Baastrup Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
'''Original Editors ''' - [[User:Sofie Bourdinon|Sofie Bourdinon]] | '''Original Editors ''' - [[User:Sofie Bourdinon|Sofie Bourdinon]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Search Strategy == | == Search Strategy == | ||
<u>Search engines</u>: Pubmed, Web of knowledge. Google Scholar and Google Books are practical too.<br><u>Keywords</u>: Baastrup syndrome, Baastrup AND etiology, Baastrup disease, kissing spines, Baastrup’s sign, Baastrup syndrome AND physical therapy, Baastrup syndrome AND exercise, Kissing spines AND conservative therapy, Baastrup disease AND surgical management, hyperlordosis AND physical therapy.<br> | <u>Search engines</u>: Pubmed, Web of knowledge. Google Scholar and Google Books are practical too.<br><u>Keywords</u>: Baastrup syndrome, Baastrup AND etiology, Baastrup disease, kissing spines, Baastrup’s sign, Baastrup syndrome AND physical therapy, Baastrup syndrome AND exercise, Kissing spines AND conservative therapy, Baastrup disease AND surgical management, hyperlordosis AND physical therapy.<br> | ||
== Definition/Description == | == Definition/Description == | ||
Baastrup’s Disease, generally known as Kissing Spine, is characterized by degenerative changes of both spinous processes and interspinous soft tissues of two neighbouring vertebrae. This syndrome was firstly characterized by Baastrup back in 1933. On the present-day, it has a worldwide recognition by other authors.[2], [4]The original author describes it as a condition where adjoining lumbar spinous processes become closely approximated to one another, which results in the formation of a new joint between them. [1], [2], [3], [4]The Kissing Spine mainly affects the lumbar area of the spine, with L4-L5 being the most frequently affected level. [5] Nonetheless, in several cases it has also been reported to occur in the cervical spine. [6] | |||
The Kissing Spine has a few consequences such as the formation of hypertrophic spinous processes, which leads to mechanical back pain in combination with degenerative disc disease.[1], [4]In some casereposrts, the syndrome can provoke neuromuscular damage. [6]<br> | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
The lumbar spine, consisting of 5 separated vertebrae, is located between the thoracic spine and the sacrum. Those five vertebrae are the largest of the spine and increase in size from superior to inferior.[7] | |||
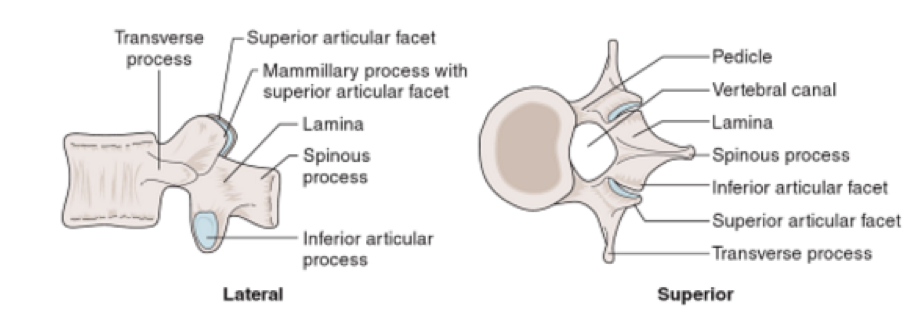
The lumbar vertebrae consist of various parts, in particular the vertebral body, the posterior elements (one process spinous and two processes transversus) and two pedicles.[8] Because of the weight-bearing function of the lumbar spine, the lumbar vertebral bodies are larger than the other vertebral bodies of the spine.[8]The processes spinous are thick and broad, and are dorsally and caudally orientated.[9]The pedicles are the junction between the vertebral body and the neural arch.[11] | |||
[[Image:Baastrup_1.png]] | |||
'''Figure 1''': Aspects of the Lumbar vertebrae [11] | |||
Stability of the lumbar spine is necessary during functional activities. This is primarily obtained by the muscles, which are attached to the posterior elements of the vertebrae. Therefore the spinous processes are subjected to major forces during movements.[9] Besides the muscles, the ligaments also provide a stabilization function. These ligaments can likewise sustain a large compressive load during movements.[10] | |||
Because of the large load on the lumbar part of the spine, there is a higher incidence of pain compared to other regions.[7] The baastrup syndrome affects two adjacent vertebrae, with L4-L5 being the most commonly corroded level. Sometimes it can even result in formation of a bursa in the intermediary interspinous soft tissues [5], [12] | |||
[[Image:Baastrup_2.png]] | |||
'''Figure 2: '''Vertebral Ligaments [11] | |||
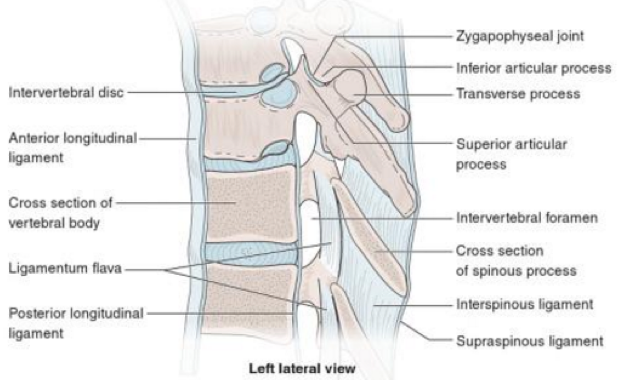
<br> | The interspinous ligament connects two adjacent processes spinous. It primarily prevents excessive spinal flexion by limiting separation of two adjacent spinous processes. It has also been proven that the interspinous ligament controls vertebral rotation during flexion, helping the facet joints remain in contact while gliding. The supraspinous ligament is attached to the posterior tips of the processes spinous from approximately C7 to L4-L5. It limits spinal flexion and resists separation of two neighboring spinous processes. The posterior part of the interspinous and supraspinous ligaments is sensory innervated. The role of this input is to give proprioceptive information and protect against excessive forces. [9]<br> | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
<br> | Just a few studies investigated the influence of the aging process on Baastrup Syndrome, including the study of DePalma M.J. et al.[15]which showed that the average age of patients with Baastrup’s disease is 75. [15] Furthermore, the study of Maes R. et al.[14] confirms that Baastrup Syndrome is more common amongst elderly persons.This does not mean that it cannot occur in younger age groups. The effect of gender is still unknown, so further research is necessary. [14] | ||
Age is not the only factor that is responsible for the evolution of Baastrup Syndrome. Other risk factors are mentioned below: [4], [5] | |||
*Excessive lordosis which results in mechanical pressure; | |||
*Repetitive strains of the interspinous ligament with subsequent degeneration and collapse; | |||
*Incorrect posture; | |||
*Traumatic injuries; | |||
*Tuberculous spondylitis; | |||
*Bilateral forms of congenital hip dislocation; | |||
*Stiffening of the thoracic spine or the thoracolumbar transition; | |||
*Obesity. | |||
The cause of pain has been described to be mainly mechanical because of the neighboring spinous processes coming into contact. Pain worsens with hyperextension or increased lordosis which can been seen in patients with obesity, limitation of hip movements and champion swimmers.[6], [14] | |||
Baastrup syndrome can occur independently or together with symptoms of other disorders, such as spondylolisthesis and spondylosis with osteophyte formation, and loss of disc height. However, there are patients with Baastrup disease without developing the abovementioned factors.[5] | |||
The precise prevalence in the population remains still uncertain, but considering the autopsy of Kacki S. et al.[4] this disease however occurs frequently according to the relatively frequent abnormal changes of the interspinous spaces.[4]<br> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Patients with Baastrup syndrome show a typical excessive lordosis. This results in the mechanical pressure that can cause pain and repetitive strains combined with subsequent degeneration and collapse.[5], [13] Patients with the Kissing Spine often complain about back pain, specifically midline pain that radiates cephalad and caudal. Furthermore, it is mostly increased in combination with extension and less painfull in combination with flexion.[1], [5] The abnormal contact between adjacent spinous processes can lead to neoarthrosis and formation of an adventitious bursa. This can be seen pathologically as well as on MRI (referring to diagnostic procedures). [2], [14], [16] | |||
Other characteristics can be pain upon finger pressure at the level of pathologic interspinous ligament, oedema, cystic lesions, sclerosis, flattening and enlargement of the articulating surfaces and bursitis. Occasionally epidural cysts or midline epidural fibrotic masse scan occur as well regarding to the article of Dimitrios K. Filippiadis et al. [5] | |||
When the rotation and lateral flexion is examined, it will be painful. Flexion is the least painful of all lumbar movements. [17]Baastrup’s disease can result in intraspinal cysts secondary to interspinous bursitis that may rarely which can cause symptomatic spinal stenosis and neurogenic claudation.[2] | |||
Generally, Baastrup syndrome occurs in the lumbar spine with L4-L5 being the most affected region. [5]People who are most likely to suffer from the Kissing Spine are particularly elderly patients with a degenerative disc disease or hyperlordosis. Both of these conditions may lead to chronic contact between adjacent spinous processes. [18]<br> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
The differential diagnosis includes the direct effects of: [1], [19]<br>- Lumbar Spondylosis<br>- Muscle Strain<br>- Spondylolisthesis<br>- Fracture of the spinous process<br>- Vertebral (e.g. lumbar) compression fractures<br>- Infectious etiologies of the spine<br>- Proliferative hyperostosis of the lumbar spinous processes<br>- Degenerative disease of the spine<br>- Cysts<br>- Ossification of the posterior longitudinal ligament<br>- Sclerotic bone metastases to spine<br> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Baastrup Syndrome cannot be diagnosed by inspecting the lumbar spine (see clinical examination). When identifying the Kissing Spine using imaging studies, physicians will have a clearer image of the specific area and can thus prevent misdiagnosis. There are many radiographic methods to determine Baastrup Syndrome. If necessary different methods can becombined in order to gather detailed information of the degenerative and inflammatory signs at the level of interspinous ligament: [5] | |||
'''Computed Tomography CT-scan'''<br>The Kissing Spine can be determined if three radiographic criteria were shown on CT-scans: the close approximation and contact between touching lumbar spinous processes followed by flattening and enlargement of the articulating surfaces and ending with reactive sclerosis of the superior and inferior fragments of adjacent processes.[2], [5], [20] CT- scans can also report detailed degenerative changes (e.g. facet joints hypertrophy, intervertebral disc herniation or spondylolisthesis).[5],[20] | |||
| However, this type of diagnostic procedure has soft tissues limited assessment of disc degeneration, thus interspinous bursae cannot be visualized.[2] CT-scans are also more expensive than radiographic imaging. | ||
[[Image:Baastrup_3.png]] | |||
'''Figure 3:''' CT-scan of Baastrup Syndrome (‘Kissing Spines’) Th12-L1-L2-L3[2] | |||
'''Radiography (X-rays)'''<br>X-rays are analogous to ST-cans, which show[5]: | |||
*Radiographic findings of the close approximation and contact of opposed spinous processes with sclerosis of the articulating surfaces; | |||
*An expansion of the articulating surfaces or articulation of the two affected spinous processes; | |||
*General degenerative changes in the spine. | |||
Advantages of X-rays contain the reasonable cost, availability and a relatively low ionising radiation dose. Nonetheless, radiographic imaging have poor imaging quality in particular at the lower lumbar fragments. | |||
'''Magnetic Resonance Imaging MRI'''<br>In contrary to CT-scans, MRI findings of Baastrup Syndrome may contain interspinous bursal fluid and a postero-central epidural cyst(s) at the opposing spinous processes.[22] When bursal fluid is present between and opposing two affected spinous processes - illustrated as bright and/or high-signal-intensity areas on imaging findings -, lumbar interspinous bursitis will be diagnosed.[14],[21] | |||
Similar to CT scan it includes flattening, sclerosis, enlargement, cystic lesions and bone oedema and at the articulating surfaces of the spinous processes. This type of diagnostic procedure is extremely beneficial in defining whether there is a compression of the posterior thecal sac as an outcome of this contact of the interspinous processes.[21] | |||
Advantages of MRI scan include the lack of ionising radiation and the extremely detailed imaging in various levels (axial, coronal and sagittal).[5] | |||
[[Image:Baastrup_4.png]] | |||
'''Figure 4:''' MRI-scan of Baastrup Syndrome (‘Kissing Spines’) L3-L4[2] | |||
Baastrup’s Syndrome is regularly misdiagnosed and therefore wrongfully treated. Thorough clinically evaluation and analyzing radiographic findings are vital for an accurate diagnosis and to prevent mismanagement.[1]<br> | |||
== Outcome Measures == | == Outcome Measures == | ||
The following tests can be used to objectively determine the progress of a patiënt and treatment efficacy | The following tests can be used to objectively determine the progress of a patiënt and treatment efficacy: | ||
- Fingertip-to-Floor (FTF) Test | *Quebec Back Pain Disability Scale | ||
*Visual Analogue Scale | |||
*Oswestry | |||
*Roland‐Morris Disability Questionnaire | |||
*Measurements of spinal mobility:<br>- Fingertip-to-Floor (FTF) Test | |||
- Modified Schober Test [24, level 4] | |||
== Examination == | == Examination == | ||
The pain can be described as a sharp or deep ache, often worse | Diagnosis of Baastrup’s disease is verified with clinical examination as well as imaging studies. [5] Symptoms include low back pain with midline distribution that exacerbates when performing extension, relieved during flexion and is exaggerated upon finger pressure at the level of the pathologic interspinous ligament. Rotation and lateral flexion are also very painful. [5] The pain can be described as a sharp or deep ache, often worse during physical activities that increase lumbar lordosis or compression of these structures. [9] | ||
Throughout physical examination, the physiotherapist manipulates active/passive techniques with the intention of evoking complaints. Active spinal extension can reproduce the symptoms. The ‘stork test’ (standing on one leg with passive extension of the lumbar spine) is very beneficial in the examination of this disease. [9] When the patient bends forward, relief is also gained. [17] | |||
Figure 5: Stork Test [24]<br> | |||
== Medical Management <br> == | == Medical Management <br> == | ||
The main goal of any therapy for patients with Baastrup syndrome is to reduce in low back pain as well as resume the normal daily activities. The medical treatment can vary between a conservative and a surgical intervention. The diagnosis of the disease is necessary when determining the treatment, which depends on the findings of MRI. When MRI demonstrates active inflammatory changes or edema, local injections will be implemented. When those injections don’t improve the situation of the patient, a surgical treatment will be recommended. [25] (Level of Evidence: 4) | |||
The non-surgical treatment consists of local injections of analgesics or nonsteroidal anti-inflammatory drugs (NSAID’s).[5] (Level of Evidence: 3B) When the complaints are of a single trauma, an injection with a corticosteroid can be effective, but when the condition is the cause of a chronic micro trauma, two to four infiltrations are indicated. The injection is given once every two weeks. During the treatment period, extension movements of the lumbar spine should be avoided. [25] (Level of Evidence: 4), [26] (Level of Evidence: 4)After local anesthesia of the skin and subcutaneous tissues, the injection will be implemented by a 24-gauge styletted needle between the affected processes spinous into the painful interspinous ligaments under fluoroscopic control.[26] (Level of Evidence: 4)Okada K. et al. investigated “the long-term effects of injections of steroid and local anesthetics into interspinous ligaments for the treatment of Baastrup's disease” (Okada K. et al., 2014). An evaluation 30 minutes after the injection represented positive results. The pain was measured by the VAS-scale before and after the treatment. The score of this scale after the treatment indicated less than 60% of their initial score. Therefore, the injection is effective in short-term. The follow-up 1,4 years after the injection indicated also that this intervention is effective for the treatment of Baastrup syndrome.[26] (Level of Evidence: 4) | |||
As mentioned before, in case of no response to non-surgical treatment, medical intervention has to be performed. Suggested surgical therapies contain excision of the bursa, partial or total removal of the process spinous, or osteotomy.[5] (Level of Evidence: 3B) According to Franok S., the average duration of the stay in hospital is up to 31 days, the patients may therefore leave the clinic after ca. 3-5 weeks.[28] (Level of Evidence: 4)However, such invasive therapies occasionally have unsatisfactory outcomes. In fact, it has been confirmed by several studies that numerous patients have developed pain post-surgery.[5] (Level of Evidence: 3B) It is also unclear whether surgery indicates better results. In only 15 to 40 % surgery resulted in remarkably effective outcomes.[27] (Level of Evidence: 1A) | |||
A newer, alternative technique used for the treatment of Baastrup Syndrome are interspinous spacer devices such as a X-STOP. [30] (Level of Evidence: 5) Zhou et al. describes it as “a ‘floating’ device was formed in the interspinous process to increase the distance between spinous processes and the intervertebral foramen” (Zhou D. et al., 2013). Essentially, these contraptions are appropriately implanted between two process spinous of the lumbar spine, therefore the surgical procedure is quite easy and less invasive than the above-mentioned therapies.[29] (Level of Evidence: 2C) | |||
The patients who are undergoing surgery are retrospectively reviewed and were asked to fill in the VAS-scale as well as the Oswestry Disability Index (ODI), pre- and post-surgery. Both of the outcomes show improvement post-operatively in comparison to pre-operatively. Thus, the in-space interspinous methods in the treatment of Baastrup Syndrome are effortless and safe therapies, with remedial results obtained in the initial follow-up.[29] (Level of Evidence: 2C)Despite the short term beneficial results, long-term outcomes regarding the durability of symptomatic relief and the long-term complications specific to the implanted device are yet lacking and need further investigation. [31] (Level of Evidence: 2C)<br> | |||
== Physical Therapy Management <br> == | == Physical Therapy Management <br> == | ||
The main goal of physical therapy for patients with Baastrup Syndrome is to reduce low back pain as well as hyperlodosis and to improve the physical functioning of the spine. Once pain is diminished – either with the help of over-the-counter drugs or conservative therapy –, physical therapy management is very much needed and therefore based on education along with strengthening and stretching of the abdominal plus spinal muscles.[2] (Level of Evidence: 2C), [27] (Level of Evidence: 1A) | |||
As mentioned previously, the treatment of hyperlordosis - among other factors -, is of crucial importance. Hence, the conservative therapy which consists of re-education and correction of core muscles exercises, posture in a flexion bias and stretching of the hip flexor groups. In order to succeed the exercises, they have to be guided by a physiotherapist. [2] (Level of Evidence: 2C) Additionally, these exercises can be performed at home when properly instructed.[32] (Level of Evidence: 2B) Below a few exercises are mentioned with the intention of decreasing the hyperlordosis: <br>• Stretching of hip flexors;<br>• Lower back muscle stretchers; <br>• Abdominal crunch;<br>• Oblique crunch; <br>• Hip extensions in supine position. [2] (Level of Evidence: 2C), [33] (Level of Evidence: 5), [34] (Level of Evidence: 5) | |||
When the abdominal muscles are weak, hip flexors, particularly M. Iliopsoas, are meanly responsible in shaping the lumbar spine.[35] (Level of Evidence: 5)Furthermore the rectus femoris muscle is also a part of the hip flexors. In order to avoid other injuries of the lower-back region, it’s important that a patient with Baastrup syndrome stretches these muscles. The hip flexors can shorten by long-term sitting or resting. When these muscles are too short, it can affect the gluteal muscles and the spinal muscles.[36] (Level of Evidence: 5)The starting position is a lunge position with resting the weight on the knee and the front foot, both resting on the ground. While pushing the hips forward, it’s important that the torso remains straight. Maintain this position for at least 10 seconds, and repeat this three times on each side.[35] (Level of Evidence: 5) | |||
Figure 6: Stretching of hip flexors [35] (Level of Evidence: 5) | |||
It is proven that the motion of the gluteus maximus muscle during the flexion-extension cycle is decreased in patients with chronic low back pain. Thus, training of this muscle should be a part of the physical management program in the rehabilitation of these kind of patients. [37] (Level of Evidence: 3A) | |||
Physical therapy is also said to be helpful for reducing the neuromuscular damage that is provoked by the disease. Neuromuscular education is then needed. Futhermore, other treatment for patients with Baastrup Syndrome such as heat therapy, ergotherapy, muscle strengthening and muscle relaxation can be helpful. [2] (Level of Evidence: 2C) | |||
Nonetheless, due to the beneficial outcomes of physical therapy management, conservative therapies must be attempted by a physiotherapist before using invasive methods such as surgical management as mentioned earlier. [27] (Level of Evidence: 1A)<br> | |||
== Key Research == | == Key Research == | ||
| Line 94: | Line 173: | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Kissing spines is characterized by close approximation and contact of the spinous processes. Often injections are used to relief the pain. Physical therapy should include stretching and strengthening exercises to reduce the pressure and the lordosis. <br>Baastrup’s syndrome is still relatively unkown and is often misdiagnosed and treateded incorrectly. [22, level 4]<br><br> | Kissing spines is characterized by close approximation and contact of the spinous processes. Often injections are used to relief the pain. Physical therapy should include stretching and strengthening exercises to reduce the pressure and the lordosis. <br>Baastrup’s syndrome is still relatively unkown and is often misdiagnosed and treateded incorrectly. [22, level 4]<br><br> | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
| Line 104: | Line 183: | ||
== References == | == References == | ||
<references /> | <references /> | ||
1. Singla A. et al., Baastrup’s disease: the kissing spine, World Journal of Clinical Cases, 2014, 2(2): 45-47. (Level of Evidence: 3B)<br>2. Kwong Y. et al., MDCT Findings in Baastrup Disease: Disease or Normal Feature of the Aging Spine?,American Journal of Roentgenology, 2011, 196(5):1156-9. (Level of Evidence: 2C)<br>3. Yang A. et al., Kissing Spine and the Retrodural Space of Okada: More Than Just a Kiss?, University of Colorado, 2014, 6(3): 287-9. (Level of Evidence: 3B)<br>4. KackiS. et al., Baastrup’s Sign (Kissing Spines): A neglected condition in paleopathology, International Journal of Paleopathology, 2011, 1(2): 104-110. (Level of Evidence: 4)<br>5. Filippiadis D.K. et al., Baastrup’s disease (kissing spines syndrome): a pictorial review, Springer, 2015, 6(1): 123–128. (Level of Evidence: 3B)<br>6. Rajasekaran S. et al., Baastrup’s Disease as a Cause of Neurogenic Claudication: a case report, Lippincott Williams & Wilkins, 2003, 28(14): 273-275. (Level of Evidence: 3B)<br>7. Herkowitz H.N. et al., The Lumbar Spine, Lippincott Williams & Wilkins, 2004, 85-87. (Level of Evidence: 5)<br>8. Bogduk N., Clinical and Radiological Anatomy of the Lumbar Spine, Churchill Livingstone, Elsevier, 2012, 85-98. (Level of Evidence: 5)<br>9. DePalma M.J., iSPINE Evidence Based Interventional Spine Care, Demos Medical, 2011, 4-8. (Level of Evidence: 5)<br>10. Han K-S., Biomechanical roles of spinal muscles in stabilizing the lumbar spine via follower load mechanism, ProQuest, 2008, 92-95. (Level of Evidence: 5)<br>11. Masaracchio M. et al., Clinical Guide to Musculoskeletal Palpation, Human Kinetics, 2014, 203-208. (Level of Evidence: 5)<br>12. Jang E-C. et al., Posterior epidural fibrotic mass associated with Baastrup’s disease, Springer, 2010; 19(2): 165-168. (Level of Evidence: 3B)<br>13. Bywaters E.G.L. et al.,The lumbar interspinous bursae and Baastrup’s syndrome,RheumatolInt, 1982, 2:87-96. (Level of Evidence: 3B)<br>14. Maes R. et al., Lumbar Interspinous Bursitis (Baastrup Disease) in a Symptomatic Population: Prevalence on Magnetic Resonance Imaging, The Spine Journal, 2008, 33(7): 211-215. (Level of Evidence: 4)<br>15. DePalma M.J. et al., What is the source of Chronic Low Back Pain and does age play a role?, Pain Medicine, 2011, 12: 224-233. (Level of Evidence: 2C) <br>16. FarinhaF. et al., Baastrup’s disease: a poorly recognized cause of back pain, ActaReumatol Port, 2015, 40:302-303. (Level of Evidence: 3B) <br>17. Hertling D. et al., Management of common musculoskeletal disorders: Physical Therapy Principles and Methods, Lippincott Williams &amp; Wilkins, 2006, 4th edition. (Level of Evidence: 5) <br>18. Pinto P.S. et al., Spinous Process Fractures associated with Baastrup disease, Clinical Imaging, 2004, 28(3): 219-222. (Level of Evidence: 4)<br>19. Kaye A.D. et al., Pain Management, Cambridge University Press, 2015, <br>20. DePalma M.J. et al., Interspinous Bursitis in an Athlete, The Journal of Bone and Joint Surgery, 2004, 86: 1062-1064. (Level of Evidence: 3B)<br>21. Clifford P.D. et al., Baastrup Disease: Imaging Series, The American Journal of Orthopedics, 2007, 36(10): 560-561. (Level of Evidence: 4) <br>22. Chen C.K.H. et al., Intraspinal Posterior Epidural Cysts Associated with Baastrup's Disease: Report of 10 patients, American Journal of Roentgenology, 2004, 182(1): 191-194. (Level of Evidence: 4)<br>23. Tousignant M. et al., The Modified-Modified Schober Test for range of motion assessment of lumbar flexion in patients with low back pain: a study of criterion validity, intra- and inter-rater reliability and minimum metrically detectable change, Disability and Rehabilitation, 2005, 27(10): 553-559. (Level of Evidence: 4)<br>24. Afbeelding : http://www.physio-pedia.com/Stork_test<br>25. Lamer T.J. et al., Fluoroscopically-Guided Injections to Treat “Kissing Spine” Disease, Pain Physician, 2008; 11: 549-554. (Level of Evidence: 4) <br>26. Okada K. et al., Interspinous Ligament Lidocaine and Steroid Injections for the Management of Baastrup’s Disease : A case Series, Asian Spine Journal, 2014 ; 8(3) : 260-266. (Level of Evidence: 4)<br>27. Cohen S.T. et al., Management of Low Back Pain, British Medical Journal, 2008, 338: 100-106. (Level of Evidence: 1A) <br>28. Franok S., Surgical Treatment of Interspinal Osteoarthrosis (“Kissing Spine”), ActaOrthopaedicaScandinavica, 1943, 14(1-4): 127-152. (Level of Evidence: 4)<br>29. Zhou D. et al., Effects of Interspinous Spacers on Lumbar Degenerative Disease, Experimental and Therapeutic Medicine, 2013, 5: 952-956. (Level of Evidence: 2C)<br>30. Yue J.J. et al., Motion Preservation Surgery of the Spine, Elsevier - Health Sciences Division, 2008, 816 pagina’s. (Level of Evidence: 5)<br>31. Chao S. et al., Interspinous Process Spacer Technology, Techniques in Orthopaedics, 2011, 26(3): 141-145. (Level of Evidence: 2C)<br>32.Scannell J.P. et al., Lumbar posture--should it, and can it, be modified? A study of passive tissue stiffness and lumbar position during activities of daily living, 2003, 83(10): 907-917. (Level of Evidence: 2B)<br>33. Buschbacher R. et al., Spine: Rehabilitation Medicine Quick Reference, Demos Medical, 2009. (Level of Evidence: 5)<br>34. Kerkar P., Baastrup Syndrome or Kissing Spine Syndrome in Humans: Causes, Symptoms, Treatment, Epainassist, 2012. (Level of Evidence: 5)<br>35. Laughlin K., Overcome Neck and Back Pain, Simon & Schuster, 1998, 58-61. (Level of Evidence: 5)<br>36. Ross M., Stretching the Hip Flexors, National Strength & Conditioning Association, 1999, 21(3): 71-72. (Level of Evidence: 5)<br>37. Leinonen V. et al., Back an Hip Extensor Activities During Trunk Flexion/Extension: Effects of Low Back Pain and Rehabilitation, American Congress of Rehabilitation Medicine and the American Academy of Physical Medicine and Rehabilitation, 200, 81: 32-37. (Level of Evidence: 3A) | |||
<br> | |||
Revision as of 12:44, 18 June 2016
Original Editors - Sofie Bourdinon
Top Contributors - Sofie Bourdinon, Scott Cornish, Nikki Rommers, Admin, Arno Vrambout, Kim Jackson, Fien Selderslaghs, Lucinda hampton, Uchechukwu Chukwuemeka, Vidya Acharya, Ceulemans Lisa, Aarti Sareen, WikiSysop and 127.0.0.1
Search Strategy[edit | edit source]
Search engines: Pubmed, Web of knowledge. Google Scholar and Google Books are practical too.
Keywords: Baastrup syndrome, Baastrup AND etiology, Baastrup disease, kissing spines, Baastrup’s sign, Baastrup syndrome AND physical therapy, Baastrup syndrome AND exercise, Kissing spines AND conservative therapy, Baastrup disease AND surgical management, hyperlordosis AND physical therapy.
Definition/Description[edit | edit source]
Baastrup’s Disease, generally known as Kissing Spine, is characterized by degenerative changes of both spinous processes and interspinous soft tissues of two neighbouring vertebrae. This syndrome was firstly characterized by Baastrup back in 1933. On the present-day, it has a worldwide recognition by other authors.[2], [4]The original author describes it as a condition where adjoining lumbar spinous processes become closely approximated to one another, which results in the formation of a new joint between them. [1], [2], [3], [4]The Kissing Spine mainly affects the lumbar area of the spine, with L4-L5 being the most frequently affected level. [5] Nonetheless, in several cases it has also been reported to occur in the cervical spine. [6]
The Kissing Spine has a few consequences such as the formation of hypertrophic spinous processes, which leads to mechanical back pain in combination with degenerative disc disease.[1], [4]In some casereposrts, the syndrome can provoke neuromuscular damage. [6]
Clinically Relevant Anatomy[edit | edit source]
The lumbar spine, consisting of 5 separated vertebrae, is located between the thoracic spine and the sacrum. Those five vertebrae are the largest of the spine and increase in size from superior to inferior.[7]
The lumbar vertebrae consist of various parts, in particular the vertebral body, the posterior elements (one process spinous and two processes transversus) and two pedicles.[8] Because of the weight-bearing function of the lumbar spine, the lumbar vertebral bodies are larger than the other vertebral bodies of the spine.[8]The processes spinous are thick and broad, and are dorsally and caudally orientated.[9]The pedicles are the junction between the vertebral body and the neural arch.[11]
Figure 1: Aspects of the Lumbar vertebrae [11]
Stability of the lumbar spine is necessary during functional activities. This is primarily obtained by the muscles, which are attached to the posterior elements of the vertebrae. Therefore the spinous processes are subjected to major forces during movements.[9] Besides the muscles, the ligaments also provide a stabilization function. These ligaments can likewise sustain a large compressive load during movements.[10]
Because of the large load on the lumbar part of the spine, there is a higher incidence of pain compared to other regions.[7] The baastrup syndrome affects two adjacent vertebrae, with L4-L5 being the most commonly corroded level. Sometimes it can even result in formation of a bursa in the intermediary interspinous soft tissues [5], [12]
Figure 2: Vertebral Ligaments [11]
The interspinous ligament connects two adjacent processes spinous. It primarily prevents excessive spinal flexion by limiting separation of two adjacent spinous processes. It has also been proven that the interspinous ligament controls vertebral rotation during flexion, helping the facet joints remain in contact while gliding. The supraspinous ligament is attached to the posterior tips of the processes spinous from approximately C7 to L4-L5. It limits spinal flexion and resists separation of two neighboring spinous processes. The posterior part of the interspinous and supraspinous ligaments is sensory innervated. The role of this input is to give proprioceptive information and protect against excessive forces. [9]
Epidemiology /Etiology[edit | edit source]
Just a few studies investigated the influence of the aging process on Baastrup Syndrome, including the study of DePalma M.J. et al.[15]which showed that the average age of patients with Baastrup’s disease is 75. [15] Furthermore, the study of Maes R. et al.[14] confirms that Baastrup Syndrome is more common amongst elderly persons.This does not mean that it cannot occur in younger age groups. The effect of gender is still unknown, so further research is necessary. [14]
Age is not the only factor that is responsible for the evolution of Baastrup Syndrome. Other risk factors are mentioned below: [4], [5]
- Excessive lordosis which results in mechanical pressure;
- Repetitive strains of the interspinous ligament with subsequent degeneration and collapse;
- Incorrect posture;
- Traumatic injuries;
- Tuberculous spondylitis;
- Bilateral forms of congenital hip dislocation;
- Stiffening of the thoracic spine or the thoracolumbar transition;
- Obesity.
The cause of pain has been described to be mainly mechanical because of the neighboring spinous processes coming into contact. Pain worsens with hyperextension or increased lordosis which can been seen in patients with obesity, limitation of hip movements and champion swimmers.[6], [14]
Baastrup syndrome can occur independently or together with symptoms of other disorders, such as spondylolisthesis and spondylosis with osteophyte formation, and loss of disc height. However, there are patients with Baastrup disease without developing the abovementioned factors.[5]
The precise prevalence in the population remains still uncertain, but considering the autopsy of Kacki S. et al.[4] this disease however occurs frequently according to the relatively frequent abnormal changes of the interspinous spaces.[4]
Characteristics/Clinical Presentation[edit | edit source]
Patients with Baastrup syndrome show a typical excessive lordosis. This results in the mechanical pressure that can cause pain and repetitive strains combined with subsequent degeneration and collapse.[5], [13] Patients with the Kissing Spine often complain about back pain, specifically midline pain that radiates cephalad and caudal. Furthermore, it is mostly increased in combination with extension and less painfull in combination with flexion.[1], [5] The abnormal contact between adjacent spinous processes can lead to neoarthrosis and formation of an adventitious bursa. This can be seen pathologically as well as on MRI (referring to diagnostic procedures). [2], [14], [16]
Other characteristics can be pain upon finger pressure at the level of pathologic interspinous ligament, oedema, cystic lesions, sclerosis, flattening and enlargement of the articulating surfaces and bursitis. Occasionally epidural cysts or midline epidural fibrotic masse scan occur as well regarding to the article of Dimitrios K. Filippiadis et al. [5]
When the rotation and lateral flexion is examined, it will be painful. Flexion is the least painful of all lumbar movements. [17]Baastrup’s disease can result in intraspinal cysts secondary to interspinous bursitis that may rarely which can cause symptomatic spinal stenosis and neurogenic claudation.[2]
Generally, Baastrup syndrome occurs in the lumbar spine with L4-L5 being the most affected region. [5]People who are most likely to suffer from the Kissing Spine are particularly elderly patients with a degenerative disc disease or hyperlordosis. Both of these conditions may lead to chronic contact between adjacent spinous processes. [18]
Differential Diagnosis[edit | edit source]
The differential diagnosis includes the direct effects of: [1], [19]
- Lumbar Spondylosis
- Muscle Strain
- Spondylolisthesis
- Fracture of the spinous process
- Vertebral (e.g. lumbar) compression fractures
- Infectious etiologies of the spine
- Proliferative hyperostosis of the lumbar spinous processes
- Degenerative disease of the spine
- Cysts
- Ossification of the posterior longitudinal ligament
- Sclerotic bone metastases to spine
Diagnostic Procedures[edit | edit source]
Baastrup Syndrome cannot be diagnosed by inspecting the lumbar spine (see clinical examination). When identifying the Kissing Spine using imaging studies, physicians will have a clearer image of the specific area and can thus prevent misdiagnosis. There are many radiographic methods to determine Baastrup Syndrome. If necessary different methods can becombined in order to gather detailed information of the degenerative and inflammatory signs at the level of interspinous ligament: [5]
Computed Tomography CT-scan
The Kissing Spine can be determined if three radiographic criteria were shown on CT-scans: the close approximation and contact between touching lumbar spinous processes followed by flattening and enlargement of the articulating surfaces and ending with reactive sclerosis of the superior and inferior fragments of adjacent processes.[2], [5], [20] CT- scans can also report detailed degenerative changes (e.g. facet joints hypertrophy, intervertebral disc herniation or spondylolisthesis).[5],[20]
However, this type of diagnostic procedure has soft tissues limited assessment of disc degeneration, thus interspinous bursae cannot be visualized.[2] CT-scans are also more expensive than radiographic imaging.
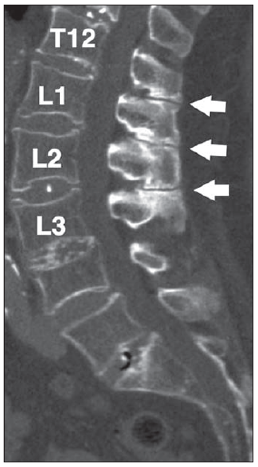
Figure 3: CT-scan of Baastrup Syndrome (‘Kissing Spines’) Th12-L1-L2-L3[2]
Radiography (X-rays)
X-rays are analogous to ST-cans, which show[5]:
- Radiographic findings of the close approximation and contact of opposed spinous processes with sclerosis of the articulating surfaces;
- An expansion of the articulating surfaces or articulation of the two affected spinous processes;
- General degenerative changes in the spine.
Advantages of X-rays contain the reasonable cost, availability and a relatively low ionising radiation dose. Nonetheless, radiographic imaging have poor imaging quality in particular at the lower lumbar fragments.
Magnetic Resonance Imaging MRI
In contrary to CT-scans, MRI findings of Baastrup Syndrome may contain interspinous bursal fluid and a postero-central epidural cyst(s) at the opposing spinous processes.[22] When bursal fluid is present between and opposing two affected spinous processes - illustrated as bright and/or high-signal-intensity areas on imaging findings -, lumbar interspinous bursitis will be diagnosed.[14],[21]
Similar to CT scan it includes flattening, sclerosis, enlargement, cystic lesions and bone oedema and at the articulating surfaces of the spinous processes. This type of diagnostic procedure is extremely beneficial in defining whether there is a compression of the posterior thecal sac as an outcome of this contact of the interspinous processes.[21]
Advantages of MRI scan include the lack of ionising radiation and the extremely detailed imaging in various levels (axial, coronal and sagittal).[5]
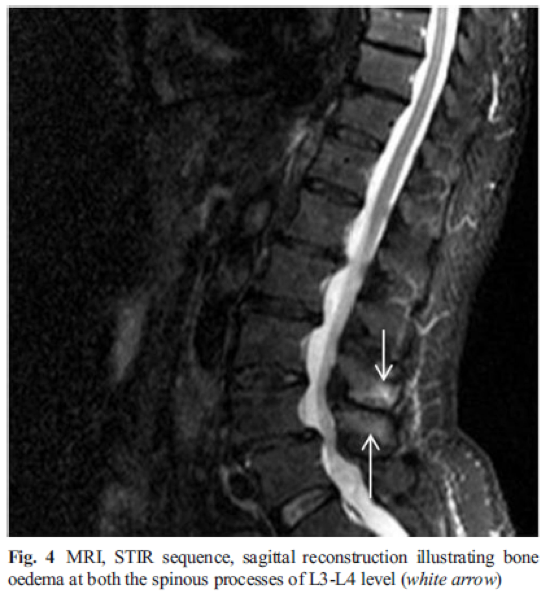
Figure 4: MRI-scan of Baastrup Syndrome (‘Kissing Spines’) L3-L4[2]
Baastrup’s Syndrome is regularly misdiagnosed and therefore wrongfully treated. Thorough clinically evaluation and analyzing radiographic findings are vital for an accurate diagnosis and to prevent mismanagement.[1]
Outcome Measures[edit | edit source]
The following tests can be used to objectively determine the progress of a patiënt and treatment efficacy:
- Quebec Back Pain Disability Scale
- Visual Analogue Scale
- Oswestry
- Roland‐Morris Disability Questionnaire
- Measurements of spinal mobility:
- Fingertip-to-Floor (FTF) Test
- Modified Schober Test [24, level 4]
Examination[edit | edit source]
Diagnosis of Baastrup’s disease is verified with clinical examination as well as imaging studies. [5] Symptoms include low back pain with midline distribution that exacerbates when performing extension, relieved during flexion and is exaggerated upon finger pressure at the level of the pathologic interspinous ligament. Rotation and lateral flexion are also very painful. [5] The pain can be described as a sharp or deep ache, often worse during physical activities that increase lumbar lordosis or compression of these structures. [9]
Throughout physical examination, the physiotherapist manipulates active/passive techniques with the intention of evoking complaints. Active spinal extension can reproduce the symptoms. The ‘stork test’ (standing on one leg with passive extension of the lumbar spine) is very beneficial in the examination of this disease. [9] When the patient bends forward, relief is also gained. [17]
Figure 5: Stork Test [24]
Medical Management
[edit | edit source]
The main goal of any therapy for patients with Baastrup syndrome is to reduce in low back pain as well as resume the normal daily activities. The medical treatment can vary between a conservative and a surgical intervention. The diagnosis of the disease is necessary when determining the treatment, which depends on the findings of MRI. When MRI demonstrates active inflammatory changes or edema, local injections will be implemented. When those injections don’t improve the situation of the patient, a surgical treatment will be recommended. [25] (Level of Evidence: 4)
The non-surgical treatment consists of local injections of analgesics or nonsteroidal anti-inflammatory drugs (NSAID’s).[5] (Level of Evidence: 3B) When the complaints are of a single trauma, an injection with a corticosteroid can be effective, but when the condition is the cause of a chronic micro trauma, two to four infiltrations are indicated. The injection is given once every two weeks. During the treatment period, extension movements of the lumbar spine should be avoided. [25] (Level of Evidence: 4), [26] (Level of Evidence: 4)After local anesthesia of the skin and subcutaneous tissues, the injection will be implemented by a 24-gauge styletted needle between the affected processes spinous into the painful interspinous ligaments under fluoroscopic control.[26] (Level of Evidence: 4)Okada K. et al. investigated “the long-term effects of injections of steroid and local anesthetics into interspinous ligaments for the treatment of Baastrup's disease” (Okada K. et al., 2014). An evaluation 30 minutes after the injection represented positive results. The pain was measured by the VAS-scale before and after the treatment. The score of this scale after the treatment indicated less than 60% of their initial score. Therefore, the injection is effective in short-term. The follow-up 1,4 years after the injection indicated also that this intervention is effective for the treatment of Baastrup syndrome.[26] (Level of Evidence: 4)
As mentioned before, in case of no response to non-surgical treatment, medical intervention has to be performed. Suggested surgical therapies contain excision of the bursa, partial or total removal of the process spinous, or osteotomy.[5] (Level of Evidence: 3B) According to Franok S., the average duration of the stay in hospital is up to 31 days, the patients may therefore leave the clinic after ca. 3-5 weeks.[28] (Level of Evidence: 4)However, such invasive therapies occasionally have unsatisfactory outcomes. In fact, it has been confirmed by several studies that numerous patients have developed pain post-surgery.[5] (Level of Evidence: 3B) It is also unclear whether surgery indicates better results. In only 15 to 40 % surgery resulted in remarkably effective outcomes.[27] (Level of Evidence: 1A)
A newer, alternative technique used for the treatment of Baastrup Syndrome are interspinous spacer devices such as a X-STOP. [30] (Level of Evidence: 5) Zhou et al. describes it as “a ‘floating’ device was formed in the interspinous process to increase the distance between spinous processes and the intervertebral foramen” (Zhou D. et al., 2013). Essentially, these contraptions are appropriately implanted between two process spinous of the lumbar spine, therefore the surgical procedure is quite easy and less invasive than the above-mentioned therapies.[29] (Level of Evidence: 2C)
The patients who are undergoing surgery are retrospectively reviewed and were asked to fill in the VAS-scale as well as the Oswestry Disability Index (ODI), pre- and post-surgery. Both of the outcomes show improvement post-operatively in comparison to pre-operatively. Thus, the in-space interspinous methods in the treatment of Baastrup Syndrome are effortless and safe therapies, with remedial results obtained in the initial follow-up.[29] (Level of Evidence: 2C)Despite the short term beneficial results, long-term outcomes regarding the durability of symptomatic relief and the long-term complications specific to the implanted device are yet lacking and need further investigation. [31] (Level of Evidence: 2C)
Physical Therapy Management
[edit | edit source]
The main goal of physical therapy for patients with Baastrup Syndrome is to reduce low back pain as well as hyperlodosis and to improve the physical functioning of the spine. Once pain is diminished – either with the help of over-the-counter drugs or conservative therapy –, physical therapy management is very much needed and therefore based on education along with strengthening and stretching of the abdominal plus spinal muscles.[2] (Level of Evidence: 2C), [27] (Level of Evidence: 1A)
As mentioned previously, the treatment of hyperlordosis - among other factors -, is of crucial importance. Hence, the conservative therapy which consists of re-education and correction of core muscles exercises, posture in a flexion bias and stretching of the hip flexor groups. In order to succeed the exercises, they have to be guided by a physiotherapist. [2] (Level of Evidence: 2C) Additionally, these exercises can be performed at home when properly instructed.[32] (Level of Evidence: 2B) Below a few exercises are mentioned with the intention of decreasing the hyperlordosis:
• Stretching of hip flexors;
• Lower back muscle stretchers;
• Abdominal crunch;
• Oblique crunch;
• Hip extensions in supine position. [2] (Level of Evidence: 2C), [33] (Level of Evidence: 5), [34] (Level of Evidence: 5)
When the abdominal muscles are weak, hip flexors, particularly M. Iliopsoas, are meanly responsible in shaping the lumbar spine.[35] (Level of Evidence: 5)Furthermore the rectus femoris muscle is also a part of the hip flexors. In order to avoid other injuries of the lower-back region, it’s important that a patient with Baastrup syndrome stretches these muscles. The hip flexors can shorten by long-term sitting or resting. When these muscles are too short, it can affect the gluteal muscles and the spinal muscles.[36] (Level of Evidence: 5)The starting position is a lunge position with resting the weight on the knee and the front foot, both resting on the ground. While pushing the hips forward, it’s important that the torso remains straight. Maintain this position for at least 10 seconds, and repeat this three times on each side.[35] (Level of Evidence: 5)
Figure 6: Stretching of hip flexors [35] (Level of Evidence: 5)
It is proven that the motion of the gluteus maximus muscle during the flexion-extension cycle is decreased in patients with chronic low back pain. Thus, training of this muscle should be a part of the physical management program in the rehabilitation of these kind of patients. [37] (Level of Evidence: 3A)
Physical therapy is also said to be helpful for reducing the neuromuscular damage that is provoked by the disease. Neuromuscular education is then needed. Futhermore, other treatment for patients with Baastrup Syndrome such as heat therapy, ergotherapy, muscle strengthening and muscle relaxation can be helpful. [2] (Level of Evidence: 2C)
Nonetheless, due to the beneficial outcomes of physical therapy management, conservative therapies must be attempted by a physiotherapist before using invasive methods such as surgical management as mentioned earlier. [27] (Level of Evidence: 1A)
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
Clinical Bottom Line[edit | edit source]
Kissing spines is characterized by close approximation and contact of the spinous processes. Often injections are used to relief the pain. Physical therapy should include stretching and strengthening exercises to reduce the pressure and the lordosis.
Baastrup’s syndrome is still relatively unkown and is often misdiagnosed and treateded incorrectly. [22, level 4]
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
1. Singla A. et al., Baastrup’s disease: the kissing spine, World Journal of Clinical Cases, 2014, 2(2): 45-47. (Level of Evidence: 3B)
2. Kwong Y. et al., MDCT Findings in Baastrup Disease: Disease or Normal Feature of the Aging Spine?,American Journal of Roentgenology, 2011, 196(5):1156-9. (Level of Evidence: 2C)
3. Yang A. et al., Kissing Spine and the Retrodural Space of Okada: More Than Just a Kiss?, University of Colorado, 2014, 6(3): 287-9. (Level of Evidence: 3B)
4. KackiS. et al., Baastrup’s Sign (Kissing Spines): A neglected condition in paleopathology, International Journal of Paleopathology, 2011, 1(2): 104-110. (Level of Evidence: 4)
5. Filippiadis D.K. et al., Baastrup’s disease (kissing spines syndrome): a pictorial review, Springer, 2015, 6(1): 123–128. (Level of Evidence: 3B)
6. Rajasekaran S. et al., Baastrup’s Disease as a Cause of Neurogenic Claudication: a case report, Lippincott Williams & Wilkins, 2003, 28(14): 273-275. (Level of Evidence: 3B)
7. Herkowitz H.N. et al., The Lumbar Spine, Lippincott Williams & Wilkins, 2004, 85-87. (Level of Evidence: 5)
8. Bogduk N., Clinical and Radiological Anatomy of the Lumbar Spine, Churchill Livingstone, Elsevier, 2012, 85-98. (Level of Evidence: 5)
9. DePalma M.J., iSPINE Evidence Based Interventional Spine Care, Demos Medical, 2011, 4-8. (Level of Evidence: 5)
10. Han K-S., Biomechanical roles of spinal muscles in stabilizing the lumbar spine via follower load mechanism, ProQuest, 2008, 92-95. (Level of Evidence: 5)
11. Masaracchio M. et al., Clinical Guide to Musculoskeletal Palpation, Human Kinetics, 2014, 203-208. (Level of Evidence: 5)
12. Jang E-C. et al., Posterior epidural fibrotic mass associated with Baastrup’s disease, Springer, 2010; 19(2): 165-168. (Level of Evidence: 3B)
13. Bywaters E.G.L. et al.,The lumbar interspinous bursae and Baastrup’s syndrome,RheumatolInt, 1982, 2:87-96. (Level of Evidence: 3B)
14. Maes R. et al., Lumbar Interspinous Bursitis (Baastrup Disease) in a Symptomatic Population: Prevalence on Magnetic Resonance Imaging, The Spine Journal, 2008, 33(7): 211-215. (Level of Evidence: 4)
15. DePalma M.J. et al., What is the source of Chronic Low Back Pain and does age play a role?, Pain Medicine, 2011, 12: 224-233. (Level of Evidence: 2C)
16. FarinhaF. et al., Baastrup’s disease: a poorly recognized cause of back pain, ActaReumatol Port, 2015, 40:302-303. (Level of Evidence: 3B)
17. Hertling D. et al., Management of common musculoskeletal disorders: Physical Therapy Principles and Methods, Lippincott Williams & Wilkins, 2006, 4th edition. (Level of Evidence: 5)
18. Pinto P.S. et al., Spinous Process Fractures associated with Baastrup disease, Clinical Imaging, 2004, 28(3): 219-222. (Level of Evidence: 4)
19. Kaye A.D. et al., Pain Management, Cambridge University Press, 2015,
20. DePalma M.J. et al., Interspinous Bursitis in an Athlete, The Journal of Bone and Joint Surgery, 2004, 86: 1062-1064. (Level of Evidence: 3B)
21. Clifford P.D. et al., Baastrup Disease: Imaging Series, The American Journal of Orthopedics, 2007, 36(10): 560-561. (Level of Evidence: 4)
22. Chen C.K.H. et al., Intraspinal Posterior Epidural Cysts Associated with Baastrup's Disease: Report of 10 patients, American Journal of Roentgenology, 2004, 182(1): 191-194. (Level of Evidence: 4)
23. Tousignant M. et al., The Modified-Modified Schober Test for range of motion assessment of lumbar flexion in patients with low back pain: a study of criterion validity, intra- and inter-rater reliability and minimum metrically detectable change, Disability and Rehabilitation, 2005, 27(10): 553-559. (Level of Evidence: 4)
24. Afbeelding : http://www.physio-pedia.com/Stork_test
25. Lamer T.J. et al., Fluoroscopically-Guided Injections to Treat “Kissing Spine” Disease, Pain Physician, 2008; 11: 549-554. (Level of Evidence: 4)
26. Okada K. et al., Interspinous Ligament Lidocaine and Steroid Injections for the Management of Baastrup’s Disease : A case Series, Asian Spine Journal, 2014 ; 8(3) : 260-266. (Level of Evidence: 4)
27. Cohen S.T. et al., Management of Low Back Pain, British Medical Journal, 2008, 338: 100-106. (Level of Evidence: 1A)
28. Franok S., Surgical Treatment of Interspinal Osteoarthrosis (“Kissing Spine”), ActaOrthopaedicaScandinavica, 1943, 14(1-4): 127-152. (Level of Evidence: 4)
29. Zhou D. et al., Effects of Interspinous Spacers on Lumbar Degenerative Disease, Experimental and Therapeutic Medicine, 2013, 5: 952-956. (Level of Evidence: 2C)
30. Yue J.J. et al., Motion Preservation Surgery of the Spine, Elsevier - Health Sciences Division, 2008, 816 pagina’s. (Level of Evidence: 5)
31. Chao S. et al., Interspinous Process Spacer Technology, Techniques in Orthopaedics, 2011, 26(3): 141-145. (Level of Evidence: 2C)
32.Scannell J.P. et al., Lumbar posture--should it, and can it, be modified? A study of passive tissue stiffness and lumbar position during activities of daily living, 2003, 83(10): 907-917. (Level of Evidence: 2B)
33. Buschbacher R. et al., Spine: Rehabilitation Medicine Quick Reference, Demos Medical, 2009. (Level of Evidence: 5)
34. Kerkar P., Baastrup Syndrome or Kissing Spine Syndrome in Humans: Causes, Symptoms, Treatment, Epainassist, 2012. (Level of Evidence: 5)
35. Laughlin K., Overcome Neck and Back Pain, Simon & Schuster, 1998, 58-61. (Level of Evidence: 5)
36. Ross M., Stretching the Hip Flexors, National Strength & Conditioning Association, 1999, 21(3): 71-72. (Level of Evidence: 5)
37. Leinonen V. et al., Back an Hip Extensor Activities During Trunk Flexion/Extension: Effects of Low Back Pain and Rehabilitation, American Congress of Rehabilitation Medicine and the American Academy of Physical Medicine and Rehabilitation, 200, 81: 32-37. (Level of Evidence: 3A)