Baastrup Syndrome
Original Editors - Sofie Bourdinon
Top Contributors - Sofie Bourdinon, Scott Cornish, Nikki Rommers, Admin, Arno Vrambout, Kim Jackson, Fien Selderslaghs, Lucinda hampton, Uchechukwu Chukwuemeka, Vidya Acharya, Ceulemans Lisa, Aarti Sareen, WikiSysop and 127.0.0.1
Search Strategy[edit | edit source]
Search engines: Pubmed, Web of knowledge. Google Scholar and Google Books are practical too.
Keywords: Baastrup syndrome, Baastrup AND etiology, Baastrup disease, kissing spines, Baastrup’s sign, Baastrup syndrome AND physical therapy, Baastrup syndrome AND exercise, Kissing spines AND conservative therapy, Baastrup disease AND surgical management, hyperlordosis AND physical therapy.
Definition/Description[edit | edit source]
Baastrup Syndrome is named after Christian Ingerslev Baastrup, a Danish radiologist (1855-1950). It is also known as ‘kissing spines’. Kissing spines is a common disorder of the vertebral column. It is characterized by close approximation and contact of the spinous processes of two neighboring vertebrae. This can result in the formation of a new joint between them. This possibly causes mechanical back pain. The hypertrophied spinous processes of adjoining lumbar vertebrae in close approximation or in actual contact may undergo reactive sclerosis or degeneration. This is mostly observed in the lumbar segment, but has also been reported to occur in the cervical spine in some cases.[1, Book][2, level 4][3, level 4]
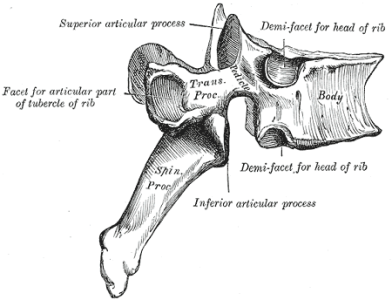
Clinically Relevant Anatomy[edit | edit source]
The spinous processes of the lumbar spine are orientated dorsally and caudally. All of the muscles that are involved in spinal movement and stabilization are only attached to the posterior elements of the spine. Therefore the spinous processes are subjected to major forces with movement or stabilization of the spine.[4, level 2B]
Abnormal downward pointing and thickening of spinous process
The interspinous ligament arches between two adjoining superior and inferior spinous processes. Anteriorly, it is continuous with the ligamentum flavum, and posteriorly, it fuses with the supraspinous ligament. The external layer of the interspinous ligament contains fibers of the aponeuroses of the M. longissimus, which contributes to the stability at that level. The interspinous ligament functions primarily to prevent excessive spinal flexion by limiting separation of two adjacent spinous processes. It has also been suggested that the interspinous ligament helps control vertebral rotation during flexion helping the facet joints remain in contact while gliding.[4, level 2B]
The supraspinous ligament is attached to the posterior tips of the spinous processes from approximately C7 to L4-L5. It limits spinal flexion and resists separation of two neighboring spinous processes.
The posterior part of the interspinous and supraspinous ligaments is sensory innervated. The role of this input is to give proprioceptive information and protect against excessive forces.[4, level 2]
Epidemiology /Etiology[edit | edit source]
The exact etiology of Baastrup’s sign is unknown. The hypothesis is that an excessive lordosis or extensive loss of intervertebral space is linked to degeneration of the vertebral disc. This can lead to contact between the spinous processes and to degeneration of other ligaments.
Other possible causes of kissing spines are: incorrect posture, traumatic injuries, excessive lordosis due to scoliosis and kyphoscoliosis, spondylolysthesis, tuberculous spondylitis, bilateral forms of congenital hip dislocation and obesity. Also, increased spinous process dimensions has been linked to several rare disorders.[1, Book][2, level 4]
It can also happen when the thoracic spine or the thoracolumbar transition stiffens[5Book].
Baastrup syndrome can occur independently or symptom of other disorders.[6Book] There is controversy regarding the etiology of pain in this condition. The cause of pain has been described to be mainly mechanical because of the neighboring spinous processes coming into contact. Pain worsens with hyperextension or increased lordosis which can been seen in patients with obesity, limitation of hip movements and champion swimmers.[1Book][7, level 2C]
The epidemiology of Baastrup syndrome in the general population is unknown. It seems to be high according to the relatively frequent abnormal changes of the interspinous spaces and spinous
processes seen at autopsy.[2, level 4]
Characteristics/Clinical Presentation[edit | edit source]
The patient will report localized interspinous or spinous process pain with or without a referral pattern [7, level 2C][8, level 2C][9, Book]. The role of Baastrup’s disease as a substantial nociceptor is controversial. Surgical excision of the involved spinous processes has not been proven to be effective in pain relief[8, level 2C]. However, Tthere are also many other possible causes of pain generators in the lower back region[8, level 2C][9, Book]. Extension is the most painful lumbar movement due to contact between the spinous processes, which causes irritation of the interspinal ligament [10, Book][5Book]. When the rotation and lateral flexion is examined, it will be painful. Flexion is the least painful of all lumbar movements[10, Book].
Baastrup’s disease can result in intraspinal cysts secondary to interspinous bursitis that may rarely which can cause symptomatic spinal stenosis and neurogenic claudation[1, level Book].
In one study using MRI for diagnosis, lumbar interspinous bursitis was present in 8,2% of patients with low back pain [7, level 2C]. In one study using CT scans of the general population, Baastrup’s disease was found in 41% of the population[8, level2C].
Baastrup’s disease is age related with an increasing occurrence in later stages of life[7, level2C][8, level2C]. L4-L5 is the most commonly affected region of the lumbar spine[8, level2C].
Differential Diagnosis[edit | edit source]
• Central spinal canal stenosis
• Infection
• Lumbar spondylosis
• Muscle strain
• Paracentral disc herniation
• Spinous process fracture
• Spondylolisthesis
• Vertebral compression fracture
• Scoliosis:
Severe deviation from the normal axis with a peak age from birth to age of 20.
• Trauma:
• Bony bridging in the fracture region
• Ossification in the surrounding soft tissue mantle
• Often accompanied by degenerative disk disease and osteoarthritis in the adjacent joints
• Disk herniation:
Sensory deficits or loss of strength in the extremities
• Calcium pyrophosphate disease (CPPD):
Sclerosis occurs only in the ligament flavum, the interspinous ligaments are not involved[20 Book]
Diagnostic Procedures[edit | edit source]
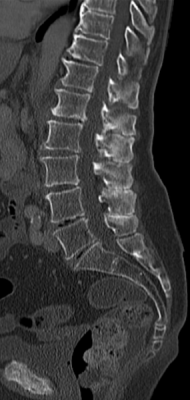
Radiology and CT
Using radiology, the opposing surfaces of the spines are seen. They develop sclerosis and can also become hypertrophied, and flattened. It shows a decreased space between adjacent spinous processes. There is a typical enlargement and flattening of the superior and inferior surfaces of the spinous processes resulting in a faceted appearance. Osteophytes may arise from the spinous processes. [11, level 4][8, level 2C][23, level 5]
MRI
MRI may demonstrate interspinous bursal fluid and a postero-central epidural cyst(s).
Lumbar interspinous bursitis can be diagnosed when hyperintense bursal fluid collections are present between and adjacent to spinous processes.[7, level 2C][11, level 4] The fluid appears as bright or high-signal-intensity areas between the posterior spinous processes.[23, level 5] MRI can be very helpful in determining whether there is resulting posterior compression of the the cal sac. It provides insight into the soft-tissue.[7, level 3] MRI may also show low-signal-intensity sclerosis and change in morphology of the spines—which reflect the findings noted on plain films. [23, level 5]
Outcome Measures[edit | edit source]
The following tests can be used to objectively determine the progress of a patiënt and treatment efficacy:
• Quebec Back Pain Disability Scale
• Visual Analogue Scale
• Oswestry
• Roland‐Morris Disability Questionnaire
• Measurements of spinal mobility:
- Fingertip-to-Floor (FTF) Test
- Modified Schober Test [24, level 4]
Examination[edit | edit source]
The pain can be described as a sharp or deep ache, often worse with activities that increase lumbar lordosis or compression of these structures.[4, level 2B] The L4-L5 level is generally the area which is mostly affected(subjective). Lumbar extension causes maximum amount of pain. Rotation and lateral flexion of the spine is also very painful. Flexion is the movement that causes the least amount of pain.History often reveals an insidious onset without associated trauma. [19 level 2B]
It is difficult to assess proximity of spinous processes on manual palpation due to their overlapping nature. There could be a palpable tenderness of the supraspinous ligament with the patient in a side lying – fetal position.
Palpation of the midline back and spinous processes may reproduce the symptoms.
Physical examination like the ‘Stork test’ or active spinal extension can reproduce the symptoms.
When the patient bends forward, relief is gained. [10, Book]
Medical Management
[edit | edit source]
Injections
If the complaints are of a single trauma, then an injection with a corticosteroid can be very effective.[12, level 4] If the condition is the cause of a chronic micro trauma, then two to four infiltrations are indicated. The injection is given once every two weeks. During the treatment period, extension movements of the lumbar spine should be avoided. In intractable cases, surgery is sometimes indicated.[13, level 2B]
Bursaeitis can produce back pain that responds to injection of local anesthetics[8, level 2C][9, Book].
Surgery
There is one study that investigates the results of surgical procedures following partial or total excision of the processus spinosi. Of the 64 patients who participated, only 11 were free of complaints after the operation. In the other 53 patients, the complaints remained or returned after a short time. [14, level 2B]
In case of propagation of the bursa into the dorsal epidural space, patiënts can suffer (more) from back pain. In this case, surgeons can excise the bursa.[22, Level 4]
Physical Therapy Management
[edit | edit source]
One article suggests conservative treatment should consist of local modalities, over-the-counter analgesics and physical therapy. Physical therapy is based on neuromuscular education and strengthening of the core muscles , posture in a flexion bias and stretching of the hip flexor groups. Some exercises that decrease the lordosis are: stretching of hip flexors, Lower back muscle stretchers, Abdominal crunch, Oblique crunch and hip extensions in supine position. [15, level 2C][16, Book][19 level 5]
Another source says that the treatment goals of physical therapy are reducing the pressure and the lordosis. The treatment includes corrections of ant sacral and vertebral dysfunctions, especially those that increase lordosis. Tight myofascial layers are stretched, and this is followed bt strengthening of the abdominal muscles and the m. psoas in order to reduce lumbar lordosis. [10, level Book][17, level 4][22 level 4]
Also negative heels in the shoes can be used to reduce lordosis[22 level 4]
A cohort study investigates whether a training program can modify lumbar posture ( This training program is not described in the article). Goals of the training program, for patients with lumbar hyperlordosis, were to increase the muscle activity of the abdominal and gluteal muscles (thereby reducing the relative contribution of the erector spinae muscles) and increasing the length of the hip flexor muscles. The results of this study suggest that training has the possibility to change lumbar positions, which decreases or increases lumbar passive tissue strain.[17, level 2B]
Pilates exercises could possibly improve hyperlordosis.[18, level 2B]
Also heat therapy, ergotherapy, muscle strengthening and muscle relaxation can be helpfull in patients with Baastrup disease.[21Book]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
Clinical Bottom Line[edit | edit source]
Kissing spines is characterized by close approximation and contact of the spinous processes. Often injections are used to relief the pain. Physical therapy should include stretching and strengthening exercises to reduce the pressure and the lordosis.
Baastrup’s syndrome is still relatively unkown and is often misdiagnosed and treateded incorrectly. [22, level 4]
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
1. ↑ 1.0 1.1 1.2 1.3 S. Rajasekaran et al. Baastrup’s Disease as a Cause of Neurogenic Claudication. SPINE Volume 28, Number 14, pp E273–E275 ©2003, Lippincott Williams & Wilkins, Inc. (Book)
2. ↑ 2.0 2.1 2.2 S. Kacki et al. Baastrup’s sign (kissing spines): A neglected condition in paleopathology. International Journal of Paleopathology 1 (2011) 104– 110. (Level of Evidence 4)
3. ↑ P.S. Pinto. Spinous process fractures associated with Baastrup disease. Journal of Clinical Imaging 28 (2004) 219–222. (Level of Evidence 4)
4. ↑ 4.0 4.1 4.2 4.3 M.J.Depalma. Ispine: Evidence based interventional spine care. 2011, Demos Medical Publishing. (Level of Evidence 2B)
5. ↑ 5.0 5.1 5.2 G. Aufdemkampe. Orthopedic medicine and manual therapy part 4b SPINE. Houten/Zaventem: Bohn Stafleu Van Longhum, 1991.(Book)
6. ↑ Orthopedische geneeskunde en manuele therapie: Wervelkolom. (book)
7. ↑ 8.0 8.1 8.2 8.3 8.4 8.5 R. Maes et al. Lumbar Interspinous Bursitis (Baastrup Disease) in a Symptomatic Population. 2008, Spine, pE211-E215 (Level of Evidence 2C)
8. ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 Y. Kwong et al. MDCT Findings in Baastrup Disease: Disease or Normal Feature of the Aging Spine? 2011, American Journal of Radiology, p1156-1159 (level of evidence 2C)
9. ↑ 10.0 10.1 10.2 C. Hui, I. Cox. Two Unusual Presentations of Baastrup’s Disease. 2007, Clinical Radiology, p495-497 (Book)
10. ↑ 11.0 11.1 11.2 11.3 D.Hertling, R.M.Kessler. Management of common musculoskeletal disorders: Physical Therapy Principles and Methods. 4th edition. 2006, Lippincott Williams & Wilkins. (Book)
11. ↑ 12.0 12.1 M.J. DePalma et al. Interspinous bursitis in an athlete. 2004, Journal of Bone & Joint Surgery, p1062-1064 (Level of Evidence 4)
12. ↑ Raj Mitra, MD, Usama Ghazi, DO, Dhiruj Kirpalani, MD, Ivan Cheng, MD.Interspinous Ligament Steroid Injections for the Management of Baastrup’s Disease: A Case Report. Arch Phys Med Rehabil. 2007;88:1353-6.(Level of Evidence 4)
13. ↑ T.J. Lamer, J.M. Tiede, D.S. Fenton. Fluoroscopically-Guided Injections to Treat “Kissing Spine” Disease.2008. (www.painphysicianjournal.com) (Level of Evidence 2)
14. ↑ J.W.F.Beks. Kissing Spines: Fact or Fancy? 1998, Neurosurgical Clinic University Hospital, Groningen, The Netherlands. (Level of Evidence 2)
15. ↑ Y. Kwong et al. MDCT Findings in Baastrup Disease: Disease or Normal Feature of the Aging Spine? 2011, American Journal of Radiology, p1156-1159 (level of evidence 2C)
16. ↑ 17.0 17.1 A.Panagos. Spine. 2009. Demos Medical Publishing. (Book)
17. ↑ J.P.Scannell, S.M.McGill. Lumbar posture-should it, and can it, be modified? A study of passive tissue stiffness and lumbar position during activities of daily living. 2003, Physical Therapy. (Level of Evidence 2B)
18. ↑ V.Razaeei, M.Ghofrani. Effect of two month Pilate's exercises on the lumbar hyperlordosis of 15-18 years old girl students. Annals of Biological Research, 2012, 3 (6):2667-2672 (Level of Evidence 2B)
19. Pramod K., Baastrup Syndrome or Kissing Spine Syndrome in Humans: Causes, Symptoms, Treatment. Epainassist, 2012, (level of evidence: 5)
20. H. Imhof et. al. (2011); Spinal Imaging, Baastrup Disease ; Thieme (Book)
21. A. Marcus; Foundations for Integrative Musculosceletal Medicine: An East-West Approach; Kissing spine (Bastrap’s Disease); 2005 (Book)
22. A. Singla et. al.; Baastrup’s disease: The kissing spine; World Journal of Clinical Cases. 2014; 2(2): 45–47; Level 4
23. Paul D. et al., Baastrup Disease. Imaging Series, 2007 (Level of Evidence: 5)
24. Tousignant M. et al., The Modified-Modified Schober Test for range of motion assessment of lumbar flexion in patients with low back pain: a study of criterion validity, intra- and inter-rater reliability and minimum metrically detectable change. Pubmed, 2005. (Level of evidence: 4)