Ankle Osteochondral Lesions
Original Editors - Lore Aerts
Top Contributors - Allan D'Hose, Lore Aerts, Admin, Scott Cornish, Kim Jackson, Rachael Lowe, 127.0.0.1, WikiSysop, Wanda van Niekerk, Ward Willaert, Pinar Kisacik, Ewa Jaraczewska, Maarten Cnudde and Cameron Mostinckx
Search Strategy[edit | edit source]
Searched by the following link:
http://biblio.vub.ac.be/vspaces/Vubis.csp?Profile=VUBPORTAL&OpacLanguage=dut
This link gives all the relevant articles that you can find on pubmed, web of knowledge, google, medicine,..
The keywords I used where ; osteochondral lesions of the ankle, osteochondral lesions, osteochondral defects, characteristics of osteochondral ankle lesions.
Definition/Description[edit | edit source]
Symptomatic osteochondral ankle defects often require surgical treatment. An osteochondral ankle defect is a lesion of the talar cartilage and subchondral bone mostly caused by a single or multiple traumatic events, leading to partial or complete detachment of the fragment. The defects cause deep ankle pain associated with weightbearing. Impaired function, limited range of motion, stiffness, catching, locking and swelling may be present. These symptoms place the ability to walk, work and perform sports at risk.
Osteochondral lesion may also involve the talar dome, most frequently the medial aspect. It is relatively prevalent and are an important cause of ankle morbidity.[1]
Osteochondral lesion of the talus (OLT) is a broad term used to describe an injury or abnormality of the talar articular cartilage and adjacent bone. Historically, a variety of terms have been used to refer to this clinical entity including osteochondritis dissecans, osteochondral fracture, and osteochondral defect. Currently, six characteristics are used to categorize a particular lesion. An OLT can be described as chondral (cartilage only), chondral-subchondral (cartilage and bone), subchondral (intact overlying cartilage), or cystic. Lesions can then be subdivided as stable or unstable and non-displaced or displaced. The stability of a lesion can be assessed directly with arthroscopy or indirectly with MRI using DeSmet’s criteria.6 A lesion can also be categorized by its location on the articular surface of the talus as medial, lateral, or central with added subdivisions into anterior, central, or posterior as advocated by some authors.82 An additional description of identifying whether the lesion is contained or uncontained (shoulder) may also be included. Finally, although no accepted definition of lesion size exists, OLTs can generally be considered as either small or large based on their cross-sectional area or greatest diameter (area greater than or less than 1.5 cm2 or diameter greater than or less than 15 mm).[2][3][4]
Epidemiology /Etiology[edit | edit source]
As the foot was inverted on the leg, the lateral border of the talar dome was compressed against the face of the fibula. When the lateral ligament ruptured, avulsion of the chip began. With the use of excessive inverting force, the talus within the mortise was rotated laterally in the frontal plane, impacting and compressing the lateral talar margin against the articular surface of the fibula. A portion of the talar margin was sheared off from the main body of the talus, which caused the lateral OD. A medial lesion was reproduced by plantarflexing the ankle in combination with slight anterior displacement of the talus on the tibia, inversion and internal rotation of the talus on the tibia.
As the foot is inverted on the leg, the lateral border is compressed against the face of the fibula (stage I), while the collateral ligament remains intact. Further inversion ruptures the lateral ligament and begins avulsion of the chip (stage II), which may be completely detached but remain in place (stage III) or be displaced by inversion (stage IV).
Characteristics/Clinical Presentation[edit | edit source]
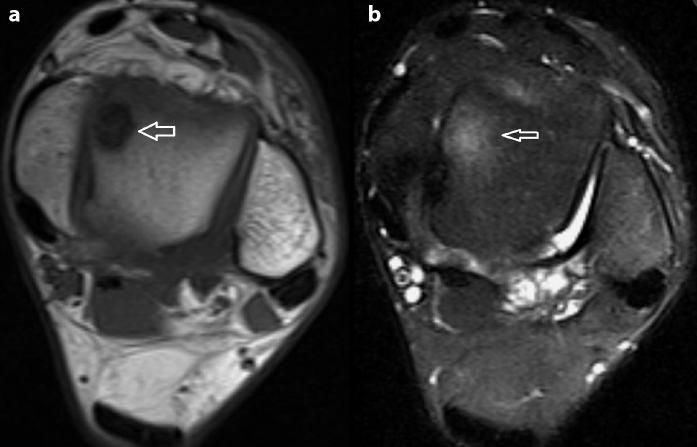
Because the injury is intra-articular is it hard to see what damage it causes. Therefore we have to use MRI scans to get a clearer view. On these images it is clear to see that the surface of cartilage is damaged and we have to prevent further bone damage. Image below is a good example, the ankle on the right shows us bone oedema. If only the cartilage is damaged we can call it chondral and it is cartilage and bone we call it osteochondral lesion.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[5]
Younger people have a higher incidence of trauma history and the lesion size is larger. It is suggested that younger patients are more exposed to sport activities.[6]
Differential Diagnosis[edit | edit source]
add text hereDiagnosing an osteochondral lesion is very difficult on a physical exam an done rarely diagnoses this without further testing. Besides an osteochondral lesion, clinicians should not rule out other diagnoses (with similar symptoms) such as: Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[7]
- Loose bodies
- Synovitis
- Ligament injury
- Fracture or crack of the talus
- Cyst formation
Diagnostic Procedures[edit | edit source]
add text here related to medical diagnostic procedures
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
add text here related to physical examination and assessment
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
Physiotherapy treatment is vital for all patients with an osteochondral lesion of the talar dome to hasten the healing process, ensure an optimal outcome and reduce the likelihood of recurrence
- soft tissue massage
- Electrotherapy (e.g. ultrasound)
- anti-inflammatory advice
- joint mobilization
- ankle Taping
- ankle bracing
- ice or heat treatment
- exercises to improve flexibility, strength and balance
- education
- activity modification advice
- crutches prescription
- the use of a protective boot
- biomechanical correction
- a gradual return to activity program
Several factors may also slow the healing process and increase the likelihood of a poor outcome in patients with this condition. These factors should be assessed and corrected by the treating physiotherapist and may include:
- poor foot mechanics
- joint stiffness
- poor flexibility
- inadequate strength
- poor balance
If there is no sign of result, further investigation is required. X-ray, CT scan or MRI, or a review by a specialist who can advise on any procedures that may be appropriate to improve the condition. A review with a podiatrist may also be indicated for the prescription of orthotics and appropriate footwear advice.
Exercises for the foot are plantar flexion, dorsal flexion, eversion and inversion movements. The patient have to do these movements without feeling any pain and with a repetition of 10 – 20 times. Without increase in symptoms. Another exercise is the lunge stretch, hold for 5 seconds and repeat 10 times. The knee can not come before the toes. Also no increase in symptoms. Al those exercise has to be painless.
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
1. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2809940/?tool=pubmed
2. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855020/?tool=pubmed
3. http://web.jbjs.org.uk/cgi/reprint/85-B/7/989
4. http://www.physioadvisor.com.au/8071091/osteochondral-lesion-of-the-talar-dome-ankle-spr.htm
5. http://ajs.sagepub.com/content/38/2/392.full.pdf+html?sid=9a33506f-84c0-4a7f-b1b8-c04358962f3d
6. http://www.osteochondraldefects.com/index.html
7. http://emedicine.medscape.com/article/1237723-overview
8. http://www.podiatrytoday.com/article/6304
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ 1.Osteochondral Lesions of Major Joints Büyük Eklemlerin Osteokondral Lezyonları Irmak Durur-Subasi, Afak Durur-Karakaya, Omer Selim Yildirim; Eurasian J Med 2015; 47: 138-44 2A
- ↑ 2.Current Concept Review: Osteochondral Lesions of the Talus Patrick J. McGahan, MD and Stephen J. Pinney, MD, FRCS(C) Sacramento, CA; Foot & Ankle International/Vol. 31, No. 1/January 2010 3A
- ↑ 3.Current Concept Review: Osteochondral Lesions of the Talus Patrick J. McGahan, MD and Stephen J. Pinney, MD, FRCS(C) Sacramento, CA; Foot & Ankle International/Vol. 31, No. 1/January 2010 3A
- ↑ 4.Assenmacher, JA; Kelikian, AS; Gottlob, C; Kodros, S: Arthroscopically assisted autologous osteochondral transplantation for osteochondral lesions of the talar dome: an MRI and clinical follow-up study. Foot Ankle Int. 22(7):544– 51, 2001. 2A
- ↑ 6.Osteochondral Lesions of Major Joints Büyük Eklemlerin Osteokondral Lezyonları Irmak Durur-Subasi, Afak Durur-Karakaya, Omer Selim Yildirim; Eurasian J Med 2015; 47: 138-44 2A
- ↑ 7.Comparison of chondral versus osteochondral lesions of the talus after arthroscopic microfracture, Hyeong-Won Park et al., level of evidence: 1B
- ↑ 4.Assenmacher, JA; Kelikian, AS; Gottlob, C; Kodros, S: Arthroscopically assisted autologous osteochondral transplantation for osteochondral lesions of the talar dome: an MRI and clinical follow-up study. Foot Ankle Int. 22(7):544– 51, 2001. 2A