Assessing Muscle Strength
Original Editors - Naomi O'Reilly and Wanda van Niekerk
Top Contributors - Naomi O'Reilly, Wanda van Niekerk, Jess Bell, Lenie Jacobs, Kim Jackson and Angeliki Chorti
Introduction[edit | edit source]
Muscle strength is defined as the maximal force a muscle or muscle group can generate at a specified or determined velocity.[1] Essentially, it is the ability of skeletal muscle to develop force in order to provide stability and mobility within the musculoskeletal system, which is necessary for functional movement to occur.[2] The muscle strength assessment is integral to the objective examination as it provides valuable information on strength and neurological deficits.
Muscle strength decreases with age and many pathologies can reduce muscle strength and control.[2] For example, it can be impaired following injury, infection, major surgery or in many medical conditions including but not limited to stroke, cerebral palsy, muscular dystrophy, metabolic syndromes, spinal cord injury, motor neuron disease, multiple sclerosis, Parkinson's, COPD, heart failure, and arthritis. Muscle strength can be a predictor of mortality, hospital length of stay, and hospital readmission.
Factors Determining Muscle Strength[edit | edit source]
Strength depends on a combination of morphological and neural factors including:[3]
- cross-sectional area of muscle
- muscle architecture
- stiffness of the musculotendinous structure
- type of muscle contraction
- motor unit recruitment, rate coding and motor unit synchronisation
- neuromuscular inhibition
- speed of contraction
Some of these factors will be discussed in more detail below.
Types of Muscle Contraction[edit | edit source]
A muscle contraction occurs when tension-generating sites within the muscle cells are activated. The type of contraction is defined by changes in the length of the muscle during contraction.
Isometric Contractions[edit | edit source]
Greek, isos: “equal” and metron: “measure”
- Isometric contractions are a static contraction with variable / accommodating resistance that does not result in changes in muscle length.[4] Tension is generated in the muscle but the distance between the muscle attachments remains the same. In an isometric contraction, cross bridges form, disengage and reform. There is no movement and no external work is done by the muscle.
Please note that "cross bridge" refers to the attachment between the myosin and actin filaments.[5] Read more about cross bridges and the sliding filament theory: Sarcomere.
Isotonic Contractions[edit | edit source]
Greek, isos: “equal” and tonos: “straining”)
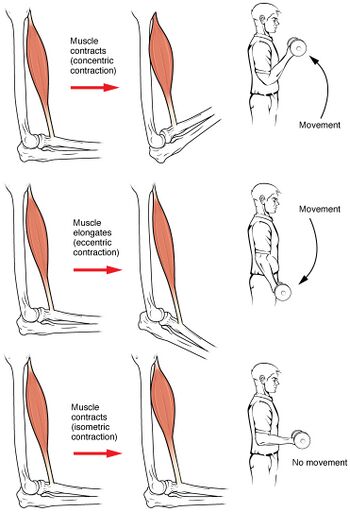
In an isotonic contraction, tension remains the same, but the muscle's length changes. There are two types of isotonic contractions: concentric and eccentric contractions.
Concentric Contraction
- During a concentric contraction, there is a shortening of the muscle,[7] so the origin and insertion of the muscle move closer together.
- A muscle performs a concentric contraction when it lifts a load or weight that is less than the maximum tetanic tension it can generate.
- The muscle shortens, movement occurs and external work is done.
Eccentric Contraction
- During an eccentric contraction, the muscle lengthens as it gives in to an external force that is greater than the contractile force exerted by the muscle.[8][9]
- In reality, the muscle does not lengthen. Instead, it returns from its shortened position to its normal length.
- The muscle lengthens, movement occurs and external work is done.
Length of Muscle[edit | edit source]
Muscle length is an important factor in governing force and tension. The full range in which a muscle can work = the range between the position of maximal stretch to the position of maximal shortening. As shown in Table 1, full range is divided into three parts.[10]
| Outer Range | Inner Range | Mid Range |
|---|---|---|
Muscle Fibre Type[edit | edit source]
- There are three types of muscle fibres.
- These can be classified based on how fast the fibres contract relative to other fibres and how the fibres regenerate adenosine triphosphate (ATP) (i.e. the source of energy for muscles).
- Muscle fibre type can also be influenced by training.
| Type I / Slow Twitch / Slow Oxidative | Type IIa / Fast Twitch / Oxidative-Glycolytic | Type IIb / Fast Twitch /
Glycolytic |
|---|---|---|
|
|
|
Read more: Muscle Fibre Types, Sliding Filament Model of Contraction, The Muscle Contraction Process
Neural Factors[edit | edit source]
- Neural factors influence the tension-developing capacity of the muscle, which determines the extent to which a muscle is activated.
- Tension are influenced by neural input through two mechanisms[14]:
- Motor unit recruitment
- Modification of the firing frequency of motor units
Integrity of Connective Tissue[edit | edit source]
- For a person to intentionally contract a muscle, they must generate a signal in their brain. This signal travels from the brain, through nerve cells in the brain stem and spinal cord to the peripheral nerves and to the muscle.
- Certain factors can impact the integrity of connective tissues at any part of this pathway, and this is evident in force production and overall muscle strength.
- Pain has been shown to impact the production of muscle force. It results in a reduction in maximal voluntary contraction and endurance time during submaximal contractions.[15]
- There is also correlation between pain intensity and reduced muscle strength in individuals with chronic pain, with increased pain intensity resulting in decreased muscle strength and force production.[16]
- Similarly, inflammation can impact force production, with research suggesting higher levels of circulating inflammatory markers are significantly associated with lower skeletal muscle strength and mass.[17]
- Many diseases, including neuromuscular diseases, cancer, chronic inflammatory diseases, and acute critical illness are associated with skeletal muscle atrophy, muscle weakness, and general muscle fatigue, which is associated with increased morbidity and mortality and decreased quality of life.[18]
Age[edit | edit source]
- Ageing effects all body organs and systems in the skeletal muscle.
- As we age, our muscles undergo progressive changes. These primarily result in loss of muscle mass and strength. Muscle mass decreases approximately 3–8% per decade after the age of 30 and this rate of decline is even higher after the age of 60.[19][20]
- The total number of muscle fibres reduces with age, beginning at around 25 years and progressing at an accelerated rate thereafter. This leads to reduced muscle cross-sectional area and reduced muscle power.[21]
- There is also a decrease in the number of functional motor units[22] - this is associated with an enlargement of remaining motor units (these remaining units also experience "reduced neuromuscular junction transmission stability".[23]
- Overall, these changes in the muscle mass, muscle fibre and cross sectional area of the muscle during the ageing process are important clinically as they lead to reduced muscle strength.
Read more: Muscle Function: Effects of Ageing
Contraindications[edit | edit source]
Muscle strength assessments are typically contraindicated when a muscle contraction or motion of the tested part of the body could disrupt the healing process, cause injury or worsen the condition.[10] Some instances where a muscle strength assessment may be contraindicated include[10]:
- Unhealed fracture
- Dislocation or unstable joint
- Active range of motion or resistance work are contraindicated (e.g. post-operative protocols etc)
- Pain limits participation
- Severe inflammation
- Severe osteoporosis
- Haemophilia
- Cognitive concerns / decreased ability to complete the test
Precautions[edit | edit source]
During a muscle strength assessment, ensure you respect pain and consider patient comfort. Specific precautions include:
- Abdominal surgery or hernia[10]
- Bony ankylosis
- Haematoma
- Cardiovascular or pulmonary disease[10]
- Prolonged immobilisation
- Extreme debility[10]
Measuring Muscle Strength[edit | edit source]
Muscle strength testing is used to determine the capability of the muscle or muscle group to produce force. It provides information that is useful in differential diagnosis, prognosis and management of neuromuscular and musculoskeletal disorders.[24] While there are many methods of assessing muscle strength, there are three key approaches described in the literature and used clinically (see Table 3): isokinetic, isotonic, and isometric testing.
| Isotonic | Isokinetic | Isometric |
|---|---|---|
|
|
|
Manual Muscle Testing (MMT)[edit | edit source]
- Manual muscle testing helps to determine the extent and degree of muscle weakness resulting from disease, injury or disuse to provide a basis for planning therapeutic procedures.
- It is used to evaluate the function and strength of an individual muscle or muscle group, based on the effective performance of a movement in relation to the forces of gravity or manual resistance through the available range of motion.[10]
- There are a wide range of scales available for completing manual muscle testing including:
- Modified Medical Research Council (MRC) Scale - also known as the Oxford Scale
- Daniels and Worthinghmans Manual Muscle Testing Scale
- Kendall Muscle Testing Scale
- Note that some scales use tests based on actions (e.g. elbow flexion) rather than tests of individual muscles (e.g. biceps brachii). In these cases, the grade will represent the performance of all muscles contributing to the specific action.
| Grade | Description |
|---|---|
| 0 | No contraction |
| 1 | Flickering contraction |
| 2 | Full range of motion with gravity eliminated |
| 3 | Full range of motion against gravity |
| 4 | Full range of motion against gravity with minimal resistance |
| 5 | Full range of motion against gravity with maximal resistance |
As per Daniels and Worthington's 'Muscle Testing: Techniques of Manual Examination and Performance Testing', there are two different methods used for manual muscle testing[27]:
- Break Test: resistance is applied to the body part at the end of the available range of motion. It is called the break test because the patient is trying to stop the therapist from "breaking" the muscle hold when resistance is applied.
- Active Resistance Test: resistance is applied to the body part through the available range of motion. This type of manual muscle testing requires skill and experience and is not the recommended practice.
Dynamometry[edit | edit source]
Dynamometry is a more precise and objective measurement of the force that a muscle can exert. It allows the assessor to compare strength on each side and measures strength changes during a rehabilitation programme. It typically uses the same positioning as manual muscle testing but provides more quantifiable data.[28]
Benefits of dynamometry:
- more sensitive than manual muscle testing
- norms available
Principles of Assessment[edit | edit source]
Some overall guiding principles when assessing muscle strength are as follows[29][30]:
- Compare the unaffected side with the affected side:
- Where possible, assess the unaffected limb's active range of motion first
- This shows the patient's willingness to move and provides a baseline for normal movement of the joint being tested
- It also shows the patient what to expect, which increases patient confidence and reduces apprehension when testing the affected side.
- Where possible, assess the unaffected limb's active range of motion first
- Any movements that are painful should be completed last. This helps to minimise the risk of overflow of painful symptoms to the next movement.[29][30]
- Preparation:
- Determine whether there are contraindications or precautions and what joints, muscles and motions need to be tested.[10]
- Organise the testing sequence by body position to minimise changes in positioning.
- Communication:
- Briefly explain the procedure for manual muscle testing to the patient.[2]
- Explain and demonstrate the movement to be performed and/or passively move the patient’s limb through the test movement.[2]
- Explain and demonstrate the examiner’s and patient's roles and confirm the patient understands and is willing to participate.[2]
- Expose the Area
- Explain and demonstrate anatomical landmarks and why they need to be exposed.
- Adequately expose the area and drape the patient as required.
- Positioning
- Proper positioning of the patient during muscle testing is essential in ensuring that the appropriate muscle is being tested. It also helps prevent substitution by other muscles.[2]
- Aim to isolate the action of a specific muscle to minimise the influence of other muscles when testing
- Place the body part that the muscle acts on in the starting position.
- As a rule, this will typically be in the mid-range of the muscle, so it can produce maximum force during the test.
- If there is any variance to the patient's position from standard assessment position outlined in our technique videos, ensure you make a note of this in your documentation.
- For example, if a patient cannot achieve full elbow extension, record the starting angle before measuring the elbow flexion strength.
- Tables 5 and 6 provide information on patient positioning for testing:
| Body Region | Muscle Action | Patient Position in Relation to Grade Being Tested | ||
|---|---|---|---|---|
| Grade 0 and 1 | Grade 2 | Grade 3, 4 and 5 | ||
| Shoulder | Extension | Prone | Side Lying | Prone |
| Flexion | Supine | Side Lying | Supine | |
| Abduction | Supine | Supine | Side Lying or Standing | |
| Adduction | Supine | Supine | Side Lying or Standing | |
| External Rotation | Prone | Supine | Sitting - Hips and Knees at 90° | |
| Internal Rotation | Supine | Supine | Sitting - Hips and Knees at 90° | |
| Elbow | Extension | Prone | Side Lying or Sitting | Prone or Sitting |
| Flexion | Supine | Side Lying or Sitting | Supine or Sitting | |
| Supination | Supine or Sitting | Difficult to eliminate gravity in FROM | Supine or Sitting
Grade 3 - Difficult to complete FROM against gravity | |
| Pronation | Supine or Sitting | Difficult to eliminate gravity in FROM | Supine or Sitting
Grade 3 - Difficult to complete FROM against gravity | |
| Wrist | Extension | Supine or Sitting | Supine or Sitting
Forearm in Mid Position |
Supine or Sitting
Forearm Pronated |
| Flexion | Supine or Sitting | Supine or Sitting
Forearm in Mid Position |
Supine or Sitting
Forearm Supinated | |
| Ulnar Deviation | Supine or Sitting | Supine or Sitting
Forearm Pronated |
Supine or Sitting
Forearm Pronated | |
| Radial Deviation | Supine or Sitting | Supine or Sitting
Forearm Pronated |
Supine or Sitting
Forearm in Mid Position | |
| Body Region | Muscle Action | Patient Position in Relation to Grade Being Tested | ||
|---|---|---|---|---|
| Grade 0 and 1 | Grade 2 | Grade 3, 4 and 5 | ||
| Hip | Extension | Prone | Side Lying | Prone |
| Flexion | Supine | Side Lying | Supine | |
| Abduction | Supine | Supine | Side Lying or Standing | |
| Adduction | Supine | Supine | Side Lying or Standing | |
| External Rotation | Prone | Supine | Sitting - Hips and Knees at 90° | |
| Internal Rotation | Supine | Supine | Sitting - Hips and Knees at 90° | |
| Knee | Extension | Supine | Side Lying | Sitting |
| Flexion | Prone | Side Lying | Prone or Standing | |
| Ankle | Plantarflexion | Prone | Side Lying | Prone or Standing |
| Dorsiflexion | Supine | Side Lying | Supine or Sitting | |
| Eversion | Supine | Supine | Side Lying | |
| Inversion | Supine | Supine | Side Lying | |
- Stabilisation[27]
- The patient’s body needs to be placed in a stable position - the joint that the muscle acts on must be firmly fixed in place.
- Stabilisation comes initially from the effect of gravity and the weight of the patient on the treatment table or chair.
- Hand placement of the rehabilitation professionals on the limb to be assessed offers additional stabilisation of the proximal joints while the resistance is placed distally.
- Substitute movements at other joints may occur without adequate stabilisation, which can affect results.
- Rehabilitation professionals should know and recognise the possible substitute movements at each joint they are assessing to increase accuracy.
- Application of Resistance[27]
- Apply resistance at the end of the range in one-joint muscles. This allows for consistency in procedure.
- Two-joint muscles should be tested in mid-range. Length tension is more favourable in this range.
- Aim to test muscles and muscle groups at optimal length-tension. However there are situations where a rehabilitation professional will not be able to distinguish between Grade 5 and 4 without putting the patient at a mechanical disadvantage.
- Ensure to apply resistance slowly and gradually at the distal end of the limb with pressure opposite the line of pull of the muscle to be tested. Typically a lumbrical grip is most comfortable for the patient.
- Application of Grades
- Always start with testing in a position against gravity (Grade 3 in MRC Scale) to determine if the patient can move through the full range of motion against gravity ensuring to isolate muscle or muscle group to be tested.
- If the patient cannot move through any part of the range of motion against gravity, re-position the patient so that the resistance of gravity is eliminated for the test movement (i.e., the patient performs the movement in the horizontal plane).
- In this case, it may be necessary to support the weight of the limb on a relatively friction-free surface or manually.[2]
- Documentation
- Documentation of manual muscle testing should list[10]:
- the muscle being tested
- muscle grade allocated
- symptoms experienced that may have impacted on strength
- changes needed to positioning to complete the test. e.g. right quadriceps 4/5 with pain performed in supine.
- Documentation of manual muscle testing should list[10]:
Clinical Significance[edit | edit source]
Muscle strength testing can help be utilised to determine if there is a loss in muscle strength. Careful and consistent technique is important to ensure valid and reproducible results. Understanding the factors that may impact on muscle strength are also important in order to clinically reason why the person is experiencing loss of strength. Manual muscle testing with the Oxford Scale is the most commonly used grading scale, which is quick to complete and does not require special equipment, and while it is a subjective measure it demonstrates reasonable inter-rater reliability. More precise methods of measurement, such as dynamometry, are less subjective and provide a quantifiable measurement that can be tracked over time, but can be more time consuming to complete and require access to more expensive equipment.
Summary[edit | edit source]
Consistency in techniques is important for valid and reliable results. Having a good understanding of the factors that influence muscle strength will enhance your clinical reasoning skills. Manual muscle testing is quick to complete, does not require special equipment and exhibits reasonable inter-rater reliability. However, it is a clinical skill that needs to be practised on a variety of patients to acquire the necessary skills and experience.
References [edit | edit source]
- ↑ Knuttgen HG, Kraemer WJ. Terminology and measurement. Journal of applied sport science research. 1987;1(1):1-0.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Berryman Reece, N. Muscle and Sensory Testing. Fourth Edition. St Louis, Missouri. Elsevier. 2021
- ↑ Suchomel TJ, Nimphius S, Bellon CR, Stone MH. The importance of muscular strength: training considerations. Sports medicine. 2018 Apr;48:765-85..
- ↑ Rivera-Brown AM, Frontera MD. Principles of exercise physiology: Responses to acute exercise and long-term adaptations to training. PM&R. 2012; 4: 797-804.
- ↑ Cross-bridge Theory. In: Binder MD, Hirokawa N, Windhorst U, editors. Encyclopedia of Neuroscience. Berlin, Heidelberg: Springer, 2009.
- ↑ OpenStax. Anatomy and Physiology Chapter. 10.4 Nervous System Control of Muscle Tension. Available from: https://openstax.org/books/anatomy-and-physiology/pages/10-4-nervous-system-control-of-muscle-tension#fig-ch10_04_01(accessed 23 March 2023).
- ↑ Yoshida R, Kasahara K, Murakami Y, Sato S, Nosaka K, Nakamura M. Less fatiguability in eccentric than concentric repetitive maximal muscle contractions. European Journal of Applied Physiology. 2023 Mar 19:1-3.
- ↑ Tomalka A. Eccentric muscle contractions: from single muscle fibre to whole muscle mechanics. Pflügers Archiv-European Journal of Physiology. 2023 Apr;475(4):421-35.
- ↑ Douglas J, Pearson S, Ross A, McGuigan M. Eccentric exercise: physiological characteristics and acute responses. Sports Medicine. 2017 Apr;47:663-75.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 Clarkson HM. Musculoskeletal assessment: joint range of motion and manual muscle strength. Lippincott Williams & Wilkins; 2013
- ↑ 11.0 11.1 11.2 Nishikawa KC, Monroy JA, Tahir U. Muscle function from organisms to molecules. Integrative and comparative biology. 2018 Aug 1;58(2):194-206.
- ↑ 12.0 12.1 Plotkin DL, Roberts MD, Haun CT, Schoenfeld BJ. Muscle fiber type transitions with exercise training: Shifting perspectives. Sports. 2021 Sep 10;9(9):127.
- ↑ Biga LM, Bronson S, Dawson S, Harwell A, Hopkins R, Kaufmann J, LeMaster M, Matern P, Morrison-Graham K, Oja K, Quick D, Runyeon J. Anatomy and Physiology. Openstax. Available from https://open.oregonstate.education/aandp/chapter/10-5-types-of-muscle-fibers/
- ↑ Bohannon RW. Contribution of neural and muscular factors to the short duration tension-developing capacity of skeletal muscle. Journal of Orthopaedic & Sports Physical Therapy. 1983 Nov 1;5(3):139-47.
- ↑ Graven-Nielsen T, Arendt-Nielsen L. Impact of clinical and experimental pain on muscle strength and activity. Current rheumatology reports. 2008 Dec;10(6):475-81.
- ↑ Van Wilgen CP, Akkerman L, Wieringa J, Dijkstra PU. Muscle strength in patients with chronic pain. Clinical rehabilitation. 2003 Dec;17(8):885-9.
- ↑ Tuttle CS, Thang LA, Maier AB. Markers of inflammation and their association with muscle strength and mass: A systematic review and meta-analysis. Ageing research reviews. 2020 Dec 1;64:101185.
- ↑ Powers SK, Lynch GS, Murphy KT, Reid MB, Zijdewind I. Disease-induced skeletal muscle atrophy and fatigue. Medicine and science in sports and exercise. 2016 Nov;48(11):2307.
- ↑ Melton LJ. Khosla S, Crowson CS, O'Connor MK, O'Fallon WM, and Riggs BL. Epidemiology of sarcopenia. J Am Geriatr Soc. 2000;48:625-30.
- ↑ Volpi E, Nazemi R, Fujita S. Muscle tissue changes with aging. Current opinion in clinical nutrition and metabolic care. 2004 Jul;7(4):405.
- ↑ Henwood TR, Riek S, Taaffe DR. Strength versus muscle power-specific resistance training in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2008; 63(1):83-91.
- ↑ Bunn JA. Aging and the Motor Unit. J Sport Medic Doping Studie. 2012; S1:e001. doi:10.4172/2161-0673.S1-e001
- ↑ Piasecki M, Ireland A, Coulson J, Stashuk DW, Hamilton-Wright A, Swiecicka A, et al. Motor unit number estimates and neuromuscular transmission in the tibialis anterior of master athletes: evidence that athletic older people are not spared from age-related motor unit remodeling. Physiol Rep. 2016 Oct;4(19):e12987.
- ↑ Kendall FP, Kendall McCreary E, Geise Provance P, McIntyre Rodgers M and Romani WA. Muscles Testing and Function with Posture and Pain - Fifth Edition. Philadelphia: Lippincott Williams and Wilkins, 2005.
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 25.6 Cannavan D, Butte KT. 3.9 Strength testing. Sport and Exercise Physiology Testing Guidelines: Volume I-Sport Testing: The British Association of Sport and Exercise Sciences Guide. 2022 Mar 22:106.
- ↑ Naqvi U. Muscle strength grading. InStatPearls [Internet] 2021 Sep 2. StatPearls Publishing.
- ↑ 27.0 27.1 27.2 Avers, D. Brown, M. Daniels and Worthingham's Muscle Testing: Techniques of Manual Examination and Performance Testing. 10th Edition. St Louis, Missouri. Elsevier. 2019
- ↑ Sole G. Physical Therapy of the Shoulder. New Zealand Journal of Physiotherapy. 2004 Jul 1;32(2):87-8.
- ↑ 29.0 29.1 Reese NB, Bandy WD. Joint Range of Motion and Muscle Length Testing-E-book. Elsevier Health Sciences; 2016 Mar 31.
- ↑ 30.0 30.1 Magee D. Orthopaedic Physical Assessment WB Saunders. pg. 2002;478:483-631.






