Anatomy of the Temperomandibular Joint: Difference between revisions
No edit summary |
No edit summary |
||
| (35 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Jess Bell|Jess Bell]] based on the course by [https://members.physio-pedia.com/course_tutor/victoria-reboredo/ Victoria Reboredo]<br> | <div class="editorbox"> '''Original Editor '''- [[User:Jess Bell|Jess Bell]] based on the course by [https://members.physio-pedia.com/course_tutor/victoria-reboredo/ Victoria Reboredo]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
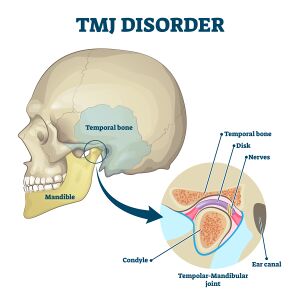
The temporomandibular joint (TMJ) is | [[File:TMJ Disorder shutterstock 1716625330.jpeg|thumb|Figure 1. TMJ Anatomy. ]] | ||
The temporomandibular joint (TMJ) is involved in mastication (chewing) and speech and it is one of the most frequently moved joints in humans.<ref>Thirunavukarasu AJ, Ferro A, Sardesai A, Biyani G, Dubb SS, Brassett C, Hamilton DL. [https://onlinelibrary.wiley.com/doi/full/10.1002/ca.23719 Temporomandibular joint anatomy: ultrasonographic appearances and sexual dimorphism]. Clin Anat. 2021 Oct;34(7):1043-9. </ref> This [[Synovial Joints|synovial joint]] must be able to respond to significant biomechanical load.<ref>Whyte A, Boeddinghaus R, Bartley A, Vijeyaendra R. [https://www.sciencedirect.com/science/article/abs/pii/S0009926020302531 Imaging of the temporomandibular joint]. Clin Radiol. 2021 Jan;76(1):76.e21-76.e35. </ref> It is made up of the articulating surface of the temporal bone and the head of the mandible. The whole joint is enclosed in a fibrous capsule.<ref name=":0">Maini K, Dua A. Temporomandibular Joint Syndrome. [Updated 2021 Apr 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551612/ </ref> The TMJ is defined as a ginglymoarthrodial [[Joint Classification|joint]] (i.e. both a hinge and a gliding joint<ref>Bodnar SE, Zdilla MJ. [https://faseb.onlinelibrary.wiley.com/doi/abs/10.1096/fasebj.2018.32.1_supplement.639.13 The relationship of the articular eminence with the mandibular fossa: implications for temporomandibular joint mechanics]. Experimental Biology 2018 Meeting Abstracts. 2018;32(S1):639.</ref>). It allows a rotational movement in the sagittal plane and a translation movement on its own axis.<ref name=":1">Reboredo V. Anatomy of the Temporomandibular Joint Course. Plus , 2021.</ref><ref name=":2">Wadhwa S, Kapila S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2547984/ TMJ disorders: future innovations in diagnostics and therapeutics]. J Dent Educ. 2008;72(8):930-47. </ref> The translation motion generates more movement.<ref name=":1" /> | |||
== Unique Features == | == Unique Features == | ||
The TMJ is unique from other synovial joints | The TMJ is unique from other synovial joints for the following reasons:<ref name=":1" /><ref name=":3">Tanaka E, Koolstra JH. [https://journals.sagepub.com/doi/10.1177/154405910808701101?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed Biomechanics of the temporomandibular joint]. J Dent Res. 2008;87(11):989-91.</ref> | ||
The role of occlusion in TMJ is controversial.<ref>Al-Ani Z. [https://journals.sagepub.com/doi/full/10.1177/2050168420911029 Occlusion and temporomandibular disorders: a long-standing controversy in dentistry]. Prim Dent J. 2020;9(1):43-8. </ref> | # Intra-articular disc | ||
#* This disc divides the joint into two compartments (i.e. superior and inferior), which allows different actions to occur simultaneously in different parts of the joint in a coordinated manner.<ref name=":3" /> | |||
# Bilaterality | |||
#* The mandible articulates on both sides of the skull - from a mechanical point of view, any movement on one side will always affect the other side.<ref name=":3" /> | |||
# Fibrous [[cartilage]] | |||
#* While hyaline cartilage typically covers the articular surfaces in synovial joints, the main articular surfaces of the TMJ (i.e. the mandibular condyle and the temporal bone) are covered by fibrous cartilage.<ref name=":2" /> Fibrocartilage contains type I and II [[Collagen|collagens]] whereas articular hyaline cartilage only contains type II collagen. Fibrocartilage is more resistant to sheer forces, so it is better able to absorb load and compressive forces.<ref name=":1" /><ref name=":2" /> It is, however, also more sensitive to friction, which is an important factor when considering degenerative pathology of the TMJ.<ref name=":1" /> | |||
# Occlusion | |||
#* Occlusion refers to the relationship between the upper and lower teeth when the jaw closes.<ref>Pai SA, Poojari SR, Ramachandra K, Patel RKV, Jyothi M. Temporomandibular joint - an anatomical view. Journal of Advanced Clinical & Research Insights. 2019;6:1-5. </ref> The TMJ is the only human joint that has a rigid end point (caused by the teeth coming into contact). Occlusion via the teeth maintains the vertical dimension in a sagittal plane and ensures that pressure is distributed along the whole joint.<ref name=":1" /> | |||
#* The role of occlusion in the TMJ is controversial.<ref>Al-Ani Z. [https://journals.sagepub.com/doi/full/10.1177/2050168420911029 Occlusion and temporomandibular disorders: a long-standing controversy in dentistry]. Prim Dent J. 2020;9(1):43-8. </ref> Differences in occlusion are not necessarily associated with TMJ dysfunction. However, a loss of height and separation in the mandibular bone and the jaw at the end of the closing movement (i.e. in individuals who lose teeth) can cause changes in the joint's intra-articular pressure and lead to earlier degeneration.<ref name=":1" /> | |||
== Intra-Articular Disc == | == Intra-Articular Disc == | ||
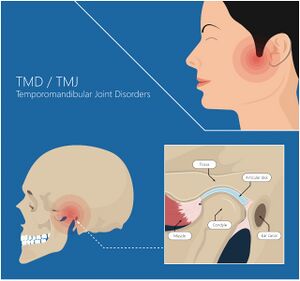
The intra-articular disc is made of fibrocartilage. Its extracellular matrix is largely made up of collagen I and elastin. Collagen I helps to resist tensile forces | [[File:TMJ TMD.jpg|thumb|Figure 2. TMJ disc location.]] | ||
The intra-articular disc is the central anatomic structure of the TMJ.<ref name=":7">Physiopedia. [[Functional Anatomy of the Head and Jaw]].</ref> It is made of fibrocartilage. Its extracellular matrix is largely made up of collagen I and elastin. Collagen I helps the disc to resist tensile forces while elastin helps it to maintain its shape after deformation.<ref>Runci Anastasi M, Cascone P, Anastasi GP, Santoro G, Nicita F, Picciolo G et al. [https://www.mdpi.com/2411-5142/6/1/22 Articular disc of a human temporomandibular joint: evaluation through light microscopy, immunofluorescence and scanning electron microscopy]. J Funct Morphol Kinesiol. 2021;6(1):22. </ref> | |||
It is located between the mandible condyle and the temporal fossa.<ref name=":0" /> It is not vascularised and has little innervation.<ref name=":1" /> | It is located between the mandible condyle and the temporal fossa (see Figure 1 and 2).<ref name=":0" /> It is not vascularised and has little innervation.<ref name=":1" /><ref name=":4">Palacios AAN. Modeling a mandibular functional shift and the resulting temporomandibular joint dysfunction in mice [dissertation]. San Francisco: University of California. 2020. </ref> | ||
Functions of the intra-articular disc include: ( | Functions of the intra-articular disc include:<ref>Beek M, Koolstra JH, van Ruijven LJ, van Eijden TM. [https://www.researchgate.net/profile/Jan-Harm-Koolstra/publication/241854570_Three-dimensional_finite_element_analysis_of_the_cartilagineous_structures_in_the_human_temporomandibular_joint/links/54bcf9900cf24e50e940da73/Three-dimensional-finite-element-analysis-of-the-cartilagineous-structures-in-the-human-temporomandibular-joint.pdf Three-dimensional finite element analysis of the human temporomandibular joint disc]. J Biomech. 2000;33(3):307-16. </ref><ref>Ferreira FM, Cézar Simamoto-Júnior P, Soares CJ, Ramos AMAM, Fernandes-Neto AJ. [https://www.scielo.br/j/bdj/a/tkbJTx6qm4gkN99YDkctbjj/?format=html Effect of occlusal splints on the stress distribution on the temporomandibular joint disc]. Braz Dent J. 2017;28(3):324-9.</ref> | ||
* Creating articular congruence | * Creating articular congruence | ||
* Absorbing and distributing load over larger areas in order to prevent damage to the articular surfaces | * Absorbing and distributing load over larger areas in order to prevent damage to the articular surfaces | ||
The disc divides the TMJ fossa into two compartments, thus creating two new articular surfaces: | The disc divides the TMJ fossa into two compartments, thus creating two new articular surfaces:<ref name=":1" /><ref>Cobo J, Cabrera-Freitag M, Cobo T, Muriel J, Junquera L, Cobo J et al. [https://www.intechopen.com/books/cartilage-tissue-engineering-and-regeneration-techniques/nonsurgical-strategies-for-the-treatment-of-temporomandibular-joint-disorders Nonsurgical strategies for the treatment of temporomandibular joint disorders]. In: Nikolopoulos DD, Safos GK Dimitrios K editors. Cartilage tissue engineering and regeneration techniques. IntechOpen, 2019. </ref> | ||
# Upper or temporodisc chamber | # Upper or temporodisc chamber | ||
# Lower or condylar disc chamber | # Lower or condylar disc chamber | ||
These surfaces have the | These surfaces have the ability to move between each other in an isolated way or in a synchronised way. Essentially, the disc acts as a largely passive, but movable articular surface which can accommodate translational movements of the condyle.<ref name=":3" /> | ||
When increased load is applied to the TMJ (i.e. during mastication), the fibrocartilage is able to modulate its water content and ensure that the load is shared.<ref name=":1" /> | |||
Unlike the disc, the retro-discal area is highly vascularised and richly innervated.<ref name=":4" /> In cases of articular dysfunction, this is a key area that can cause symptoms.<ref name=":1" /> | |||
Please watch the following video for an overview of the anatomy of the TMJ. | |||
{{#ev:youtube|_TJd7lKC064}}<ref>Geeky Medics. Temporomandibular Joint (TMJ) Anatomy (3D Anatomy Tutorial). Available from: https://www.youtube.com/watch?v=_TJd7lKC064 [last accessed 22/6/2021]</ref> | |||
== Articular Capsule == | |||
Like any synovial joint, the TMJ has a joint capsule that surrounds all the articular elements. This capsule has an external and internal layer. The external layer is a fibrous membrane, which is thickened laterally by the temporomandibular ligament. The anterior and posterior part of the capsule are thinner and more elastic, thus allowing for the glide of the condyle disc complex in the sagittal plane.<ref name=":1" /> | |||
The internal or [[Synovium & Synovial Fluid|synovial]] layer generates the intra-articular fluid that lubricates the jaw and decreases friction between the surfaces. It is also involved in the nourishment of the intra-articular tissues and helps to remove metabolic residues.<ref name=":1" /> | |||
The capsule is highly innervated by the [[Trigeminal Nerve|trigeminal]] nerve (i.e. cranial nerve V):<ref name=":5">Bordoni B, Varacallo M. Anatomy, Head and Neck, Temporomandibular Joint. [Updated 2021 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538486/ </ref> | |||
* The anterolateral portion is innervated by the masseteric nerve, which is a motor branch of the anterior division of the mandibular division of the trigeminal nerve<ref>Hacking C. Masseteric nerve [Internet]. Radiopedia [cited 23 June 2021]. Available from: https://radiopaedia.org/articles/masseteric-nerve</ref> | |||
* The lateral area is innervated by the auriculotemporal nerve, which is a sensory branch of the posterior division of the mandibular division of the trigeminal nerve<ref>Hacking C. Auriculotemporal nerve [Internet]. Radiopedia [cited 23 June 2021]. Available from: https://radiopaedia.org/articles/auriculotemporal-nerve</ref> | |||
The trigeminal nerve also innervates the tympanic membrane, the anterior cochlear surface, the external auditory canal, the temporal region, the parotid gland and, alongside the facial nerve (i.e. cranial nerve VII), the skin and posterior part of the cheek. This is significant because an articular problem at this level can cause painful sensations around the auricle and on the skin in the area.<ref name=":1" /> | |||
The articular capsule is supplied by the maxillary, temporal and masseteric arteries.<ref name=":1" /><ref name=":5" /> | |||
== Ligaments == | |||
The [[Ligament|ligaments]] of the TMJ can be divided into intrinsic and extrinsic ligaments.<ref name=":1" /> | |||
* Intrinsic ligaments: | |||
** collateral disc ligaments | |||
** temporomandibular ligament | |||
* Extrinsic ligaments: | |||
** affect the position of the bony levers in the TMJ | |||
=== Collateral Disc Ligaments === | |||
The collateral ligaments (also known as the discal ligaments) are intra-capsular. They connect the articular disc to the joint capsule<ref>Fuentes R, Dias F, Salamanca C, Borie-Echevarría E, Ottone NE. [https://scielo.conicyt.cl/pdf/ijmorphol/v36n1/0717-9502-ijmorphol-36-01-00087.pdf Review of the Tanaka ligament in the temporomandibular joint. Analyzing its scientific validity]. International Journal of Morphology. 2018;36:87-91.</ref> and are made of two fascicles: one lateral and one medial.<ref name=":1" /> | |||
Their primary function is to help to prevent movement of the intra-articular disc away from the condyle. Movement of the condyle-disc complex depends on these ligaments - the disc modifies its position depending on the position of the condyle during movement in order to improve pressure distribution. As these ligaments are richly innervated, they also provide [[Proprioception|proprioceptive]] and [[Pain Behaviours|pain]] information.<ref name=":1" /> | |||
=== Temporomandibular Ligament === | |||
As mentioned above, the temporomandibular ligament is considered a reinforcement of the capsule. It originates at the lower articular tubercle of the zygomatic arch and inserts into the lateral and posterior border of the neck of the mandible.<ref name=":7" /> It restricts jaw closure and mandible retraction, thus protecting the retro-discal tissues.<ref name=":1" /> | |||
=== Extrinsic Ligaments === | |||
* Stylomandibular - acts to limit excessive protrusion of the jaw<ref name=":5" /> | |||
* Sphenomandibular - primarily acts to protect the TMJ from excessive translation of the condyle after the mouth is opened more than 10 degrees<ref name=":5" /> | |||
* Pterigomandibular - limits excessive jaw movements<ref name=":5" /> | |||
Together these ligaments maintain the position of the jaw against gravity (i.e. jaw suspension).<ref name=":1" /> | |||
Please watch the video below for further discussion of the anatomy of the TMJ. | |||
{{#ev:youtube|6tJsi5oghNY}}<ref>Dr.G Bhanu Prakash Animated Medical Videos. Anatomy of Temporomandibular joint ( TMJ ) Head and Neck - Gross Anatomy medical animations. Available from: https://www.youtube.com/watch?v=6tJsi5oghNY [last accessed 22/6/2021]</ref> | |||
== Innervation and Vascularisation == | |||
The TMJ is innervated by the mandibular nerve, which is the third root of the trigeminal nerve (cranial nerve V).<ref name=":1" /> | |||
The superficial temporal artery and maxillary artery run along the lateral and medial sides of the condylar neck. The temporal superficial and internal maxillary arteries supply the TMJ through the auricular root. Both of these arteries arise from the external carotid.<ref name=":1" /><ref>Cuccia AM, Caradonna C, Caradonna D, Anastasi G, Milardi D, Favaloro A et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3604369/ The arterial blood supply of the temporomandibular joint: an anatomical study and clinical implications]. Imaging Sci Dent. 2013;43(1):37-44.</ref> | |||
The key veins are the pterygoid plexus and superficial temporal veins.<ref name=":1" /> | |||
== Musculature == | |||
<gallery caption="" widths="260px" heights="260px" perrow="3"> | |||
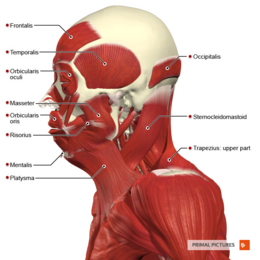
File:Superficial muscles of the head and neck lateral aspect Primal.png|thumb|Figure 3. Temporalis, masseter, platysma | |||
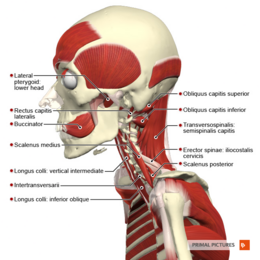
File:Deep muscles of the head and neck lateral aspect Primal.png|thumb|Figure 4. Lateral pterygoid | |||
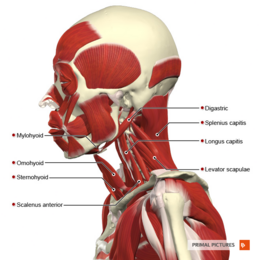
File:Intermediate muscles of the head and neck lateral aspect Primal.png|thumb|Figure 5. Mylohyoid, sternohyoid, digastric | |||
</gallery> | |||
Movements at the TMJ are:<ref name=":1" /> | |||
* Opening and closing (descending and ascending movements) | |||
* Lateral movements (lateral glide, left and right) | |||
* Anterior posterior movements in a horizontal plane (mandibular protraction and retraction) | |||
The muscles involved in elevating the mandible (i.e. closing the jaw) are:<ref name=":6">Corcoran NM, Goldman EM. Anatomy, Head and Neck, Masseter Muscle. [Updated 2020 Jul 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539869/ </ref> | |||
* Temporalis | |||
* Masseter | |||
* Medial pterygoid | |||
See figure 3. | |||
The muscles involved in descension of the mandible (i.e. opening the jaw) are:<ref name=":1" /><ref name=":6" /> | |||
* Lateral pterygoid (see figure 4) | |||
* Suprahyoid | |||
* Infrahyoid | |||
{| class="wikitable" | |||
|+Table 1. Muscles acting on the TMJ.<ref name=":1" /><ref name=":7" /> | |||
!Muscle | |||
!Origin | |||
!Insertion | |||
!Innervation | |||
!Actions | |||
|- | |||
|Temporalis | |||
|Temporal bone | |||
|Coronoid process of the mandible | |||
|''Central part'': deep temporal nerves of the mandibular nerve | |||
''Anterior part'': branches of the buccal nerve ''Posterior part'': branches of the masseteric nerve | |||
|Elevates and retracts the mandible | |||
|- | |||
|Masseter | |||
|Zygomatic arch | |||
|Angle of the mandible | |||
|Mandibular branch (V3) of the trigeminal nerve. | |||
|Elevates the mandible | |||
|- | |||
|Lateral pterygoid (superior and inferior heads) | |||
|Superior head: sphenoid bone, | |||
In ferior head: sphenoid bone | |||
|Superior head: capsule and articular disc of the TMJ, | |||
Inferior head: pterygoid process of the mandible | |||
|Mandibular branch (V3) of the trigeminal nerve | |||
|Unilateral action: lateral mandible deviation to the ''opposite side.'' | |||
Bilateral action: mandible protraction. | |||
Depresses the chin. | |||
|- | |||
|Medial pterygoid | |||
|Sphenoid, | |||
maxilla, and palatine bones | |||
|Angle of the mandible | |||
|Mandibular branch (V3) of the trigeminal nerve | |||
|Works with masseter to elevate the mandible and aids in protraction. | |||
Also assists in lateral deviation. | |||
|- | |||
|Digastric: | |||
Anterior belly (DAB) | |||
Posterior belly (DPB) | |||
|''DAB'': digastric fossa of mandible | |||
''DPB'': mastoid notch of the temporal bone | |||
|DAB/DPB: Body of the hyoid bone | |||
|''DAB'': Mylohyoid nerve of the inferior alveolar nerve (Mandibular division of the trigeminal nerve (CN V) | |||
''DPB'': digastric branch of the facial nerve (CN VII) | |||
|Depresses the mandible. | |||
Assists with chewing and swallowing as it elevates the hyoid bone. | |||
|- | |||
|Stylohyoid | |||
|Styloid process of temporal bone | |||
|Body of the hyoid bone | |||
|Stylohyoid branch of facial nerve (CN VII) | |||
|Depress the mandible against resistance when the infrahyoid muscles stabilise or depress the hyoid bone | |||
|- | |||
|Mylohyoid | |||
|Mandible near the molars | |||
|Hyoid bone | |||
|Mylohyoid nerve of the inferior alveolar nerve (Mandibular division of the trigeminal nerve (Cranial nerve V, CN V) | |||
|Elevates the hyoid bone and floor of the mouth. | |||
Depresses the mandible. | |||
|- | |||
|Geniohyoid | |||
|Inferior mental spine: the posterior surface of the mandible near the lower part of the mandibular symphysis | |||
|Superior border of the body of the hyoid bone | |||
|C1 via the hypoglossal nerve | |||
|Depress the mandible against resistance when the infrahyoid muscles stabilise or depress the hyoid bone | |||
|- | |||
|Platysma | |||
|Skin and fascia of the shoulder | |||
Superior thoracic regions | |||
|Mandible, lower lip, modiolus | |||
|Cervical branch of the facial nerve (CN VII) | |||
Transverse cervical nerve | |||
|Depresses the mandible against resistance. | |||
Pulls down the corner of the mouth and hee lower lip. | |||
|} | |||
== References == | |||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
<references /> | |||
[[Category:Plus Content]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Head - TMJ]] | |||
Latest revision as of 11:48, 17 October 2023
Top Contributors - Jess Bell, Kim Jackson, Tarina van der Stockt, Rucha Gadgil, Lucinda hampton and Olajumoke Ogunleye
Introduction[edit | edit source]
The temporomandibular joint (TMJ) is involved in mastication (chewing) and speech and it is one of the most frequently moved joints in humans.[1] This synovial joint must be able to respond to significant biomechanical load.[2] It is made up of the articulating surface of the temporal bone and the head of the mandible. The whole joint is enclosed in a fibrous capsule.[3] The TMJ is defined as a ginglymoarthrodial joint (i.e. both a hinge and a gliding joint[4]). It allows a rotational movement in the sagittal plane and a translation movement on its own axis.[5][6] The translation motion generates more movement.[5]
Unique Features[edit | edit source]
The TMJ is unique from other synovial joints for the following reasons:[5][7]
- Intra-articular disc
- This disc divides the joint into two compartments (i.e. superior and inferior), which allows different actions to occur simultaneously in different parts of the joint in a coordinated manner.[7]
- Bilaterality
- The mandible articulates on both sides of the skull - from a mechanical point of view, any movement on one side will always affect the other side.[7]
- Fibrous cartilage
- While hyaline cartilage typically covers the articular surfaces in synovial joints, the main articular surfaces of the TMJ (i.e. the mandibular condyle and the temporal bone) are covered by fibrous cartilage.[6] Fibrocartilage contains type I and II collagens whereas articular hyaline cartilage only contains type II collagen. Fibrocartilage is more resistant to sheer forces, so it is better able to absorb load and compressive forces.[5][6] It is, however, also more sensitive to friction, which is an important factor when considering degenerative pathology of the TMJ.[5]
- Occlusion
- Occlusion refers to the relationship between the upper and lower teeth when the jaw closes.[8] The TMJ is the only human joint that has a rigid end point (caused by the teeth coming into contact). Occlusion via the teeth maintains the vertical dimension in a sagittal plane and ensures that pressure is distributed along the whole joint.[5]
- The role of occlusion in the TMJ is controversial.[9] Differences in occlusion are not necessarily associated with TMJ dysfunction. However, a loss of height and separation in the mandibular bone and the jaw at the end of the closing movement (i.e. in individuals who lose teeth) can cause changes in the joint's intra-articular pressure and lead to earlier degeneration.[5]
Intra-Articular Disc[edit | edit source]
The intra-articular disc is the central anatomic structure of the TMJ.[10] It is made of fibrocartilage. Its extracellular matrix is largely made up of collagen I and elastin. Collagen I helps the disc to resist tensile forces while elastin helps it to maintain its shape after deformation.[11]
It is located between the mandible condyle and the temporal fossa (see Figure 1 and 2).[3] It is not vascularised and has little innervation.[5][12]
Functions of the intra-articular disc include:[13][14]
- Creating articular congruence
- Absorbing and distributing load over larger areas in order to prevent damage to the articular surfaces
The disc divides the TMJ fossa into two compartments, thus creating two new articular surfaces:[5][15]
- Upper or temporodisc chamber
- Lower or condylar disc chamber
These surfaces have the ability to move between each other in an isolated way or in a synchronised way. Essentially, the disc acts as a largely passive, but movable articular surface which can accommodate translational movements of the condyle.[7]
When increased load is applied to the TMJ (i.e. during mastication), the fibrocartilage is able to modulate its water content and ensure that the load is shared.[5]
Unlike the disc, the retro-discal area is highly vascularised and richly innervated.[12] In cases of articular dysfunction, this is a key area that can cause symptoms.[5]
Please watch the following video for an overview of the anatomy of the TMJ.
Articular Capsule[edit | edit source]
Like any synovial joint, the TMJ has a joint capsule that surrounds all the articular elements. This capsule has an external and internal layer. The external layer is a fibrous membrane, which is thickened laterally by the temporomandibular ligament. The anterior and posterior part of the capsule are thinner and more elastic, thus allowing for the glide of the condyle disc complex in the sagittal plane.[5]
The internal or synovial layer generates the intra-articular fluid that lubricates the jaw and decreases friction between the surfaces. It is also involved in the nourishment of the intra-articular tissues and helps to remove metabolic residues.[5]
The capsule is highly innervated by the trigeminal nerve (i.e. cranial nerve V):[17]
- The anterolateral portion is innervated by the masseteric nerve, which is a motor branch of the anterior division of the mandibular division of the trigeminal nerve[18]
- The lateral area is innervated by the auriculotemporal nerve, which is a sensory branch of the posterior division of the mandibular division of the trigeminal nerve[19]
The trigeminal nerve also innervates the tympanic membrane, the anterior cochlear surface, the external auditory canal, the temporal region, the parotid gland and, alongside the facial nerve (i.e. cranial nerve VII), the skin and posterior part of the cheek. This is significant because an articular problem at this level can cause painful sensations around the auricle and on the skin in the area.[5]
The articular capsule is supplied by the maxillary, temporal and masseteric arteries.[5][17]
Ligaments[edit | edit source]
The ligaments of the TMJ can be divided into intrinsic and extrinsic ligaments.[5]
- Intrinsic ligaments:
- collateral disc ligaments
- temporomandibular ligament
- Extrinsic ligaments:
- affect the position of the bony levers in the TMJ
Collateral Disc Ligaments[edit | edit source]
The collateral ligaments (also known as the discal ligaments) are intra-capsular. They connect the articular disc to the joint capsule[20] and are made of two fascicles: one lateral and one medial.[5]
Their primary function is to help to prevent movement of the intra-articular disc away from the condyle. Movement of the condyle-disc complex depends on these ligaments - the disc modifies its position depending on the position of the condyle during movement in order to improve pressure distribution. As these ligaments are richly innervated, they also provide proprioceptive and pain information.[5]
Temporomandibular Ligament[edit | edit source]
As mentioned above, the temporomandibular ligament is considered a reinforcement of the capsule. It originates at the lower articular tubercle of the zygomatic arch and inserts into the lateral and posterior border of the neck of the mandible.[10] It restricts jaw closure and mandible retraction, thus protecting the retro-discal tissues.[5]
Extrinsic Ligaments[edit | edit source]
- Stylomandibular - acts to limit excessive protrusion of the jaw[17]
- Sphenomandibular - primarily acts to protect the TMJ from excessive translation of the condyle after the mouth is opened more than 10 degrees[17]
- Pterigomandibular - limits excessive jaw movements[17]
Together these ligaments maintain the position of the jaw against gravity (i.e. jaw suspension).[5]
Please watch the video below for further discussion of the anatomy of the TMJ.
Innervation and Vascularisation[edit | edit source]
The TMJ is innervated by the mandibular nerve, which is the third root of the trigeminal nerve (cranial nerve V).[5]
The superficial temporal artery and maxillary artery run along the lateral and medial sides of the condylar neck. The temporal superficial and internal maxillary arteries supply the TMJ through the auricular root. Both of these arteries arise from the external carotid.[5][22]
The key veins are the pterygoid plexus and superficial temporal veins.[5]
Musculature[edit | edit source]
Movements at the TMJ are:[5]
- Opening and closing (descending and ascending movements)
- Lateral movements (lateral glide, left and right)
- Anterior posterior movements in a horizontal plane (mandibular protraction and retraction)
The muscles involved in elevating the mandible (i.e. closing the jaw) are:[23]
- Temporalis
- Masseter
- Medial pterygoid
See figure 3.
The muscles involved in descension of the mandible (i.e. opening the jaw) are:[5][23]
- Lateral pterygoid (see figure 4)
- Suprahyoid
- Infrahyoid
| Muscle | Origin | Insertion | Innervation | Actions |
|---|---|---|---|---|
| Temporalis | Temporal bone | Coronoid process of the mandible | Central part: deep temporal nerves of the mandibular nerve
Anterior part: branches of the buccal nerve Posterior part: branches of the masseteric nerve |
Elevates and retracts the mandible |
| Masseter | Zygomatic arch | Angle of the mandible | Mandibular branch (V3) of the trigeminal nerve. | Elevates the mandible |
| Lateral pterygoid (superior and inferior heads) | Superior head: sphenoid bone,
In ferior head: sphenoid bone |
Superior head: capsule and articular disc of the TMJ,
Inferior head: pterygoid process of the mandible |
Mandibular branch (V3) of the trigeminal nerve | Unilateral action: lateral mandible deviation to the opposite side.
Bilateral action: mandible protraction. Depresses the chin. |
| Medial pterygoid | Sphenoid,
maxilla, and palatine bones |
Angle of the mandible | Mandibular branch (V3) of the trigeminal nerve | Works with masseter to elevate the mandible and aids in protraction.
Also assists in lateral deviation. |
| Digastric:
Anterior belly (DAB) Posterior belly (DPB) |
DAB: digastric fossa of mandible
DPB: mastoid notch of the temporal bone |
DAB/DPB: Body of the hyoid bone | DAB: Mylohyoid nerve of the inferior alveolar nerve (Mandibular division of the trigeminal nerve (CN V)
DPB: digastric branch of the facial nerve (CN VII) |
Depresses the mandible.
Assists with chewing and swallowing as it elevates the hyoid bone. |
| Stylohyoid | Styloid process of temporal bone | Body of the hyoid bone | Stylohyoid branch of facial nerve (CN VII) | Depress the mandible against resistance when the infrahyoid muscles stabilise or depress the hyoid bone |
| Mylohyoid | Mandible near the molars | Hyoid bone | Mylohyoid nerve of the inferior alveolar nerve (Mandibular division of the trigeminal nerve (Cranial nerve V, CN V) | Elevates the hyoid bone and floor of the mouth.
Depresses the mandible. |
| Geniohyoid | Inferior mental spine: the posterior surface of the mandible near the lower part of the mandibular symphysis | Superior border of the body of the hyoid bone | C1 via the hypoglossal nerve | Depress the mandible against resistance when the infrahyoid muscles stabilise or depress the hyoid bone |
| Platysma | Skin and fascia of the shoulder
Superior thoracic regions |
Mandible, lower lip, modiolus | Cervical branch of the facial nerve (CN VII)
Transverse cervical nerve |
Depresses the mandible against resistance.
Pulls down the corner of the mouth and hee lower lip. |
References[edit | edit source]
- ↑ Thirunavukarasu AJ, Ferro A, Sardesai A, Biyani G, Dubb SS, Brassett C, Hamilton DL. Temporomandibular joint anatomy: ultrasonographic appearances and sexual dimorphism. Clin Anat. 2021 Oct;34(7):1043-9.
- ↑ Whyte A, Boeddinghaus R, Bartley A, Vijeyaendra R. Imaging of the temporomandibular joint. Clin Radiol. 2021 Jan;76(1):76.e21-76.e35.
- ↑ 3.0 3.1 Maini K, Dua A. Temporomandibular Joint Syndrome. [Updated 2021 Apr 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551612/
- ↑ Bodnar SE, Zdilla MJ. The relationship of the articular eminence with the mandibular fossa: implications for temporomandibular joint mechanics. Experimental Biology 2018 Meeting Abstracts. 2018;32(S1):639.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 5.18 5.19 5.20 5.21 5.22 5.23 5.24 5.25 Reboredo V. Anatomy of the Temporomandibular Joint Course. Plus , 2021.
- ↑ 6.0 6.1 6.2 Wadhwa S, Kapila S. TMJ disorders: future innovations in diagnostics and therapeutics. J Dent Educ. 2008;72(8):930-47.
- ↑ 7.0 7.1 7.2 7.3 Tanaka E, Koolstra JH. Biomechanics of the temporomandibular joint. J Dent Res. 2008;87(11):989-91.
- ↑ Pai SA, Poojari SR, Ramachandra K, Patel RKV, Jyothi M. Temporomandibular joint - an anatomical view. Journal of Advanced Clinical & Research Insights. 2019;6:1-5.
- ↑ Al-Ani Z. Occlusion and temporomandibular disorders: a long-standing controversy in dentistry. Prim Dent J. 2020;9(1):43-8.
- ↑ 10.0 10.1 10.2 Physiopedia. Functional Anatomy of the Head and Jaw.
- ↑ Runci Anastasi M, Cascone P, Anastasi GP, Santoro G, Nicita F, Picciolo G et al. Articular disc of a human temporomandibular joint: evaluation through light microscopy, immunofluorescence and scanning electron microscopy. J Funct Morphol Kinesiol. 2021;6(1):22.
- ↑ 12.0 12.1 Palacios AAN. Modeling a mandibular functional shift and the resulting temporomandibular joint dysfunction in mice [dissertation]. San Francisco: University of California. 2020.
- ↑ Beek M, Koolstra JH, van Ruijven LJ, van Eijden TM. Three-dimensional finite element analysis of the human temporomandibular joint disc. J Biomech. 2000;33(3):307-16.
- ↑ Ferreira FM, Cézar Simamoto-Júnior P, Soares CJ, Ramos AMAM, Fernandes-Neto AJ. Effect of occlusal splints on the stress distribution on the temporomandibular joint disc. Braz Dent J. 2017;28(3):324-9.
- ↑ Cobo J, Cabrera-Freitag M, Cobo T, Muriel J, Junquera L, Cobo J et al. Nonsurgical strategies for the treatment of temporomandibular joint disorders. In: Nikolopoulos DD, Safos GK Dimitrios K editors. Cartilage tissue engineering and regeneration techniques. IntechOpen, 2019.
- ↑ Geeky Medics. Temporomandibular Joint (TMJ) Anatomy (3D Anatomy Tutorial). Available from: https://www.youtube.com/watch?v=_TJd7lKC064 [last accessed 22/6/2021]
- ↑ 17.0 17.1 17.2 17.3 17.4 Bordoni B, Varacallo M. Anatomy, Head and Neck, Temporomandibular Joint. [Updated 2021 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538486/
- ↑ Hacking C. Masseteric nerve [Internet]. Radiopedia [cited 23 June 2021]. Available from: https://radiopaedia.org/articles/masseteric-nerve
- ↑ Hacking C. Auriculotemporal nerve [Internet]. Radiopedia [cited 23 June 2021]. Available from: https://radiopaedia.org/articles/auriculotemporal-nerve
- ↑ Fuentes R, Dias F, Salamanca C, Borie-Echevarría E, Ottone NE. Review of the Tanaka ligament in the temporomandibular joint. Analyzing its scientific validity. International Journal of Morphology. 2018;36:87-91.
- ↑ Dr.G Bhanu Prakash Animated Medical Videos. Anatomy of Temporomandibular joint ( TMJ ) Head and Neck - Gross Anatomy medical animations. Available from: https://www.youtube.com/watch?v=6tJsi5oghNY [last accessed 22/6/2021]
- ↑ Cuccia AM, Caradonna C, Caradonna D, Anastasi G, Milardi D, Favaloro A et al. The arterial blood supply of the temporomandibular joint: an anatomical study and clinical implications. Imaging Sci Dent. 2013;43(1):37-44.
- ↑ 23.0 23.1 Corcoran NM, Goldman EM. Anatomy, Head and Neck, Masseter Muscle. [Updated 2020 Jul 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539869/