distal 1/3 of the medial surface of fibula, interosseous membrane (anterior surface), anterior intermuscular septum | |||
* Insertion: Dorsal surface of base of the 5th metatarsal bone | |||
* Nerve supply: Deep fibular nerve (L5, S1) | |||
* Vascular supply: Anterior lateral malleolar artery, lateral tarsal artery, metatarsal arteries, lateral plantar artery, digital arteries, arcuate artery, fourth dorsal metatarsal artery | |||
== Foot Muscles == | == Foot Muscles == | ||
Stabilisation of the arches, metatarsophalangeal (MTP) and interphalangeal (IP) joints are the main functions of the intrinsic muscles of the foot. In addition these muscles :[[File: Intrinsic foot muscles.png|thumb|Foot Muscles]] | |||
* assist with tension regulation and counteract extrinsic muscle force production | * assist with tension regulation and counteract extrinsic muscle force production | ||
* provide critical stabilisation of the foot allowing its transition from rigid to flexible during the gait cycle | * provide critical stabilisation of the foot allowing its transition from rigid to flexible during the gait cycle | ||
* quadratus plantae helps with | * quadratus plantae helps with toe flexion in the sagittal plane | ||
* lumbricals extend the interphalangeal joint | * lumbricals extend the interphalangeal joint | ||
* interosseus assist with the MTP joint flexion, IP joint extension, | * interosseus assist with the MTP joint flexion, IP joint extension, toe abduction and adduction | ||
* | * | ||
''[[Quadratus Plantae]]'' Origin: | ''[[Quadratus Plantae]]'' | ||
* Origin: Calcaneus | |||
* Insertion: tendon of the flexor digitorum longus | |||
* Nerve supply: Lateral plantar nerve (S1-S3) | |||
* Vascular supply: branch of the posterior tibial artery | |||
''Lumbricals'' | |||
* Origin: Tendon of the flexor digitorum longus | |||
* Insertion: Medial proximal phalanx and dorsal expansion of the extensor digitorum longus | |||
* Nerve supply: Lumbrical 1: Medial plantar nerve (S2, S3); Lumbricals 2-4: Lateral plantar nerve (S2-S3) | |||
* Vascular supply: Lateral plantar artery, plantar metatarsal arteries, dorsal metatarsal arteries, dorsal digital arteries | |||
''Interossei'' | |||
* Origin: Shafts of the metatarsals | |||
* Insertion: Base of the proximal phalanx | |||
* Nerve supply: Lateral plantar nerve (S2-S3) | |||
* Vascular supply: Lateral plantar artery | |||
{{#ev:youtube|v=dg4QDyZmFoc&t=57s|300}}<ref>Taim Talks Med. Muscles of the Foot (Groups, Origin, Insertion, Function). Available from: https://www.youtube.com/watch?v=dg4QDyZmFoc&t=57s[last accessed 10/01/2022]</ref> | |||
[ | |||
== Fascia == | == Fascia == | ||
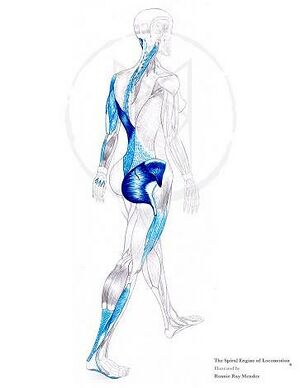
Fascia connects mechanically with the underlying muscles. The clinical | [[File: Myofascial chains.jpg|thumb|Myofascial chains]][[Fascia]] connects mechanically with the underlying muscles. The muscles' insertion into the [[Myofascial Pain|myofascia]] supports the clinical observation that the fascia and muscles influence each other. The connection between the extensor hallucis longus muscle, the anterior crural compartment and the muscles located in the peroneal compartment that connects with the lateral collateral ligament is an example of when myofascial connections have a direct and indirect effect on muscle function and proprioception.<ref name=":4" /> | ||
The myofascial chain is a concept that explains how the mechanical forces transfer between the muscles of one limb and the muscles in series. The available studies of the muscle-fascia lines indicate, for example, a force transmission across the posterior myofascial chain (PL) that includes the plantar aponeurosis, gastrocnemius muscle and fascia hamstring muscles and fasciae, sacrotuberous ligament, and lumbar fascia and erector spinae muscle.<ref name=":4" /> | |||
Another function of the fascia is blood flow regulation. In the lower leg, proper vascular supply partially depends on the pressure created by the fascia compartments. Fascial restrictions can cause blood vessel entrapment, leading to oedema, cramping, and claudication.<ref>Boser A, Schumaker K. Fascia and the Circulatory System. In: Fascia, Function, and Medical Applications 2020 Aug 20 (pp. 71-84). CRC Press.</ref> | |||
==== Lower Leg Fascia ==== | ==== Lower Leg Fascia ==== | ||
The Lateral Line of | The Lateral Line of fascia (LL) connects the lateral and the medial side of the foot with the lateral side of the body.<ref name=":3">Thomas V. Myers. The Lateral Line. In: Thomas V. Myers, editor. Anatomy Trains. Edinburgh: Churchill Livingstone, Elsevier 2009. 2nd ed. p.115-118.</ref> It begins on the medial side of the foot with the insertion of the peroneus longus, travels under the foot towards its lateral aspect and is joined by the peroneus brevis tendon. It then moves up towards the lateral malleolus, where peroneus longus and peroneus brevis are the only muscles within the lateral compartment of the lower leg. The complete LL myofascial tracks are as follow: | ||
Splenius capitis/sternocleidomastoid→external/internal intercostals→lateral abdominal obliques→Gluteus maximus/Tensor Fasciae Latae/Iliotibial track→Anterior ligament of head of fibula→Peroneal(Fibularis) muscles/lateral crural compartment.<ref name=":3" /> | Splenius capitis/sternocleidomastoid→external/internal intercostals→lateral abdominal obliques→Gluteus maximus/Tensor Fasciae Latae/Iliotibial track→Anterior ligament of head of fibula→Peroneal(Fibularis) muscles/lateral crural compartment.<ref name=":3" /> | ||
[ | {{#ev:youtube|v=nuxTfQ15qOc&t=229s|300}}<ref>Lateral Line - Fascial Planes - Ask Dr. Abelson. 2014. Available from: https://www.youtube.com/watch?v=nuxTfQ15qOc&t=229s [last accessed 10/01/2022]</ref> | ||
Tensor Fascia Latae is a fascial continuation of the LL that divides the lower leg muscles into four compartments.<ref>Peabody T, Bordoni B. [https://www.ncbi.nlm.nih.gov/books/NBK557497/ Anatomy, Bony Pelvis and Lower Limb, Fascia Lata]. StatPearls [Internet]. 2021 Feb 7.</ref> Their primary roles are: | |||
* assisting the muscle with transferring the power from the muscle to the bone | * assisting the muscle with transferring the power from the muscle to the bone | ||
* creating spatial restriction for oedema | * creating spatial restriction for oedema | ||
* | * affecting nerve and blood vessel function within the compartment in case of oedema. | ||
==== Foot Fascia ==== | ==== Foot Fascia ==== | ||
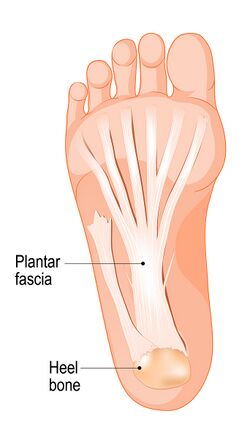
The fascia of the foot can be defined by the superficial and deep fascia, each having different strengths and thicknesses. Its primary function is to support, divide and attach muscles.<ref name=":1">Bourne M, Talkad A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb, Foot Fascia. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2021. </ref> In addition it: | [[File: Adapted Bigstock Image -Plantar aponeurosis -ID 309750076.jpg|thumb|433x433px|Foot Fascia]]The fascia of the foot can be defined by the superficial and deep fascia, each having different strengths and thicknesses. Its primary function is to support, divide and attach muscles.<ref name=":1">Bourne M, Talkad A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb, Foot Fascia. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2021. </ref> In addition it: | ||
* optimises the static and dynamic function of the foot | * optimises the static and dynamic function of the foot | ||
* influences the shape of the muscles | * influences the shape of the muscles | ||
* optimises movement and function of the regional nerves and blood vessels | * optimises movement and function of the regional nerves and blood vessels | ||
* supports foot arches. Partial and total plantar fascia release may decrease the arch height <ref>Cheung JT, An KN, Zhang M. Consequences of partial and total plantar fascia release: a finite element study. Foot Ankle Int. 2006 Feb;27(2):125-32. </ref> | * supports foot arches. Partial and total plantar fascia release may decrease the arch height <ref>Cheung JT, An KN, Zhang M. Consequences of partial and total plantar fascia release: a finite element study. Foot Ankle Int. 2006 Feb;27(2):125-32. </ref> | ||
* is a functional windlass | * is a functional windlass | ||
* provides the shock-absorbing characteristics to allow for pedal movement<ref name=":1" /> | * provides the shock-absorbing characteristics to allow for pedal movement<ref name=":1" /> | ||
The fascia specifies five anatomic compartments of the foot: medial, central, lateral, dorsal, and interosseous compartments. The plantar fascia appears to be the major contributor to static foot posture. | The fascia specifies five anatomic compartments of the foot: medial, central, lateral, dorsal, and interosseous compartments. The plantar fascia appears to be the major contributor to static foot posture. | ||
''[[Plantar Aponeurosis|Plantar fascia]]'' Origin: calcaneus | ''[[Plantar Aponeurosis|Plantar fascia]]'' | ||
* Origin: calcaneus | |||
* Insertion: phalanges | |||
* Nerve supply: lateral and medial plantar nerves | |||
* Vascular supply: branch of the dorsalis pedis artery and the posterior tibial artery<blockquote>The lateral band of the plantar fascia belongs to the Superficial Back Line. However, the fascia Lateral Line through the metatarsal complex and its connections with the fibula provides support for the [[Arches of the Foot|lateral longitudinal arch]].<ref name=":3" /> </blockquote> | |||
===== Windlass Mechanism ===== | ===== Windlass Mechanism ===== | ||
Windlass mechanism (tightening of a cable) describes plantar fascia role in weight-bearing activities by providing dynamic support to the foot. You can read more about this mechanism and how to test it [[Windlass Test|here]]. | The [[Windlass Test|Windlass mechanism]] (tightening of a cable) describes the plantar fascia's role in weight-bearing activities by providing dynamic support to the foot. You can read more about this mechanism and how to test it [[Windlass Test|here]]. | ||
== Arches == | == Arches == | ||
There is one continuous arch in the foot that runs anterior to posterior and medial to lateral, but the literature usually describes three arches of the foot: medial, lateral and transverse arch.<ref name=":0" /> | There is one continuous [[Arches of the Foot|arch]] in the foot that runs anterior to posterior and medial to lateral, but the literature usually describes three arches of the foot: the medial, lateral and transverse arch.<ref name=":0" /> The medial and lateral arches constitute the longitudinal arch. All arches act as rigid and flexible structures needed for normal walking.<ref name=":2">Gwani AS, Asari MA, Mohd Ismail ZI. [https://journals.viamedica.pl/folia_morphologica/article/view/FM.a2017.0049/38549 How the three arches of the foot intercorrelate.] Folia Morphol (Warsz). 2017;76(4):682-688. </ref> In addition: | ||
* the arches provide a stable base for standing posture | |||
* the lateral arch plays a role in providing support during frontal plane body weight shift with locomotion | |||
* | * the height of the medial arch defines pes planus or pes cavus | ||
* lateral arch plays role in providing support during frontal plane body weight shift | * the transverse arch is necessary for the medial and lateral arches' stability. | ||
* the height of the medial arch defines pes | |||
* the transverse arch is necessary for medial and lateral arches stability. | |||
The arches are formed by the following bones: | The arches are formed by the following bones: | ||
''The medial arch'': calcaneus, talus, navicular, three cuneiforms, first three metatarsals | * ''The medial arch'': | ||
** calcaneus, talus, navicular, three cuneiforms, first three metatarsals | |||
''The lateral arch'': calcaneus, cuboid, lateral two metatarsals | * ''The lateral arch'': | ||
** calcaneus, cuboid, lateral two metatarsals | |||
''The transverse arch'': three cuneiforms, cuboid, bases of five metatarsals.<ref name=":2" /> | * ''The transverse arch'': | ||
** three cuneiforms, cuboid, bases of five metatarsals.<ref name=":2" /> | |||
All arches receive ligamentous support via plantar ligaments and plantar aponeurosis. | All arches receive ligamentous support via plantar ligaments and plantar aponeurosis. | ||
== Clinical | == Clinical Relevance == | ||
# The area posterior to the medial malleolus tends to get injured frequently causing tendon injury of the posterior tibialis, flexor hallucis longus or flexor digitorum and tibial nerve compression.<ref name=":0" /> | # The area posterior to the medial malleolus tends to get injured frequently causing tendon injury of the posterior tibialis, flexor hallucis longus or flexor digitorum and tibial nerve compression.<ref name=":0" /> | ||
# The transtarsal joint achieves its stability through bony shape, ligament tightness and extrinsic muscles crossing the foot as there are no intrinsic muscles attaching to talus or | # The transtarsal joint achieves its stability through the bony shape, ligament tightness and extrinsic muscles crossing the foot as there are no intrinsic muscles attaching to the talus or calcaneus and inserting to the cuboid or navicular bones. This may be the cause of this joint's frequent hypermobility.<ref name=":0" /> | ||
# Hammer and claw toe deformities can be prevented with strong action of the interossei and lumbricals. | # Hammer and claw toe deformities can be prevented with strong action of the interossei and lumbricals. | ||
# Increased tissue stiffness in gastrocnemius and hamstrings muscles can lead to [[Plantar Fasciitis|plantar fasciitis]], and calf muscle stretching can be the solution for the problem.<ref name=":4">Wilke J, Schleip R, Yucesoy CA, Banzer W. [https://journals.physiology.org/doi/full/10.1152/japplphysiol.00565.2017 Not merely a protective packing organ? A review of fascia and its force transmission capacity]. Journal of Applied Physiology. 2018 Jan 1;124(1):234-44.</ref> | # Increased tissue stiffness in gastrocnemius and hamstrings muscles can lead to [[Plantar Fasciitis|plantar fasciitis]], and calf muscle stretching can be the solution for the problem.<ref name=":4">Wilke J, Schleip R, Yucesoy CA, Banzer W. [https://journals.physiology.org/doi/full/10.1152/japplphysiol.00565.2017 Not merely a protective packing organ? A review of fascia and its force transmission capacity]. Journal of Applied Physiology. 2018 Jan 1;124(1):234-44.</ref> | ||
# Acute or chronic tears in the plantar fascia can be diagnosed by palpation of the painful lump on the sole of the foot.<ref name=":1" /> | # Acute or chronic tears in the plantar fascia can be diagnosed by palpation of the painful lump on the sole of the foot.<ref name=":1" /> | ||
== | == References == | ||
<references /> | <references /> | ||
[[Category:Anatomy]] [[Category:Muscles]] | [[Category:Anatomy]] [[Category:Muscles]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Foot - Anatomy]] | [[Category:Foot - Anatomy]] | ||
[[Category:Ankle - Anatomy]] | [[Category:Ankle - Anatomy]] | ||
[[Category: | [[Category:Plus Content]] | ||
Latest revision as of 12:20, 16 April 2024
Original Editor - Ewa Jaraczewska
Top Contributors - Ewa Jaraczewska, Wanda van Niekerk, Kim Jackson, Jess Bell, Tarina van der Stockt, Lucinda hampton and Olajumoke Ogunleye
Description[edit | edit source]
Muscles are responsible for movement and the primary cause of ankle and foot injuries is when a movement is performed excessively, repetitively, and for a long duration that exceeds tissue capabilities.[1] Weight-bearing is a primary function of the foot and ankle - each structure has a different role in ensuring that this task can be completed. These structures must be both flexible (to adapt to ground forces) and very rigid (to propel the body forwards). They must also be able to transform quickly between these two states. Other functions include maintaining balance, upright posture and recognising body position in space.[1]
Lower Leg Muscle Compartments[edit | edit source]
The lower leg muscles are divided into four compartments: the superficial posterior compartment, the deep posterior compartment, the lateral compartment, and the anterior compartment.
Posterior Compartments[edit | edit source]
The primary plantar flexors of the ankle are located in this compartment. Because of its insertion medial to the midline of the foot, they also function as supinators.
Primary responsibilities include:
- transforming the foot into a rigid lever
- assisting with push-off during the gait cycle
- controlling tibia progression over the foot during initial contact through the push-off gait cycle
- controlling foot pronation during initial contact through the push-off gait cycle
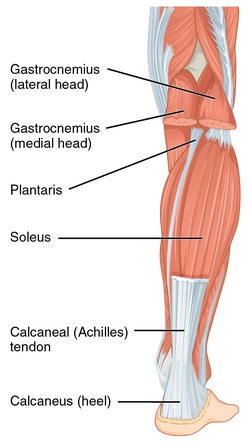
Superficial Posterior Compartment[edit | edit source]
- Origin: Soleal line, medial border of tibia, head of the fibula, posterior border of the fibula
- Insertion: Posterior surface of the calcaneus (via calcaneal tendon)
- Nerve supply: Tibial nerve (S1, S2)
- Vascular supply: Posterior tibial artery and vein
- Origin: Two heads, lateral: Posterolateral aspect of lateral condyle of the femur, medial: Posterior surface of the medial femoral condyle, the popliteal surface of the femoral shaft
- Insertion: Posterior surface of the calcaneus via the calcaneal tendon
- Nerve supply: Tibial nerve (S1, S2)
- Vascular supply: Medial sural artery, a branch of the popliteal artery
- Origin: Lateral supracondylar line of the femur, oblique popliteal ligament of the knee
- Insertion: Posterior surface of the calcaneus (via calcaneal tendon)
- Nerve supply: Tibial nerve (S1, S2)
- Vascular supply: lateral sural and popliteal arteries and superior lateral genicular artery
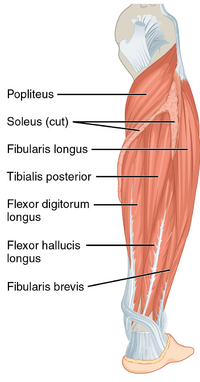
Deep Posterior Compartment[edit | edit source]
- Origin: Posterior surface of the tibia (inferior to soleal line)
- Insertion: Bases of distal phalanges of digits 2-5
- Nerve supply: Tibial nerve (L5, S1, S2)
- Vascular supply: Posterior tibial artery
- Origin: Posterior surface of the tibia, posterior surface of fibula and interosseous membrane
- Insertion: Tuberosity of navicular bone, all cuneiform bones, cuboid bone, bases of metatarsal bones 2-4
- Nerve supply: Tibial nerve (L4, L5)
- Vascular supply: Branches of the posterior tibial artery
- Origin: Distal 2/3 of the posterior surface of fibula, interosseous membrane, the posterior intermuscular septum of the leg, fascia of tibialis posterior muscle
- Insertion: Base of distal phalanx of the great toe
- Nerve supply: Tibial nerve (S2, S3)
- Vascular supply: Posterior tibial artery, fibular artery
- Origin: Lateral condyle of femur, posterior horn of lateral meniscus of the knee joint
- Insertion: Posterior surface of the proximal tibia
- Nerve supply: Tibial nerve (L4-S1)
- Vascular supply: Inferior medial and lateral genicular arteries (popliteal artery), posterior tibial recurrent artery, posterior tibial artery, nutrient artery of the tibia
Lateral Compartment[edit | edit source]
- Origin: Head and superior 2/3 of the lateral surface of the fibula
- Insertion: base of the 1st metatarsal and medial cuneiform
- Nerve supply: Superficial fibular nerve (L5 - S1)
- Vascular supply: Fibular artery
- Function:
- Ankle eversion and weak plantarflexion
- Muscular control of the forefoot position
- Origin: Inferior 2/3 of the lateral surface of the fibula
- Insertion: base of the 5th metatarsal
- Nerve supply: superficial fibular nerve (L5 - S1)
- Vascular supply: Anterior tibial artery
- Function:
- Ankle eversion and weak plantarflexion
- Stabilises the lateral column of the foot
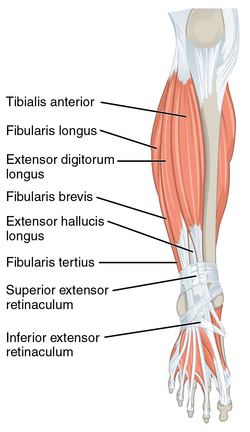
Anterior Compartment[edit | edit source]
Ankle dorsiflexion is performed by all the muscles within the anterior compartment. In addition
- tibialis anterior and extensor hallucis longus invert the foot during dorsiflexion
- extensor digitorum longus everts the foot during dorsiflexion
- eccentric control of foot lowering during heel strike
- concentric control of toes clearance during swing phase
- Origin: upper two-thirds of the lateral (outside) surface of the tibia
- Insertion: medial cuneiform and first metatarsal bones of the foot
- Nerve supply: Deep fibular nerve (L4, L5), and a branch of common fibular nerve
- Vascular supply: Anterior tibial artery
- Origin: Proximal 1/2 of the medial surface of fibula, lateral tibial condyle, interosseous membrane
- Insertion: Distal and middle phalanges of digits 2-5
- Nerve supply: Deep fibular nerve (L5, S1)
- Vascular supply: Anterior tibial, fibular, anterior lateral malleolar, lateral tarsal, metatarsal, plantar, and digital arteries
- Origin: Middle 1/3 of the medial surface of fibula, interosseous membrane
- Insertion: Base of distal phalanx of the great toe
- Nerve supply: Deep fibular nerve (L5, S1)
- Vascular supply: Anterior tibial artery
- Origin: Distal 1/3 of the medial surface of fibula, interosseous membrane (anterior surface), anterior intermuscular septum
- Insertion: Dorsal surface of base of the 5th metatarsal bone
- Nerve supply: Deep fibular nerve (L5, S1)
- Vascular supply: Anterior lateral malleolar artery, lateral tarsal artery, metatarsal arteries, lateral plantar artery, digital arteries, arcuate artery, fourth dorsal metatarsal artery
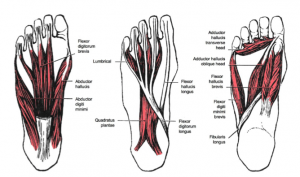
Foot Muscles[edit | edit source]
Stabilisation of the arches, metatarsophalangeal (MTP) and interphalangeal (IP) joints are the main functions of the intrinsic muscles of the foot. In addition these muscles :
- assist with tension regulation and counteract extrinsic muscle force production
- provide critical stabilisation of the foot allowing its transition from rigid to flexible during the gait cycle
- quadratus plantae helps with toe flexion in the sagittal plane
- lumbricals extend the interphalangeal joint
- interosseus assist with the MTP joint flexion, IP joint extension, toe abduction and adduction
- Origin: Calcaneus
- Insertion: tendon of the flexor digitorum longus
- Nerve supply: Lateral plantar nerve (S1-S3)
- Vascular supply: branch of the posterior tibial artery
Lumbricals
- Origin: Tendon of the flexor digitorum longus
- Insertion: Medial proximal phalanx and dorsal expansion of the extensor digitorum longus
- Nerve supply: Lumbrical 1: Medial plantar nerve (S2, S3); Lumbricals 2-4: Lateral plantar nerve (S2-S3)
- Vascular supply: Lateral plantar artery, plantar metatarsal arteries, dorsal metatarsal arteries, dorsal digital arteries
Interossei
- Origin: Shafts of the metatarsals
- Insertion: Base of the proximal phalanx
- Nerve supply: Lateral plantar nerve (S2-S3)
- Vascular supply: Lateral plantar artery
Fascia[edit | edit source]
Fascia connects mechanically with the underlying muscles. The muscles' insertion into the myofascia supports the clinical observation that the fascia and muscles influence each other. The connection between the extensor hallucis longus muscle, the anterior crural compartment and the muscles located in the peroneal compartment that connects with the lateral collateral ligament is an example of when myofascial connections have a direct and indirect effect on muscle function and proprioception.[3]
The myofascial chain is a concept that explains how the mechanical forces transfer between the muscles of one limb and the muscles in series. The available studies of the muscle-fascia lines indicate, for example, a force transmission across the posterior myofascial chain (PL) that includes the plantar aponeurosis, gastrocnemius muscle and fascia hamstring muscles and fasciae, sacrotuberous ligament, and lumbar fascia and erector spinae muscle.[3]
Another function of the fascia is blood flow regulation. In the lower leg, proper vascular supply partially depends on the pressure created by the fascia compartments. Fascial restrictions can cause blood vessel entrapment, leading to oedema, cramping, and claudication.[4]
Lower Leg Fascia[edit | edit source]
The Lateral Line of fascia (LL) connects the lateral and the medial side of the foot with the lateral side of the body.[5] It begins on the medial side of the foot with the insertion of the peroneus longus, travels under the foot towards its lateral aspect and is joined by the peroneus brevis tendon. It then moves up towards the lateral malleolus, where peroneus longus and peroneus brevis are the only muscles within the lateral compartment of the lower leg. The complete LL myofascial tracks are as follow:
Splenius capitis/sternocleidomastoid→external/internal intercostals→lateral abdominal obliques→Gluteus maximus/Tensor Fasciae Latae/Iliotibial track→Anterior ligament of head of fibula→Peroneal(Fibularis) muscles/lateral crural compartment.[5]
Tensor Fascia Latae is a fascial continuation of the LL that divides the lower leg muscles into four compartments.[7] Their primary roles are:
- assisting the muscle with transferring the power from the muscle to the bone
- creating spatial restriction for oedema
- affecting nerve and blood vessel function within the compartment in case of oedema.
Foot Fascia[edit | edit source]
The fascia of the foot can be defined by the superficial and deep fascia, each having different strengths and thicknesses. Its primary function is to support, divide and attach muscles.[8] In addition it:
- optimises the static and dynamic function of the foot
- influences the shape of the muscles
- optimises movement and function of the regional nerves and blood vessels
- supports foot arches. Partial and total plantar fascia release may decrease the arch height [9]
- is a functional windlass
- provides the shock-absorbing characteristics to allow for pedal movement[8]
The fascia specifies five anatomic compartments of the foot: medial, central, lateral, dorsal, and interosseous compartments. The plantar fascia appears to be the major contributor to static foot posture.
- Origin: calcaneus
- Insertion: phalanges
- Nerve supply: lateral and medial plantar nerves
- Vascular supply: branch of the dorsalis pedis artery and the posterior tibial artery
The lateral band of the plantar fascia belongs to the Superficial Back Line. However, the fascia Lateral Line through the metatarsal complex and its connections with the fibula provides support for the lateral longitudinal arch.[5]
Windlass Mechanism[edit | edit source]
The Windlass mechanism (tightening of a cable) describes the plantar fascia's role in weight-bearing activities by providing dynamic support to the foot. You can read more about this mechanism and how to test it here.
Arches[edit | edit source]
There is one continuous arch in the foot that runs anterior to posterior and medial to lateral, but the literature usually describes three arches of the foot: the medial, lateral and transverse arch.[1] The medial and lateral arches constitute the longitudinal arch. All arches act as rigid and flexible structures needed for normal walking.[10] In addition:
- the arches provide a stable base for standing posture
- the lateral arch plays a role in providing support during frontal plane body weight shift with locomotion
- the height of the medial arch defines pes planus or pes cavus
- the transverse arch is necessary for the medial and lateral arches' stability.
The arches are formed by the following bones:
- The medial arch:
- calcaneus, talus, navicular, three cuneiforms, first three metatarsals
- The lateral arch:
- calcaneus, cuboid, lateral two metatarsals
- The transverse arch:
- three cuneiforms, cuboid, bases of five metatarsals.[10]
All arches receive ligamentous support via plantar ligaments and plantar aponeurosis.
Clinical Relevance[edit | edit source]
- The area posterior to the medial malleolus tends to get injured frequently causing tendon injury of the posterior tibialis, flexor hallucis longus or flexor digitorum and tibial nerve compression.[1]
- The transtarsal joint achieves its stability through the bony shape, ligament tightness and extrinsic muscles crossing the foot as there are no intrinsic muscles attaching to the talus or calcaneus and inserting to the cuboid or navicular bones. This may be the cause of this joint's frequent hypermobility.[1]
- Hammer and claw toe deformities can be prevented with strong action of the interossei and lumbricals.
- Increased tissue stiffness in gastrocnemius and hamstrings muscles can lead to plantar fasciitis, and calf muscle stretching can be the solution for the problem.[3]
- Acute or chronic tears in the plantar fascia can be diagnosed by palpation of the painful lump on the sole of the foot.[8]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Hastings MK. Movement system syndromes of the foot and ankle. In:Sahrmann S and Associates. Movement system impairment syndromes of the extremities, cervical and thoracic spine St.Louis, MO (USA): Elsevier Mosby; 2011:p.439-482
- ↑ Taim Talks Med. Muscles of the Foot (Groups, Origin, Insertion, Function). Available from: https://www.youtube.com/watch?v=dg4QDyZmFoc&t=57s[last accessed 10/01/2022]
- ↑ 3.0 3.1 3.2 Wilke J, Schleip R, Yucesoy CA, Banzer W. Not merely a protective packing organ? A review of fascia and its force transmission capacity. Journal of Applied Physiology. 2018 Jan 1;124(1):234-44.
- ↑ Boser A, Schumaker K. Fascia and the Circulatory System. In: Fascia, Function, and Medical Applications 2020 Aug 20 (pp. 71-84). CRC Press.
- ↑ 5.0 5.1 5.2 Thomas V. Myers. The Lateral Line. In: Thomas V. Myers, editor. Anatomy Trains. Edinburgh: Churchill Livingstone, Elsevier 2009. 2nd ed. p.115-118.
- ↑ Lateral Line - Fascial Planes - Ask Dr. Abelson. 2014. Available from: https://www.youtube.com/watch?v=nuxTfQ15qOc&t=229s [last accessed 10/01/2022]
- ↑ Peabody T, Bordoni B. Anatomy, Bony Pelvis and Lower Limb, Fascia Lata. StatPearls [Internet]. 2021 Feb 7.
- ↑ 8.0 8.1 8.2 Bourne M, Talkad A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb, Foot Fascia. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2021.
- ↑ Cheung JT, An KN, Zhang M. Consequences of partial and total plantar fascia release: a finite element study. Foot Ankle Int. 2006 Feb;27(2):125-32.
- ↑ 10.0 10.1 Gwani AS, Asari MA, Mohd Ismail ZI. How the three arches of the foot intercorrelate. Folia Morphol (Warsz). 2017;76(4):682-688.