Assessing Muscle Strength: Difference between revisions
No edit summary |
No edit summary |
||
| Line 157: | Line 157: | ||
* Requires extensive training | * Requires extensive training | ||
* Only measures isometric muscle force | * Only measures isometric muscle force | ||
== Contraindications == | |||
* Unhealed fracture | |||
* Dislocation or Unstable Joint | |||
* Active ROM or Resistance Contraindicated (e.g. Post-op Protocols etc) | |||
* Pain Limit Particpation | |||
* Severe Inflammation | |||
* Severe Osteoporosis | |||
* Haemophelia | |||
* Cognitive concerns and ability to complete test | |||
== Precautions == | |||
* Respect Pain | |||
* Patient Comfort | |||
* Abdominal Surgery or Hernia | |||
* Bony Ankylosis | |||
* Hematoma | |||
* Cardiovascular or Pulmonary disease | |||
* Prolonged Immobilisation | |||
* Extreme Debility | |||
== Principles of Measurement == | == Principles of Measurement == | ||
===== Positioning ===== | ===== Positioning ===== | ||
The main idea of the muscle test is to attempt to isolate the action of a specific muscle so that synergism from other muscles is eliminated or at least reduced to a minimum. In order to achieve this, the body part that is acted on by the muscle is put into a precise start position. As a rule, this will typically be in the mid-range of the muscle, thus allowing it to produce maximum force during the test. The following table provides information on the positioning of the patient for testing. | The main idea of the muscle test is to attempt to isolate the action of a specific muscle so that synergism from other muscles is eliminated or at least reduced to a minimum. In order to achieve this, the body part that is acted on by the muscle is put into a precise start position. As a rule, this will typically be in the mid-range of the muscle, thus allowing it to produce maximum force during the test. The following table provides information on the positioning of the patient for testing. | ||
| Line 339: | Line 359: | ||
===== Application of Grades ===== | ===== Application of Grades ===== | ||
Always start with | Always start with testing for Grade 3 to determine if the patient can move through the full range of motion against gravity ensuring to isolate muscle or muscle group to be tested | ||
===== Application of Resistance ===== | |||
Ensure to apply resistance slowly and gradually at the distal end of the limb with pressure opposite the line of pull of the muscle to be tested. | |||
===== Comparison (if applicable) ===== | ===== Comparison (if applicable) ===== | ||
Always ensure to check strength on the uninvolved side first where possible, ensuring understanding of the test and to be able to determine a baseline for force application to the affected limb. | |||
===== Objectivity ===== | ===== Objectivity ===== | ||
===== Documentation ===== | ===== Documentation ===== | ||
Documentation of manual muscle testing should list the muscle being tested, muscle grade allocated, symptoms experienced that may have impacted on strength and any changes needed to positioning to complete the test. e.g. right quadriceps 4/5 without discomfort performed in supine | |||
== Clinical Significance == | == Clinical Significance == | ||
Revision as of 16:26, 7 April 2023
Original Editors - Naomi O'Reilly and Wanda van Niekerk
Top Contributors - Naomi O'Reilly, Wanda van Niekerk, Jess Bell, Lenie Jacobs, Kim Jackson and Angeliki Chorti
Introduction[edit | edit source]
Muscle strength is the ability of skeletal muscle to develop force for the purpose of providing stability and mobility within the musculoskeletal system so that functional movement can take place. Muscle strength decreases with age in adults and can be impaired following injury, infection, post major surgery or in many medical conditions including but not limited to stroke, cerebral palsy, muscular dystrophies, metabolic syndromes, spinal cord injury, motor neuron disease, multiple sclerosis, myopathy, Parkinson's disease, chronic obstructive pulmonary disease, heart failure, peripheral arterial disease and arthritis and can be a predictor of mortality, hospital length of stay, and hospital readmission. Given this practical options for measuring muscle strength are key for rehabilitation with assessment of muscle strength typically performed as part of the objective assessment, and is an important component of the physical exam that can reveal information about strength and neurological deficits.
Factors Determining Muscle Strength[edit | edit source]
Strength depends on the combination of morphological and neural factors including muscle cross-sectional area and architecture, musculotendinous stiffness, motor unit recruitment, rate coding, motor unit synchronisation, and neuromuscular inhibition[1]
Type of Muscle Contraction[edit | edit source]
Muscle contraction is the activation of tension-generating sites within the muscle cells, and are defined by changes in the length of the muscle during contraction.
Isometric Contractions[edit | edit source]
Isometric contractions produce a static contraction with a variable and accommodating resistance without producing any appreciable change in muscle length. Tension is being generated in the muscle but the distance between the muscle attachments remains the same. In an isometric contraction the cross bridges form, disengage and reform. There is no movement and no external work is done by the muscle.
Isotonic Contractions[edit | edit source]
In an isotonic contraction, tension remains the same, whilst the muscle's length changes. There are two types of isotonic contractions: concentric and eccentric contractions.
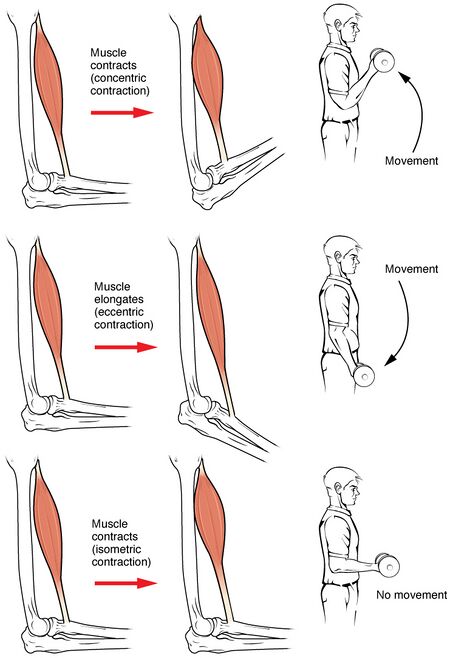
- A concentric contraction produce a shortening of the muscle such that the origin and insertion of the muscle move closer together.
- A muscle performs a concentric contraction when it lifts a load or weight that is less than the maximum tetanic tension it can generate.
- The muscle shortens, movement occurs and external work is done.
Eccentric Contraction;
- An eccentric contraction occurs when a muscle lengthens as it gives in to an external force that is greater than the contractile force it is exerting.
- In reality, the muscle does not lengthen; it merely returns from its shortened position to its normal length.
- During eccentric work cross bridges form and the myosin head swings towards the Z line, which is opposite to what happens during a concentric contraction. The overlap between the actin and myosin decreases and the sarcomere increases in length. Muscle is actively lengthening, in the direction of the force of gravity. The extrinsic forces acting on the muscle are greater than those generated intrinsically.
- The muscle lengthens, movement occurs and external work is done.
Length of Muscle[edit | edit source]
The length of a muscle is an important factor in governing the force and tension it can generate. The full range in which a muscle can work refers to the muscle changing from a position of maximal stretch to contracting to a position of maximal shortening. The full range is divided into three parts.
Muscle Working in Outer Range:
- Muscle is working in a maximally stretched position (moves between the longest length and the mid-point of range).
- Actin and myosin have least overlap, fewer cross bridges can form and so less tension is produced.
Muscle Working in Inner Range:
- Muscle is working in a maximally shortened position (moves between the shortest length and the mid-point of range).
- Actin and Myosin overlap, which decreases the number of sites available for cross bridge formation and therefore less force is generated
Muscle Working in Mid Range:
- Muscle is working between between the mid point of the outer range and the midpoint of the inner range (muscle changes length from the middle positions of outer and middle ranges).
- Actin and Myosin filaments have optimal overlap, which provides the optimum number of sites for cross bridge formation, and therefore maximum tension is generated in this range.
Muscle Fibre Type[edit | edit source]
There are three types of muscle fibres, which can be classified based on how fast the fibres contract relative to other fibres and how the fibres regenerate adenosine triphosphate (ATP), which is muscles source of energy. Each muscle will contains a mix of these muscle fibres with wide variations in their exact composition, based on genetics and the main function of muscle, which can be influenced by training. People who do well at endurance sports tend to have a higher number of slow-twitch fibres, whereas people who are better at sprint events tend to have higher numbers of fast-twitch muscle fibres.
Type I Slow Twitch Oxidative
- Slow oxidative fibres contract relatively slowly and use aerobic respiration (oxygen and glucose) to produce ATP.
- They produce low power contractions over long periods and are slow to fatigue.
- High aerobic capacity, efficient at working isometrically.
- Generally Deep, Penniform, Cross One Joint - Extension, Abduction, External Rotation
Type IIa Fast Twitch Oxidative-Glycolytic
- Fast oxidative fibres have fast contractions and primarily use aerobic respiration.
- Respond quicker than Type I but fatigue more quickly because they may switch to anaerobic respiration (glycolysis).
Type IIb Fast Twitch Glycolytic
- Fast glycolytic fibres have fast contractions and primarily use anaerobic glycolysis.
- Quickest response but fatigue rapidly and have a relatively slow recovery rate.
- Generally Superficial, Parallel - Flexion, Adduction, Internal Rotation.
Speed of Contraction[edit | edit source]
The speed of muscle contraction is dependent on how quickly myosin’s ATPase hydrolyses ATP to produce cross-bridge action. Fast fibres hydrolyse ATP approximately twice as quickly as slow fibres, resulting in much quicker cross-bridge cycling, which pulls the thin filaments toward the center of the sarcomeres at a faster rate.
Cross Sectional Area of Muscle[edit | edit source]
The greater the cross sectional area of the muscle the greater the force a muscle can produce. The cross sectional area is proportional to the force that is produces with force independent of fibre length. The only forces transmitted though the muscle attachments are those generated by the sarcomeres at the end of the muscle. In a pennate structure more fibres can be packed in and so they tend to be stronger and have a greater cross sectional area.
Neural Factors[edit | edit source]
Neural factors influence the tension-developing capacity of the muscle, which determines the extent to which a muscle is activated. Neural input influences the tension and EMG of skeletal muscle by two mechanisms; the recruitment of motor units and the modification of the firing frequency of motor units. [3] Each muscle fibres generates a force so small as to be impractical for even the most delicate movement. Therefore the system is designed such that a group of muscle fibres share common innervation from a single alpha motor neuron with the amount of force generated based on the number of motor units recruited and the firing frequency of the motor units.
Motor Unit Recruitment - Hennemann Size Principle
- The force generated can be increased by activating more motor units and this is termed motor unit recruitment. The smaller motor units have the most excitable motor neurones and therefore are recruited first. As more force is required the larger and progressively less excitable motor neurones are recruited in an orderly fashion. This has become known as the Hennemann Size Principle.
Rate Coding - Firing Frequency of Motor Units
- Rate Coding is a term used to describe the firing frequency or discharge rates of motor units. The force of active motor units can also be varied by the frequency of stimulation of the motor neurone and by utilising the force frequency characteristics. Motor units alter firing rates.
- The fibres belonging to a motor unit may be scattered throughout a muscle thus adjacent muscle fibres are unlikely to belong to the same motor unit. A muscle fibre will contract when the nerve stimulus is of sufficient intensity to release calcium. This is called threshold stimulus.
- If there are less than 30 twitches per second then the fibre will contract but the cross bridges will detach before the next stimulus. This allows the muscle to relax back to its former length.
- If the frequency of successive impulses is greater than 30 each impulse will produce the twitch of the fibre before there is time to relax. This means there is a progressive shortening of the fibre causing an increase in tension between the muscle attachments so a stronger contraction is produced. This is called a tetanic contraction.
Integrity of Connective Tissue[edit | edit source]
For a person to intentionally contract a muscle the brain must generate a signal that travels a pathway from the brain, through nerve cells in the brain stem and spinal cord to the peripheral nerves and across the connection between nerve and muscle (called a neuromuscular junction). Many factors can impact of the integrity of connective tissues at any part of this pathway, which have been shown to impact on force production and overall muscle strength. Pain has been shown to impact on the production of muscle force including a reduction in maximal voluntary contraction and endurance time during submaximal contractions.[4] There has also been shown to be a correlation between pain intensity and reduced muscle strength in individuals with chronic pain, with increased pain intensity resulting in decreased muscle strength and force production.[5] Similarly inflammation can also impact on force production, with research suggesting that higher levels of circulating inflammatory markers are significantly associated with lower skeletal muscle strength and muscle mass.[6] Many diseases including neuromuscular diseases, cancer, chronic inflammatory diseases, and acute critical illness are associated with skeletal muscle atrophy, muscle weakness, and general muscle fatigue, which is associated with increased morbidity and mortality and a decreased quality of life.[7]
Age[edit | edit source]
Aging effects all body organs and systems in the skeletal muscle. As we age our muscles undergo progressive changes, primarily involving loss of muscle mass and strength. Muscle mass decreases approximately 3–8% per decade after the age of 30 and this rate of decline is even higher after the age of 60. [8][9] Total number of muscle fibres reduces with age, beginning at about 25 years and progressing at an accelerated rate thereafter, with reduced muscle cross-sectional area and as results reduced muscle power. [10] There is also a decrease in the number of functional motor units associated with enlargement of the cross sectional area of the remaining units in the aging motor unit. [11] Overall these changes in the muscle mass, muscle fibre and cross sectional area of the muscle during the aging process is important clinically as it reduces muscle strength.
Measuring Muscle Strength[edit | edit source]
Muscle strength testing is used to determine the capability of the muscle or muscle group to function in movement and their ability to provide stability and support, and is an integral part of the physical examination. It provides information that is useful in differential diagnosis, prognosis and management of neuromuscular and musculoskeletal disorders.[12] Muscle strength can be assessed by a number of methods -manually, functionally, or mechanically.[13]
Manual Muscle Testing[edit | edit source]
Manual muscle testing helps to determine the extent and degree of muscular weakness resulting from disease, injury or disuse to provide a basis for planning therapeutic procedures and periodic re-testing. It is a procedure used to evaluate the strength of an individual muscle or muscle group, based on the performance of a movement in relation to the forces of gravity or manual resistance through the available range of motion. As per Daniels and Worthington's 'Muscle Testing: Techniques of Manual Examination and Performance Testing', there are two different methods for performing manual muscle testing.
- Break testing in manual muscle testing, is when resistance is applied to the body part at the end of the available range of motion. It's called the break test because when a therapist provides resistance the objective for the patient is to not allow the therapist to "break" the muscle hold.
- Active Resistance testing in manual muscle testing is when resistance is applied to the body part through the available range of motion. This type of manual muscle testing requires skill and experience and is not the recommended practice.
| Grade | Description |
|---|---|
| 0 | No Contraction |
| 1 | Flickering Contraction |
| 2 | Full Range of Motion with Gravity Eliminated |
| 3 | Full Range of Motion Against Gravity |
| 4 | Full Range of Motion Against Gravity with Minimal Resistance |
| 5 | Full Range of Motion Against Gravity with Maximal Resistance |
Dynamometry[edit | edit source]
Dynamometry is a more precise and objective measurement of the force that a muscle can exert and can allow for comparison across extremities or as a measure of progress in strengthening during rehabilitation. [15]
- More sensitive than MMT
- Norms available
- Requires training
- If subject is very strong the tester may not be able to hold the patient in position
Isokinetic Machines[edit | edit source]
Mechanical measurement of muscle performance
- Objective
- Quantitative
- Isometric / Concentric / Eccentric
- Muscle works at constant velocity; Isokinetic
- Resistance is variable depending on muscle ability to generate force & to keep pace with selected speed
Strain Gauges[edit | edit source]
Assess Maximum Voluntary Isometric Contraction MVIC
Advantages
- Sensitive
- Objective
- Reliable
Disadvantages
- Time consuming
- But can cover more muscle groups in less time than isokinetic testing
- Requires extensive training
- Only measures isometric muscle force
Contraindications[edit | edit source]
- Unhealed fracture
- Dislocation or Unstable Joint
- Active ROM or Resistance Contraindicated (e.g. Post-op Protocols etc)
- Pain Limit Particpation
- Severe Inflammation
- Severe Osteoporosis
- Haemophelia
- Cognitive concerns and ability to complete test
Precautions[edit | edit source]
- Respect Pain
- Patient Comfort
- Abdominal Surgery or Hernia
- Bony Ankylosis
- Hematoma
- Cardiovascular or Pulmonary disease
- Prolonged Immobilisation
- Extreme Debility
Principles of Measurement[edit | edit source]
Positioning[edit | edit source]
The main idea of the muscle test is to attempt to isolate the action of a specific muscle so that synergism from other muscles is eliminated or at least reduced to a minimum. In order to achieve this, the body part that is acted on by the muscle is put into a precise start position. As a rule, this will typically be in the mid-range of the muscle, thus allowing it to produce maximum force during the test. The following table provides information on the positioning of the patient for testing.
| Body Region | Muscle Action | Patient Position in Relation to Grade Being Tested | ||
|---|---|---|---|---|
| Grade 0 and 1 | Grade 2 | Grade 3, 4 and 5 | ||
| Shoulder | Extension | Prone | Side Lying | Prone |
| Flexion | Supine | Side Lying | Supine | |
| Abduction | Supine | Supine | Side Lying or Standing | |
| Adduction | Supine | Supine | Side Lying or Standing | |
| External Rotation | Prone | Supine | Sitting - Hips and Knees at 90° | |
| Internal Rotation | Supine | Supine | Sitting - Hips and Knees at 90° | |
| Elbow | Extension | Prone | Side Lying or Sitting | Prone or Sitting |
| Flexion | Supine | Side Lying or Sitting | Supine or Sitting | |
| Supination | Supine or Sitting | Difficult to eliminate gravity in FROM | Supine or Sitting
Grade 3 - Difficult to complete FROM against gravity | |
| Pronation | Supine or Sitting | Difficult to eliminate gravity in FROM | Supine or Sitting
Grade 3 - Difficult to complete FROM against gravity | |
| Wrist | Extension | Supine or Sitting | Supine or Sitting
Forearm in Mid Position |
Supine or Sitting
Forearm Pronated |
| Flexion | Supine or Sitting | Supine or Sitting
Forearm in Mid Position |
Supine or Sitting
Forearm Supinated | |
| Ulnar Deviation | Supine or Sitting | Supine or Sitting
Forearm Pronated |
Supine or Sitting
Forearm Pronated | |
| Radial Deviation | Supine or Sitting | Supine or Sitting
Forearm Pronated |
Supine or Sitting
Forearm in Mid Position | |
| Body Region | Muscle Action | Patient Position in Relation to Grade Being Tested | ||
|---|---|---|---|---|
| Grade 0 and 1 | Grade 2 | Grade 3, 4 and 5 | ||
| Hip | Extension | Prone | Side Lying | Prone |
| Flexion | Supine | Side Lying | Supine | |
| Abduction | Supine | Supine | Side Lying or Standing | |
| Adduction | Supine | Supine | Side Lying or Standing | |
| External Rotation | Prone | Supine | Sitting - Hips and Knees at 90° | |
| Internal Rotation | Supine | Supine | Sitting - Hips and Knees at 90° | |
| Knee | Extension | Supine | Side Lying | Sitting |
| Flexion | Prone | Side Lying | Prone or Standing | |
| Ankle | Plantarflexion | Prone | Side Lying | Prone or Standing |
| Dorsiflexion | Supine | Side Lying | Supine or Sitting | |
| Eversion | Supine | Supine | Side Lying | |
| Inversion | Supine | Supine | Side Lying | |
Stabilisation[edit | edit source]
The patient’s body needs to be placed in a stable position with the joint acted on by the muscle firmly fixed in place. This stabilisation comes initially from the effect of gravity and the weight of the patient on the treatment table or chair. Hand placement of the rehabilitation professionals on the limb to be assessed offers additional stabilisation of the proximal joints while the resistance is placed distally.
Demonstration[edit | edit source]
Application of Resistance[edit | edit source]
In manual muscle testing, external force (resistance) is applied at the end of the range in one-joint muscles to allow for consistency of procedure. Two-joint muscles are typically tested in mid-range where length-tension is more favorable. Ideally, all muscles and muscle groups should be tested at optimal length-tension, but there are many occasions in manual muscle testing where the therapist is not able to distinguish between Grade 5 and 4 without putting the patient at a mechanical disadvantage. The point on an extremity, or part, where the therapist should apply resistance is near the distal end of the segment to which the muscle attaches.
Application of Grades[edit | edit source]
Always start with testing for Grade 3 to determine if the patient can move through the full range of motion against gravity ensuring to isolate muscle or muscle group to be tested
Application of Resistance[edit | edit source]
Ensure to apply resistance slowly and gradually at the distal end of the limb with pressure opposite the line of pull of the muscle to be tested.
Comparison (if applicable)[edit | edit source]
Always ensure to check strength on the uninvolved side first where possible, ensuring understanding of the test and to be able to determine a baseline for force application to the affected limb.
Objectivity[edit | edit source]
Documentation[edit | edit source]
Documentation of manual muscle testing should list the muscle being tested, muscle grade allocated, symptoms experienced that may have impacted on strength and any changes needed to positioning to complete the test. e.g. right quadriceps 4/5 without discomfort performed in supine
Clinical Significance[edit | edit source]
Muscle strength testing can help be utilised to determine if there is a loss in muscle strength. Careful and consistent technique is important to ensure valid and reproducible results. Understanding the factors that may impact on muscle strength are also important in order to clinically reason why the person is experiencing loss of strength. Manual muscle testing with the Oxford Scale is the most commonly used grading scale, which is quick to complete and does not require special equipment, and while it is a subjective measure it demonstrates reasonable inter-rater reliability. More precise methods of measurement, such as dynamometry, are less subjective and provide a quantifiable measurement that can be tracked over time but can be more time consuming to complete and require access to more expensive equipment.
Resources[edit | edit source]
References [edit | edit source]
- ↑ Timothy J Suchomel, Sophia Nimphius, Christopher R Bellon, Michael H Stone.The Importance of Muscular Strength: Training Considerations.PubMed.gov.National Library of Medicine.National Centre for Biotechnology Information.2018 Apr;48(4):765-785.doi: 10.1007/s40279-018-0862-z.
- ↑ OpenStax. Anatomy and Physiology Chapter. 10.4 Nervous System Control of Muscle Tension. Available from: https://openstax.org/books/anatomy-and-physiology/pages/10-4-nervous-system-control-of-muscle-tension#fig-ch10_04_01(accessed 23 March 2023).
- ↑ Bohannon RW. Contribution of neural and muscular factors to the short duration tension-developing capacity of skeletal muscle. Journal of Orthopaedic & Sports Physical Therapy. 1983 Nov 1;5(3):139-47.
- ↑ Graven-Nielsen T, Arendt-Nielsen L. Impact of clinical and experimental pain on muscle strength and activity. Current rheumatology reports. 2008 Dec;10(6):475-81.
- ↑ Van Wilgen CP, Akkerman L, Wieringa J, Dijkstra PU. Muscle strength in patients with chronic pain. Clinical rehabilitation. 2003 Dec;17(8):885-9.
- ↑ Tuttle CS, Thang LA, Maier AB. Markers of inflammation and their association with muscle strength and mass: A systematic review and meta-analysis. Ageing research reviews. 2020 Dec 1;64:101185.
- ↑ Powers SK, Lynch GS, Murphy KT, Reid MB, Zijdewind I. Disease-induced skeletal muscle atrophy and fatigue. Medicine and science in sports and exercise. 2016 Nov;48(11):2307.
- ↑ Melton LJ. Khosla S, Crowson CS, O'Connor MK, O'Fallon WM, and Riggs BL. Epidemiology of sarcopenia. J Am Geriatr Soc. 2000;48:625-30.
- ↑ Volpi E, Nazemi R, Fujita S. Muscle tissue changes with aging. Current opinion in clinical nutrition and metabolic care. 2004 Jul;7(4):405.
- ↑ Henwood TR, Riek S, Taaffe DR. Strength versus muscle power-specific resistance training in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2008; 63(1):83-91.
- ↑ Bunn JA. Aging and the Motor Unit. J Sport Medic Doping Studie. 2012; S1:e001. doi:10.4172/2161-0673.S1-e001
- ↑ Kendall FP, Kendall McCreary E, Geise Provance P, McIntyre Rodgers M and Romani WA. Muscles Testing and Function with Posture and Pain - Fifth Edition. Philadelphia: Lippincott Williams and Wilkins, 2005.
- ↑ Naqvi U. Muscle strength grading. InStatpearls [Internet] 2019 May 29. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436008/ (last accessed 7.1.20)
- ↑ Naqvi U. Muscle strength grading. InStatPearls [Internet] 2021 Sep 2. StatPearls Publishing.
- ↑ Sole G. Physical Therapy of the Shoulder. New Zealand Journal of Physiotherapy. 2004 Jul 1;32(2):87-8.






