Assessment Before Moving and Handling: Difference between revisions
No edit summary |
No edit summary |
||
| Line 18: | Line 18: | ||
*Time/Date - "Can you tell me today's date?" or "What day of the week is it?" or "What year is it?" | *Time/Date - "Can you tell me today's date?" or "What day of the week is it?" or "What year is it?" | ||
*Situation - "Can you tell me what brought you to the hospital or health centre?" or "What surgery did you have?" | *Situation - "Can you tell me what brought you to the hospital or health centre?" or "What surgery did you have?" | ||
There are many other outcome measures that can be used to assess cognition relevant to the specific environment you work in or specific populations you work with, which can provide insight as to the patient's appropriateness for participation in any rehabilitation activities. The [[Richmond Agitation-Sedation Scale (RASS)]] is one such instrument designed to assess the level of alertness and agitated behaviour in critically-ill patients, <ref name=":03">Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, Tesoro EP, Elswick RK. [https://www.atsjournals.org/doi/full/10.1164/rccm.2107138 The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients]. American journal of respiratory and critical care medicine. 2002 Nov 15;166(10):1338-44.</ref> A RASS Score between -1 and +1 generally indicate that the patient possess a level of alertness that will allow them to participate in rehabilitation with a minimal risk of adverse effects.<ref>Green M, Marzano V, Leditschke IA, Mitchell I, Bissett B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4889100/ Mobilization of intensive care patients: a multidisciplinary practical guide for clinicians.] J Multidiscip Healthc 2016; 25(9): 247-56.</ref><ref name=":2" /> While the mini-mental state examination is used primarily to screen for [[Cognitive Impairments|cognitive impairment]] in [[Older People Introduction|older adults]], and estimate the severity of cognitive impairment at a given point in time, and assesses a number of subsets of cognitive status including attention, language, [[memory]], orientation, and visuospatial proficiency.<ref>Folstein MF, Folstein SE, McHugh PR "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov; 12(3):189-98.</ref> <ref name=":1">Sleutjes DK, Harmsen IJ, van Bergen FS, Oosterman JM, Dautzenberg PL, Kessels RP. | There are many other outcome measures that can be used to assess cognition relevant to the specific environment you work in or specific populations you work with, which can provide insight as to the patient's appropriateness for participation in any rehabilitation activities. The [[Richmond Agitation-Sedation Scale (RASS)]] is one such instrument designed to assess the level of alertness and agitated behaviour in critically-ill patients, <ref name=":03">Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, Tesoro EP, Elswick RK. [https://www.atsjournals.org/doi/full/10.1164/rccm.2107138 The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients]. American journal of respiratory and critical care medicine. 2002 Nov 15;166(10):1338-44.</ref> A RASS Score between -1 and +1 generally indicate that the patient possess a level of alertness that will allow them to participate in rehabilitation with a minimal risk of adverse effects.<ref>Green M, Marzano V, Leditschke IA, Mitchell I, Bissett B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4889100/ Mobilization of intensive care patients: a multidisciplinary practical guide for clinicians.] J Multidiscip Healthc 2016; 25(9): 247-56.</ref><ref name=":2" /> While the mini-mental state examination is used primarily to screen for [[Cognitive Impairments|cognitive impairment]] in [[Older People Introduction|older adults]], and estimate the severity of cognitive impairment at a given point in time, and assesses a number of subsets of cognitive status including attention, language, [[memory]], orientation, and visuospatial proficiency.<ref>Folstein MF, Folstein SE, McHugh PR "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov; 12(3):189-98.</ref> <ref name=":1">Sleutjes DK, Harmsen IJ, van Bergen FS, Oosterman JM, Dautzenberg PL, Kessels RP. Validity of the Mini-Mental State Examination-2 in Diagnosing Mild Cognitive Impairment and Dementia in Patients Visiting an Outpatient Clinic in the Netherlands. Alzheimer disease and associated disorders. 2020 Jul;34(3):278. | ||
</ref> A Mini Mental State Score of 0 - 17 is interpreted as severe cognitive impairment, which may impact participation in rehabilitation activities. <ref>Faber RA. The neuropsychiatric mental status examination. ''Semin Neurol''. 2009;29(3):185–193. Level of evidence C</ref> | |||
== Emotional Status == | == Emotional Status == | ||
Confusion, Agitation, Aggression, Depression, Cooperation | Confusion, Agitation, Aggression, Depression, Cooperation | ||
== Vision == | == Vision == | ||
== Hearing == | == Hearing == | ||
=== Cardiovascular Status === | === Cardiovascular Status === | ||
==== Pulses and Heart Rate ==== | ==== Pulses and Heart Rate ==== | ||
[[Pulse rate]] is defined as the wave of blood in the artery created by contraction of the left ventricle during a cardiac cycle. The most common sites of measuring the peripheral pulses are the radial pulse, ulnar pulse, brachial pulse in the upper extremity, and the posterior tibialis or the [[Dorsalis Pedis Artery|dorsalis pedis]] pulse as well as the femoral pulse in the lower extremity. Clinicians also measure the carotid pulse in the neck. In day to day practice, the radial pulse is the most frequently used site for checking the peripheral pulse, where the pulse is palpated on the radial aspect of the forearm, just proximal to the [[Wrist and Hand|wrist joint.]] | [[Pulse rate]] is defined as the wave of blood in the artery created by contraction of the left ventricle during a cardiac cycle. The most common sites of measuring the peripheral pulses are the radial pulse, ulnar pulse, brachial pulse in the upper extremity, and the posterior tibialis or the [[Dorsalis Pedis Artery|dorsalis pedis]] pulse as well as the femoral pulse in the lower extremity. Clinicians also measure the carotid pulse in the neck. In day to day practice, the radial pulse is the most frequently used site for checking the peripheral pulse, where the pulse is palpated on the radial aspect of the forearm, just proximal to the [[Wrist and Hand|wrist joint.]] | ||
# '''Rate:''' | # '''Rate:''' | ||
#* The normal range used in an adult is between 60 to 100 beats /minute with rates above 100 beats/minute and rates and below 60 beats per minute, referred to as tachycardia and bradycardia, respectively. Changes in the rate of the pulse, along with changes in respiration is called sinus arrhythmia. In sinus arrhythmia, the pulse rate becomes faster during inspiration and slows down during expiration. | #* The normal range used in an adult is between 60 to 100 beats /minute with rates above 100 beats/minute and rates and below 60 beats per minute, referred to as tachycardia and bradycardia, respectively. Changes in the rate of the pulse, along with changes in respiration is called sinus arrhythmia. In sinus arrhythmia, the pulse rate becomes faster during inspiration and slows down during expiration. | ||
# '''Rhythm:''' | # '''Rhythm:''' | ||
#* Assessing whether the rhythm of the pulse is regular or irregular is essential. The pulse could be regular, irregular, or irregularly irregular. Irregularly irregular pattern is more commonly indicative of processes like atrial flutter or atrial fibrillation. | #* Assessing whether the rhythm of the pulse is regular or irregular is essential. The pulse could be regular, irregular, or irregularly irregular. Irregularly irregular pattern is more commonly indicative of processes like atrial flutter or atrial fibrillation. | ||
# '''Volume:''' | # '''Volume:''' | ||
#* Assessing the volume of the pulse is equally essential. A low volume pulse could be indicative of inadequate tissue perfusion; this can be a crucial indicator of indirect prediction of the systolic blood pressure of the patient. | #* Assessing the volume of the pulse is equally essential. A low volume pulse could be indicative of inadequate tissue perfusion; this can be a crucial indicator of indirect prediction of the systolic blood pressure of the patient. | ||
# '''Symmetry:''' | # '''Symmetry:''' | ||
#* Checking for symmetry of the pulses is important as asymmetrical pulses could be seen in conditions like aortic dissection, aortic coarctation, Takayasu arteritis, and subclavian steal syndrome. | #* Checking for symmetry of the pulses is important as asymmetrical pulses could be seen in conditions like aortic dissection, aortic coarctation, Takayasu arteritis, and subclavian steal syndrome. | ||
# '''Amplitude and Rate of Increase:''' | # '''Amplitude and Rate of Increase:''' | ||
#* Low amplitude and low rate of increase could be seen in conditions like aortic stenosis, besides weak perfusion states. High amplitude and rapid rise can be indicative of conditions like aortic regurgitation, mitral regurgitation, and hypertrophic cardiomyopathy.<ref name=":0">Sapra A, Malik A, Bhandari P. Vital Sign Assessment. InStatPearls [Internet] 2019 Dec 28. StatPearls Publishing.</ | #* Low amplitude and low rate of increase could be seen in conditions like aortic stenosis, besides weak perfusion states. High amplitude and rapid rise can be indicative of conditions like aortic regurgitation, mitral regurgitation, and hypertrophic cardiomyopathy.<nowiki><ref name=":0">Sapra A, Malik A, Bhandari P. Vital Sign Assessment. InStatPearls [Internet] 2019 Dec 28. StatPearls Publishing.</nowiki> | ||
==== Blood Pressure ==== | ==== Blood Pressure ==== | ||
[[Blood Pressure|Blood pressure]] is the force of circulating blood on the walls of the arteries, mainly in large arteries of the systemic circulation. Blood pressure incorporates two measurements: | [[Blood Pressure|Blood pressure]] is the force of circulating blood on the walls of the arteries, mainly in large arteries of the systemic circulation. Blood pressure incorporates two measurements: | ||
Revision as of 23:45, 23 May 2023
Original Editors - Add your name/s here if you are the original editor/s of this page. User Name
Top Contributors - Naomi O'Reilly, Ewa Jaraczewska, Jess Bell, Tarina van der Stockt, Kim Jackson and Carina Therese Magtibay
Introduction[edit | edit source]
Moving and handling of people is a part of everyday working life, and a core activity for many rehabilitation professionals. Many rehabilitation techniques and interventions frequently rely on handling and moving patients. While adequate training in manual handling is key element of safe patient handling, having a clear understanding of all the elements that can impact on patient handling are key to providing a safe environment. The ability to think critically and interpret patient cognition, behaviours and physiologic changes is essential to ensure safety when moving with a patient. The skills of observational and physical assessment are powerful tools for detecting both subtle and obvious changes in a patient’s health.
Communication[edit | edit source]
Communication is a "two-way process of reaching mutual understanding, in which participants not only exchange (encode-decode) information, news, ideas and feelings but also create and share meaning. [1] Transferring of information can take the form of verbal communication such as speech and listening or non-verbal communication including body language, eye contact, gestures and expressions. [2] Effective clinical communication skills can improve health outcomes and are considered an important aspect of high-quality healthcare.[3]
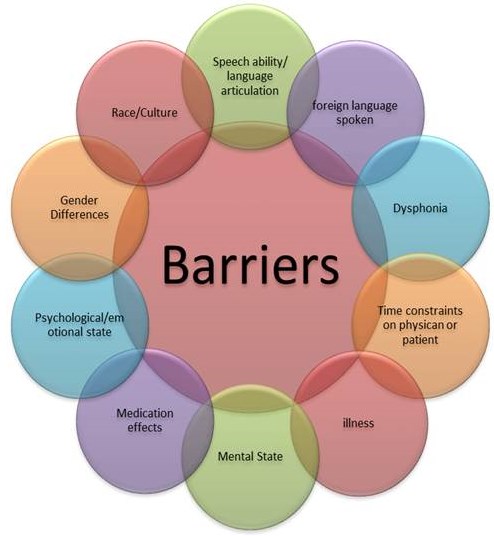
Communication can impact on your interaction with patients in a variety of ways with poor communication shown to lead to adverse patient outcomes and reduced compliance to treatment, while conversely effective communication leads to productive health changes and higher satisfaction among patients.[4]. Language barriers, physical impairments including hearing or vision loss, cognitive impairment, the physical environment and even a person's emotional state can all affect the communication cycle. In healthcare specifically, there can be barriers for the patients as well as communication barriers for the healthcare professional. Environmental factors have been identified as being a key barrier to therapist-patient communication i.e. a noisy environment or lack of privacy may result in a patient not communicating precisely what they need to.[5][6] Patient barriers may include language barriers, cultural barriers, medication effects, anxiety, pain and physical discomfort.[7] For healthcare professionals, other identified communication barriers include time management and an inability to build rapport with patients,[8] as well as high patient loads, stress and anxiety. Similarly. healthcare professionals may not be able to communicate effectively if they do not feel confident in their clinical diagnosis or their treatment plan.[6]
Cognitive Status[edit | edit source]
Cognitive status is crucial in determining if a patient can safely participate in assessment, positioning, transferring and mobilising a patient. [9] A simple method of quickly assessing a patients cognitive status is by determining their orientation at the time of initial assessment and during any manual handling tasks. A patient's level of orientation can convey a lot about their cognitive status, and provide some basic information on their ability to answer questions and possibly follow instructions.[10] Assessing orientation can be accomplished by asking the patient a series of standard questions:*Person - "Can you tell me your name and date of birth?"
- Place - "Can you tell me where you are right now?" or "Can you tell me what city we are in?"
- Time/Date - "Can you tell me today's date?" or "What day of the week is it?" or "What year is it?"
- Situation - "Can you tell me what brought you to the hospital or health centre?" or "What surgery did you have?"
There are many other outcome measures that can be used to assess cognition relevant to the specific environment you work in or specific populations you work with, which can provide insight as to the patient's appropriateness for participation in any rehabilitation activities. The Richmond Agitation-Sedation Scale (RASS) is one such instrument designed to assess the level of alertness and agitated behaviour in critically-ill patients, [11] A RASS Score between -1 and +1 generally indicate that the patient possess a level of alertness that will allow them to participate in rehabilitation with a minimal risk of adverse effects.[12][13] While the mini-mental state examination is used primarily to screen for cognitive impairment in older adults, and estimate the severity of cognitive impairment at a given point in time, and assesses a number of subsets of cognitive status including attention, language, memory, orientation, and visuospatial proficiency.[14] [15] A Mini Mental State Score of 0 - 17 is interpreted as severe cognitive impairment, which may impact participation in rehabilitation activities. [16]
Emotional Status[edit | edit source]
Confusion, Agitation, Aggression, Depression, Cooperation
Vision[edit | edit source]
Hearing[edit | edit source]
Cardiovascular Status[edit | edit source]
Pulses and Heart Rate[edit | edit source]
Pulse rate is defined as the wave of blood in the artery created by contraction of the left ventricle during a cardiac cycle. The most common sites of measuring the peripheral pulses are the radial pulse, ulnar pulse, brachial pulse in the upper extremity, and the posterior tibialis or the dorsalis pedis pulse as well as the femoral pulse in the lower extremity. Clinicians also measure the carotid pulse in the neck. In day to day practice, the radial pulse is the most frequently used site for checking the peripheral pulse, where the pulse is palpated on the radial aspect of the forearm, just proximal to the wrist joint.
- Rate:
- The normal range used in an adult is between 60 to 100 beats /minute with rates above 100 beats/minute and rates and below 60 beats per minute, referred to as tachycardia and bradycardia, respectively. Changes in the rate of the pulse, along with changes in respiration is called sinus arrhythmia. In sinus arrhythmia, the pulse rate becomes faster during inspiration and slows down during expiration.
- Rhythm:
- Assessing whether the rhythm of the pulse is regular or irregular is essential. The pulse could be regular, irregular, or irregularly irregular. Irregularly irregular pattern is more commonly indicative of processes like atrial flutter or atrial fibrillation.
- Volume:
- Assessing the volume of the pulse is equally essential. A low volume pulse could be indicative of inadequate tissue perfusion; this can be a crucial indicator of indirect prediction of the systolic blood pressure of the patient.
- Symmetry:
- Checking for symmetry of the pulses is important as asymmetrical pulses could be seen in conditions like aortic dissection, aortic coarctation, Takayasu arteritis, and subclavian steal syndrome.
- Amplitude and Rate of Increase:
- Low amplitude and low rate of increase could be seen in conditions like aortic stenosis, besides weak perfusion states. High amplitude and rapid rise can be indicative of conditions like aortic regurgitation, mitral regurgitation, and hypertrophic cardiomyopathy.<ref name=":0">Sapra A, Malik A, Bhandari P. Vital Sign Assessment. InStatPearls [Internet] 2019 Dec 28. StatPearls Publishing.
Blood Pressure[edit | edit source]
Blood pressure is the force of circulating blood on the walls of the arteries, mainly in large arteries of the systemic circulation. Blood pressure incorporates two measurements:
- Systolic Pressure
- Describes the maximum pressure in the large arteries when the heart contracts to propel blood through the body.
- Measured when the heart beats
- Diastolic Pressure
- Describes the lowest pressure within the large arteries when the heart relaxes between beats.
- Measured between heart beats.
Blood pressure is traditionally assessed using auscultation with a mercury-tube sphygmomanometer measured in millimeters of mercury and expressed in terms of systolic pressure over diastolic pressure e.g. 120/60.[17] However, semiautomated and automated devices that use the oscillometry method, which detects the amplitude of the blood pressure oscillations on the arterial wall, have become widely used in daily clinical practice. The brachial artery is the most common site for BP measurement.
| Reduce Accuracy | Systolic | Diastolic |
|---|---|---|
| Hypotension | <90 | <60 |
| Normal | 90 - 129 | 60 - 79 |
| Hypertension; Stage 1 | 130 - 139 | 80 - 89 |
| Hyoertension: Stage 2 | 140 - 179 | 90 - 109 |
| Hypertension: Critical | >180 | >110 |
Respiratory Status[edit | edit source]
Work of breathing is the amount of energy or O2 consumption needed by the respiratory muscles to produce enough ventilation and respiration to meet the metabolic demands of the body.
Respiratory Rate[edit | edit source]
The respiratory rate, which is the number of breaths per minute, is defined as the one breath to each movement of air in and out of the lungs. The normal breathing rate is about 12 to 20 beats per minute in an average adult. In paediatrics age group, the respiratory rate is dependant on the age of the child.
- Rates:
- Rates higher or lower than expected are termed as tachypnea and bradypnea, respectively. Tachypnea described as a respiratory rate more than 20 beats per minute could occur in physiological conditions like exercise, emotional changes, pregnancy, and pathological conditions like pain, pneumonia, pulmonary embolism, asthma, etc. Bradypnea which is ventilation less than 12 breaths/minute can occur due to worsening of any underlying respiratory condition leading to respiratory failure or due to usage of central nervous system depressants like alcohol, narcotics, benzodiazepines, or metabolic derangements. Apnea is the complete cessation of airflow to the lungs for a total of 15 seconds which may appear in cardiopulmonary arrests, airway obstructions, the overdose of narcotics and benzodiazepines.
- Depth of Breathing:
- Hyperpnea is described as an increase in the depth of breathing. Hyperventilation, on the other hand, is described as both an increase in the rate and depth of breathing and hypoventilation describes the decreased rate and depth of ventilation. Depth of breathing involves what muscle groups they are using—for example, the sternocleidomastoid (accessory muscles) and abdominal muscles—the movement of the chest wall in terms of symmetry. The inability to speak in full sentences or increased effort to speak is an indicator of discomfort when breathing.[18]
Oxygen Saturation[edit | edit source]
Oxygen saturation is a crucial measure of how well the lungs are working, and is considered an essential element to assess and monitor a patient for positioning, transferring or mobilising. The term oxygen saturation refers to the percentage of oxygen circulating in an individuals blood.
Pulse oximetry is a painless, noninvasive method of measuring the saturation of oxygen (SpO2) in a person’s blood.[19] Most pulse oximeters are accurate to within 2% to 4% of the actual blood oxygen saturation level, which means that a pulse oximeter reading may be anywhere from 2% to 4% higher or lower than the actual oxygen level in arterial blood, in oarticulalr when oxygen saturation is below 90%.[20] For example, a 92% oxygen saturation on the pulse oximeter can actually be between 88 to 96% depending on the accuracy of the specific pulse oximeter.[3]
| Reduce Accuracy | Increase Accuracy |
|---|---|
| Cold Hands | Warm Up Skin |
| Poor Circulation or Low Perfusion State | Apply Topical Vasodilator |
| Wearing Artifical Nails | Hand Below Level of Heart |
Wearing Nail Polish
|
Probe Location
|
Very Low Oxygen Saturation
|
Probe Type
|
Skin Pigment
|
Probe Size
|
| Skin Thickness | |
| Anaemia | |
Motion Artefact
|
|
| Intravascular Dyes | |
| Smoking |
Breathing Pattern[edit | edit source]
There are many conditions which are based on the variation in the pattern of breathing. Biot’s respiration is a condition where there are periods of increased rate and depth of breathing, followed by periods of no breathing or apnea. Cheyne-Stokes respiration is a peculiar pattern of breathing where there is an increase in the depth of ventilation followed by periods of no breathing or apnea. Kussmaul’s breathing refers to the increased depth of ventilation, although the rate remains regular. Orthopnea refers to difficulty in respiration occurring on lying horizontal but gets better when the patient sits up or stands. Paradoxical ventilation refers to the inward movement of the abdominal or chest wall during inspiration, and outward movement during expiration, which is seen in cases of diaphragmatic paralysis, muscle fatigue, trauma to the chest wall.[23]
Pain[edit | edit source]
Determining pain is an important component of any assessment prior to moving a patient. When assessing pain, it is important to recognise the differences between acute and persistent pain and the implications for assessment and management of the patient. Pain is a subjective experience, and self-report of pain is the most reliable indicator of a patient’s experience. Always assess pain at the beginning of any physical assessment to determine the patient’s comfort level and potential need for pain comfort measures prior to moving the patient.
Medication[edit | edit source]
In the older person in particular, medications are among one of the most common cause of increased falls risk so as rehabilitation professionals it is important to be aware of medications that our patients are taking, as these can impact on on our patients safety during manual handling tasks. While medication management is not the role of most rehabilitation professionals, understanding what the potential impact of some medications can be very valuable. Planning assessment and rehabilitation interventions around medication, where interventions involving manual handling should be timed to coincide with medication peak effectiveness where applicable.[24]
The following classes of drugs in particular can increase risks of falls as they can affect the brain, heart and circulatory system;
- Drugs Acting on the Central Nervous System e.g. Psychotrophic Drugs
- Drugs or other substance that affects how the brain works that can cause changes in mood, thoughts, perception, behaviour, levels of alertness, altered reflexes, altered reaction times, altered muscle tone, balance etc.
- Drugs Acting on the Heart and Circulatory System
- Drugs that are used to treat different heart disorders (such as congestive heart failure, angina, or arrhythmia) or diseases of the vascular system (e.g., hypertension) can cause hypotension, orthostaic hypotension, syncope, bradycardia, muscle weakness or muscle spasms secondary to hyponatermia
- Drugs Acting on Glycemic Control
- Hypoglycemia and hyperglycemia have been correlated with an increased risk for falls in the hospitalised population.
Attachments[edit | edit source]
Environment[edit | edit source]
Resources[edit | edit source]
References [edit | edit source]
- ↑ Business Dictionary. Definition of communication. Accessed from http://www.businessdictionary.com/definition/communication.htmlon 13 August 2019
- ↑ Mata, Á.N.D.S., de Azevedo, K.P.M., Braga, L.P., de Medeiros, G.C.B.S., de Oliveira Segundo, V.H., Bezerra, I.N.M., Pimenta, I.D.S.F., Nicolás, I.M. and Piuvezam, G., 2021. Training in communication skills for self-efficacy of health professionals: a systematic review. Human resources for health, 19(1), pp.1-9.
- ↑ 3.0 3.1 Iversen ED, Wolderslund MO, Kofoed PE, Gulbrandsen P, Poulsen H, Cold S et al. Codebook for rating clinical communication skills based on the Calgary-Cambridge Guide. BMC Med Educ. 2020;20(1):140. Cite error: Invalid
<ref>tag; name ":4" defined multiple times with different content - ↑ Cannity KM, Banerjee SC, Hichenberg S, Leon-Nastasi AD, Howell F, Coyle N, Zaider T, Parker PA. Acceptability and efficacy of a communication skills training for nursing students: Building empathy and discussing complex situations. Nurse Education in Practice. 2021 Jan 1;50:102928.
- ↑ Al-Kalaldeh M, Amro N, Qtait M, Alwawi A. Barriers to effective nurse-patient communication in the emergency department. Emerg Nurse. 2020;28(3):29-35.
- ↑ 6.0 6.1 Cite error: Invalid
<ref>tag; no text was provided for refs named:02 - ↑ Amoah VMK, Anokye R, Boakye DS, Gyamfi N, Lee A (Reviewing Editor). Perceived barriers to effective therapeutic communication among nurses and patients at Kumasi South Hospital, Cogent Medicine. 2018;5:1.
- ↑ Albahri AH, Abushibs AS, Abushibs NS. Barriers to effective communication between family physicians and patients in walk-in centre setting in Dubai: a cross-sectional survey. BMC Health Serv Res. 2018;18(1):637.
- ↑ Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med 2013; 369(14):1306-16.
- ↑ Fruth SJ. Fundamentals of the Physical Therapy Examination: Patient Interview and Test & Measures. 2nd Ed. Burlington: Jones & Bartlett Learning, 2018.
- ↑ Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, Tesoro EP, Elswick RK. The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients. American journal of respiratory and critical care medicine. 2002 Nov 15;166(10):1338-44.
- ↑ Green M, Marzano V, Leditschke IA, Mitchell I, Bissett B. Mobilization of intensive care patients: a multidisciplinary practical guide for clinicians. J Multidiscip Healthc 2016; 25(9): 247-56.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs named:2 - ↑ Folstein MF, Folstein SE, McHugh PR "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov; 12(3):189-98.
- ↑ Sleutjes DK, Harmsen IJ, van Bergen FS, Oosterman JM, Dautzenberg PL, Kessels RP. Validity of the Mini-Mental State Examination-2 in Diagnosing Mild Cognitive Impairment and Dementia in Patients Visiting an Outpatient Clinic in the Netherlands. Alzheimer disease and associated disorders. 2020 Jul;34(3):278.
- ↑ Faber RA. The neuropsychiatric mental status examination. Semin Neurol. 2009;29(3):185–193. Level of evidence C
- ↑ https://www.cancer.gov/publications/dictionaries/cancer-terms/def/blood-pressure
- ↑ Rolfe S. The importance of respiratory rate monitoring. British Journal of Nursing. 2019 Apr 25;28(8):504-8.
- ↑ Hafen B, Sharma S. Oxygen Saturation. [Updated 2021 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan- [cited 2022 Oct 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525974/
- ↑ Jubran A. Pulse Oximetry. Critical Care. 1999 Apr;3:1-7.
- ↑ Hafen B, Sharma S. Oxygen Saturation. [Updated 2021 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan- [cited 2022 Oct 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525974/
- ↑ American Thoracic Society. Pulse-oximetry. Available from pulse-oximetry.pdf (thoracic.org) (accessed 15 October 2022).
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs named:0 - ↑ Stiller K. Safety issues that should be considered when mobilizing critically ill patients. Critical care clinics. 2007 Jan 1;23(1):35-53.