An Overview of Physiotherapy Assessment and Treatment of the Pelvic Floor: Difference between revisions
No edit summary |
m (Changed protection level for "An Overview of Physiotherapy Assessment and Treatment of the Pelvic Floor" ([Edit=⧼protect-level-ppadmin⧽] (indefinite) [Move=⧼protect-level-ppadmin⧽] (indefinite))) |
||
| (20 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Jess Bell|Jess Bell]] based on the course by [https://members.physio-pedia.com/course_tutor/ibukun-afolabi/ Ibukun Afolabi]<br> | <div class="editorbox"> '''Original Editor '''- [[User:Jess Bell|Jess Bell]] based on the course by [https://members.physio-pedia.com/course_tutor/ibukun-afolabi/ Ibukun Afolabi]<br>'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== Introduction == | |||
This page aims to provide an introductory discussion of the physiotherapy assessment and treatment of the pelvic floor. Please note that further training is required through a reputable pelvic health education company before attempting the techniques discussed in this page. See the Resources section at the bottom of this page for links to pelvic and women's health special interest groups. | |||
== Clinic Environment == | == Clinic Environment == | ||
Before discussing the actual assessment and treatment of female pelvic health patients, it is useful to consider the environment in which you will be conducting your sessions. Where possible, it is important to be mindful of the clinic environment as the treatment setting has been shown to have an impact on a client’s health outcomes.<ref>Hesselink G, Smits M, Doedens M, Nijenhuis SMT, van Bavel D, van Goor H et al. [https://journals.sagepub.com/doi/full/10.1177/1937586719900885 Environmental needs, barriers, and facilitators for optimal healing in the postoperative process: a qualitative study of patients' lived experiences and perceptions]. HERD. 2020 Jul;13(3):125-39. </ref><ref>Huisman ERCM, Morales E, van Hoof J, Kort HSM. [https://www.sciencedirect.com/science/article/pii/S0360132312001758 Healing environment: A review of the impact of physical environmental factors on users]. Building and Environment. 2012;58:70-80.</ref><ref name=":0">Zborowsky T, Kreitzer MJ. Creating optimal healing environments in a health care setting [Internet]. Minnesota Medicine [cited 9 January 2022]. Available from: https://www.minnesotamedicine.com/clinical-health-affairs/creating-optimal-healing-environments-in-a-health-care-setting/</ref> The physical environment can help a client feel relaxed, safe and empowered or, conversely, feel stressed, threatened and tense.<ref name=":2">Afolabi I. Physiotherapy Assessment and Treatment of the Pelvic Floor Course. | Before discussing the actual assessment and treatment of female pelvic health patients, it is useful to consider the environment in which you will be conducting your sessions. Where possible, it is important to be mindful of the clinic environment as the treatment setting has been shown to have an impact on a client’s health outcomes.<ref name=":6">Hesselink G, Smits M, Doedens M, Nijenhuis SMT, van Bavel D, van Goor H et al. [https://journals.sagepub.com/doi/full/10.1177/1937586719900885 Environmental needs, barriers, and facilitators for optimal healing in the postoperative process: a qualitative study of patients' lived experiences and perceptions]. HERD. 2020 Jul;13(3):125-39. </ref><ref name=":7">Huisman ERCM, Morales E, van Hoof J, Kort HSM. [https://www.sciencedirect.com/science/article/pii/S0360132312001758 Healing environment: A review of the impact of physical environmental factors on users]. Building and Environment. 2012;58:70-80.</ref><ref name=":0">Zborowsky T, Kreitzer MJ. Creating optimal healing environments in a health care setting [Internet]. Minnesota Medicine [cited 9 January 2022]. Available from: https://www.minnesotamedicine.com/clinical-health-affairs/creating-optimal-healing-environments-in-a-health-care-setting/</ref> The physical environment can help a client feel relaxed, safe and empowered or, conversely, feel stressed, threatened and tense.<ref name=":2">Afolabi I. Physiotherapy Assessment and Treatment of the Pelvic Floor Course. Plus , 2022.</ref><ref name=":1">La Torre MA. Creating a healing environment. Perspectives in psychiatric care. 2006;42(4):262-4.</ref> For instance: | ||
* Daylight and windows have been shown to reduce fatigue and depression. Where this is not possible, indoor plants, aquariums, or nature-themed artworks can help to reduce stress<ref name=":0" /><ref name=":1" /> | * Daylight and windows have been shown to reduce fatigue and depression. Where this is not possible, indoor plants, aquariums, or nature-themed artworks can help to reduce stress<ref name=":0" /><ref name=":1" /> | ||
| Line 14: | Line 14: | ||
For more information on evidence-based design in healthcare settings, please have a look at the following articles: | For more information on evidence-based design in healthcare settings, please have a look at the following articles: | ||
* [https://journals.sagepub.com/doi/full/10.1177/1937586719900885 Environmental needs, barriers, and facilitators for optimal healing in the postoperative process: a qualitative study of patients' lived experiences and perceptions] | * [https://journals.sagepub.com/doi/full/10.1177/1937586719900885 Environmental needs, barriers, and facilitators for optimal healing in the postoperative process: a qualitative study of patients' lived experiences and perceptions]<ref name=":6" /> | ||
* [https://www.sciencedirect.com/science/article/pii/S0360132312001758 A review of the impact of physical environmental factors on users] | * [https://www.sciencedirect.com/science/article/pii/S0360132312001758 A review of the impact of physical environmental factors on users]<ref name=":7" /> | ||
* [https://www.minnesotamedicine.com/clinical-health-affairs/creating-optimal-healing-environments-in-a-health-care-setting/ Creating optimal healing environments in a health care setting] | * [https://www.minnesotamedicine.com/clinical-health-affairs/creating-optimal-healing-environments-in-a-health-care-setting/ Creating optimal healing environments in a health care setting]<ref name=":0" /> | ||
Creating a healing environment can be particularly important for women’s health clients as they may present with trauma, shame, embarrassment or other emotions associated with their condition.<ref name=":2" /> | Creating a healing environment can be particularly important for women’s health clients as they may present with trauma, shame, embarrassment or other emotions associated with their condition.<ref name=":2" /> | ||
| Line 25: | Line 25: | ||
* Validated outcome measures | * Validated outcome measures | ||
* Psychosocial inventories | * Psychosocial inventories | ||
There are many different | There are many different Patient Report Outcome measures (PROs) for pelvic floor dysfunction. They can be used to:<ref>Habashy E, Mahdy AE. Patient-reported outcome measures (PROMs) in pelvic floor disorders. Curr Urol Rep. 2019;20(5):22.</ref> | ||
* Screen for conditions | * Screen for conditions | ||
* Determine the impact of these conditions on an individual's quality of life | * Determine the impact of these conditions on an individual's quality of life | ||
* Evaluate the | * Evaluate the effectiveness of a treatment | ||
* Determine if an individual is satisfied with a treatment | * Determine if an individual is satisfied with a treatment | ||
The Pelvic Floor Disorders Consortium<ref>Bordeianou LG, Anger JT, Boutros M, Birnbaum E, Carmichael JC, Connell KA et al. [https://journals.lww.com/fpmrs/fulltext/2020/01000/measuring_pelvic_floor_disorder_symptoms_using.1.aspx Measuring pelvic floor disorder symptoms using patient-reported instruments: proceedings of the Consensus Meeting of the Pelvic Floor Consortium of the American Society of Colon and Rectal Surgeons, the International Continence Society, the American Urogynecologic Society, and the Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction]. Dis Colon Rectum. 2020;63(1):6-23.</ref> have found that the following outcome measures can be useful: | The Pelvic Floor Disorders Consortium<ref name=":8">Bordeianou LG, Anger JT, Boutros M, Birnbaum E, Carmichael JC, Connell KA et al. [https://journals.lww.com/fpmrs/fulltext/2020/01000/measuring_pelvic_floor_disorder_symptoms_using.1.aspx Measuring pelvic floor disorder symptoms using patient-reported instruments: proceedings of the Consensus Meeting of the Pelvic Floor Consortium of the American Society of Colon and Rectal Surgeons, the International Continence Society, the American Urogynecologic Society, and the Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction]. Dis Colon Rectum. 2020;63(1):6-23.</ref> have found that the following outcome measures can be useful: | ||
* Cleveland Clinic Florida Incontinence Score and the St. Mark’s Incontinence Score | * To assess the severity of faecal incontinence the [https://www.researchgate.net/figure/Cleveland-Clinic-Florida-Fecal-Incontinence-Score-CCFFIS_tbl4_311677789 Cleveland Clinic Florida Incontinence Score] and the [https://www.semanticscholar.org/paper/Does-the-St.-Mark%E2%80%99s-Incontinence-Score-Reflect-A-of-Maeda-Pares/e87710847198be092a826d3eb2519ca13fb074a7 St. Mark’s Incontinence Score] can be used together | ||
* Patient Assessment of Constipation and the Constipation Severity Instrument | * To assess the severity of constipation, the [https://www.dovepress.com/cr_data/article_fulltext/s32000/32684/img/DDDT-32684-T03.png Patient Assessment of Constipation] and the [https://www.semanticscholar.org/paper/The-Constipation-Severity-Instrument%3A-A-Validated-Varma-Wang/37565336421cbac35156c56ee736596738587387 Constipation Severity Instrument] can be used together | ||
* Short | * To assess stress and overflow incontinence, the [https://www.thecalculator.co/health/Urogenital-Distress-Inventory-Short-Form-(UDI-6)-Calculator-1127.html Short Form of the Urogenital Distress Inventory] can be used (this is in the final combined IMPACT tool discussed by Bordeianou et al.<ref name=":8" />) | ||
* Short | * The [[Pelvic Floor Distress Inventory (PFDI - 20)|Short Form of the Pelvic Floor Distress Inventory]], which is also in the final combined IMPACT tool, can be used to determine the impact of bowel and bladder dysfunction, and pelvic organ prolapse symptoms | ||
For more information on these outcomes, please see the full article [https://journals.lww.com/fpmrs/fulltext/2020/01000/measuring_pelvic_floor_disorder_symptoms_using.1.aspx here]. | For more information on these outcomes, please see the full article [https://journals.lww.com/fpmrs/fulltext/2020/01000/measuring_pelvic_floor_disorder_symptoms_using.1.aspx here]. | ||
== Subjective Evaluation == | == Subjective Evaluation == | ||
Like any physiotherapy session, you must first complete a subjective assessment | Like any physiotherapy session, you must first complete a subjective assessment. During this assessment, it is necessary to actively listen to your client and gain an understanding of why she is coming to see you.<ref name=":2" /> | ||
It has been suggested that motivational interviewing techniques may be beneficial for pelvic physiotherapy patients.<ref>Navarro-Brazález B, Vergara-Pérez F, Prieto-Gómez V, Sánchez-Sánchez B, Yuste-Sánchez MJ, Torres-Lacomba M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8706048/ What influences women to adhere to pelvic floor exercises after physiotherapy treatment? A qualitative study for individualized pelvic health care]. ''J Pers Med''. 2021;11(12):1368.</ref> Motivational interviewing is defined as:<blockquote>" | It has been suggested that motivational interviewing techniques may be beneficial for pelvic physiotherapy patients.<ref>Navarro-Brazález B, Vergara-Pérez F, Prieto-Gómez V, Sánchez-Sánchez B, Yuste-Sánchez MJ, Torres-Lacomba M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8706048/ What influences women to adhere to pelvic floor exercises after physiotherapy treatment? A qualitative study for individualized pelvic health care]. ''J Pers Med''. 2021;11(12):1368.</ref> Motivational interviewing is defined as:<blockquote>'''"A collaborative conversation style for strengthening a person's own motivation and commitment to change."'''<ref>Miller WR, Rollnick S. Motivational interviewing: helping people change. 3rd ed. New York: Guilford Press, 2013.</ref></blockquote>It is an evidence-based intervention that helps to encourage health behaviour change. It has been used in areas such as weight loss, smoking cessation, alcohol consumption, and blood sugar control.<ref>Kopp SL, Ramseier CA, Ratka-Krüger P, Woelber JP. Motivational Interviewing As an Adjunct to Periodontal Therapy-A Systematic Review. Front Psychol. 2017;8:279.</ref> It is also becoming more popular in physiotherapy practice.<ref>Lindson‐Hawley N, Thompson TP, Begh R. Motivational interviewing for smoking cessation. Cochrane Database of Systematic Reviews. 2015(3).</ref> To learn more about motivational interview, please click [https://members.physio-pedia.com/motivational-interviewing/ here]. | ||
<div class="row"> | <div class="row"> | ||
| Line 54: | Line 54: | ||
* Asking open-ended questions | * Asking open-ended questions | ||
* Being curious | * Being curious / enquiring questioning | ||
* Reflecting back to the client and summarising what has been said | * Reflecting back to the client and summarising what has been said | ||
* Listening without judgement | * Listening without judgement | ||
| Line 64: | Line 64: | ||
== Objective Evaluation of the External Body == | == Objective Evaluation of the External Body == | ||
The external evaluation helps you to understand how the wider systems or structures may relate to pelvic floor dysfunction. It can also help | The external evaluation helps you to understand how the wider systems or structures may relate to pelvic floor dysfunction. It can also help to increase your client’s trust in your physical handling of her body. | ||
While you may not be able to do everything in one session, you may choose to evaluate:<ref name=":2" /> | While you may not be able to do everything in one session, you may choose to evaluate:<ref name=":2" /> | ||
| Line 82: | Line 82: | ||
* The pressure system | * The pressure system | ||
* Motor control strategies | * Motor control strategies | ||
* Pelvic floor muscle function (externally) | * Pelvic floor muscle function (externally) | ||
== Objective Evaluation of the Pelvic Floor == | == Objective Evaluation of the Pelvic Floor == | ||
Please note that each country / state will have different rules and regulations about who can perform internal | Please note that each country / state will have different rules and regulations about who can perform an internal examination. Many areas require specific post-graduate training. Please make sure you are familiar with the regulations / requirements in your own area before performing an internal examination and make sure you complete the necessary training. | ||
According to Abe-Takahashi et al.,<ref>Abe-Takahashi Y, Kitta T, Ouchi M, Okayauchi M, Chiba H, Higuchi M et al. [https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-020-01127-x Reliability and validity of pelvic floor muscle strength assessment using the MizCure perineometer]. BMC Womens Health. 2020;20(1):257. </ref> the most common method of evaluating the pelvic floor muscles is digital vaginal penetration, which will be discussed below. | |||
Other methods include:<ref name=":2" /> | |||
* Real-time ultrasound: a safe, simple, cheap, and readily accessible technique<ref>Dietz HP. [https://link.springer.com/article/10.1007/s40137-013-0026-x Pelvic floor ultrasound]. ''Curr Surg Rep''. 2013;1:167-81.</ref> that can be used to assess pelvic floor contractions<ref>Thompson JA, O’Sullivan PB, Briffa K, Neumann P. Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. International Urogynecology Journal. 2005 Aug 1;16(4):285-92.</ref> | * Real-time ultrasound: a safe, simple, cheap, and readily accessible technique<ref>Dietz HP. [https://link.springer.com/article/10.1007/s40137-013-0026-x Pelvic floor ultrasound]. ''Curr Surg Rep''. 2013;1:167-81.</ref> that can be used to assess pelvic floor contractions<ref>Thompson JA, O’Sullivan PB, Briffa K, Neumann P. Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. International Urogynecology Journal. 2005 Aug 1;16(4):285-92.</ref> | ||
| Line 98: | Line 100: | ||
</div> | </div> | ||
If your client does proceed with an internal assessment, you should invite her feedback about what she is feeling. Ask about:<ref name=":2" /> | If your client does proceed with an internal assessment, you should invite her feedback about what she is feeling. | ||
Ask about:<ref name=":2" /> | |||
* Symptom reproduction | * Symptom reproduction | ||
| Line 108: | Line 112: | ||
Before the assessment, set up the treatment table with sheets for draping, gloves and lubricant. It is important to provide an opportunity for your client to remove her undergarments in private.<ref name=":2" /> | Before the assessment, set up the treatment table with sheets for draping, gloves and lubricant. It is important to provide an opportunity for your client to remove her undergarments in private.<ref name=":2" /> | ||
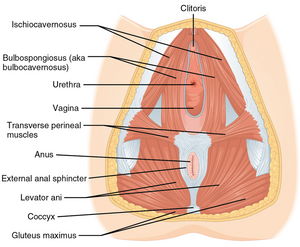
Remember to wash your hands prior to beginning the assessment. | Remember to wash your hands prior to beginning the assessment.[[File:Muscle of the Female Perineum.png|thumb|Figure 1. Muscles of the female perineum.]]'''During the assessment:'''<ref name=":2" /> | ||
'''During the assessment:'''<ref name=":2" /> | |||
* Observe the perineum, superficial pelvic floor muscles, vulva | * Observe the perineum, superficial pelvic floor muscles, vulva and then look at how the client reacts to palpation of these [[Overview of Female Pelvic Floor Muscle Anatomy and Physiology|superficial pelvic floor elements]] | ||
* Active tests | * Active tests | ||
** Provide cues to encourage pelvic floor engagement (e.g. “try to stop an imaginary stream of pee”) | ** Provide cues to encourage pelvic floor engagement (e.g. “try to stop an imaginary stream of pee”) | ||
| Line 122: | Line 124: | ||
*** The client is asked to perform another Valsalva manoeuvre and the speculum is slowly removed in order to assess apical descent | *** The client is asked to perform another Valsalva manoeuvre and the speculum is slowly removed in order to assess apical descent | ||
*** The anterior and posterior vaginal walls are then examined | *** The anterior and posterior vaginal walls are then examined | ||
*** Measurements may be taken and the prolapse can be classified (POP-Q)<ref name=":4" /> | *** Measurements may be taken and the prolapse can be classified (i.e. using the [[Pelvic Organ Prolapse Quantification (POP-Q) System|POP-Q]])<ref name=":4" /> | ||
* Then gently introduce one or two fingers into the introitus and assess tissues internally, from superficial to deep: | * Then gently introduce one or two fingers into the introitus and assess tissues internally, from superficial to deep checking for: | ||
** | ** Muscle tone | ||
** Spasm | |||
** Structure | |||
** Position | |||
** Compliance | |||
** Tissue quality | |||
** Tissue texture | |||
** Scarring | |||
** Tender areas | |||
** Partial / complete levator ani muscle avulsion | |||
* Assess muscle function | * Assess muscle function | ||
** Assess responsiveness, lift, range of motion, strength, endurance and coordination | ** Assess responsiveness, lift, range of motion, strength, endurance and coordination | ||
| Line 130: | Line 141: | ||
** Observe accessory muscle recruitment | ** Observe accessory muscle recruitment | ||
** Assess for strain or Valsalva with the cue to lift the pelvic floor | ** Assess for strain or Valsalva with the cue to lift the pelvic floor | ||
* It may be useful to check | * It may be useful to check, either vaginally or rectally, the impact of different actions, such as breathing, [[Transversus Abdominis|transversus abdominis]] engagement or coughing, on the pelvic floor | ||
* Pelvic floor muscle strength is graded using a Modified Oxford Grading Scale:<ref name=":3" /><ref>Chevalier F, Fernandez-Lao C, Cuesta-Vargas AI. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4251926/ Normal reference values of strength in pelvic floor muscle of women: a descriptive and inferential study]. ''BMC Womens Health''. 2014;14:143. </ref> | * Pelvic floor muscle strength is graded using a Modified Oxford Grading Scale:<ref name=":3" /><ref>Chevalier F, Fernandez-Lao C, Cuesta-Vargas AI. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4251926/ Normal reference values of strength in pelvic floor muscle of women: a descriptive and inferential study]. ''BMC Womens Health''. 2014;14:143. </ref> | ||
** 0 = no contraction | ** 0 = no contraction | ||
| Line 142: | Line 153: | ||
{{#ev:youtube|b19x9AVCUgc}}<ref>OBGYN Academy. Assessment of the Pelvic Floor Musculature. Available from: https://www.youtube.com/watch?v=b19x9AVCUgc [last accessed 9/1/2022]</ref> | {{#ev:youtube|b19x9AVCUgc}}<ref>OBGYN Academy. Assessment of the Pelvic Floor Musculature. Available from: https://www.youtube.com/watch?v=b19x9AVCUgc [last accessed 9/1/2022]</ref> | ||
During an internal examination, you will typically have your client | During an internal examination, you will typically have your client hook-lying or side-lying.<ref name=":2" /> You can, however, also assess specific elements of pelvic floor muscle function in standing.<ref name=":2" /><ref>Bø K, Finckenhagen HB. [https://obgyn.onlinelibrary.wiley.com/doi/full/10.1046/j.1600-0412.2003.00240.x Is there any difference in measurement of pelvic floor muscle strength in supine and standing position?] Acta Obstet Gynecol Scand. 2003;82(12):1120-4. </ref> Because standing is a more functional position, it can provide a more accurate understanding of how the pelvic floor functions in relation to gravity or under load. | ||
== Treatment == | == Treatment == | ||
| Line 169: | Line 180: | ||
* Re-mapping the brain | * Re-mapping the brain | ||
* Pain management strategies | * Pain management strategies | ||
* Acupuncture or dry needling | * Acupuncture or dry needling | ||
It is important to adopt a bio-psycho-social-spiritual lens when working with women. Exploring how emotional health, mental health, relational health | It is important to adopt a bio-psycho-social-spiritual lens when working with women. Exploring how emotional health, mental health, relational health and spiritual health influence physical health is vital in these patients. Alongside this, it is important to consider how factors such as sleep, nutrition, hydration and movement, interact when working to restore pelvic health.<ref name=":2" /> | ||
== Specific Bladder and Bowel Retraining Techniques == | |||
=== Urinary Incontinence === | |||
Conservative approaches to managing urinary incontinence include behavioural and lifestyle modifications, pelvic floor retraining and using specific mechanical devices.<ref name=":5">Robert M. Ross S. No. 186-Conservative Management of Urinary Incontinence. Journal of Obstetrics and Gynaecology Canada. 2018;40(2):e119-e125.</ref> | |||
Specific techniques include:<ref name=":5" /> | |||
* [[Kegel's Exercise : Females|Kegel exercises]] | * [[Kegel's Exercise : Females|Kegel exercises]] | ||
| Line 189: | Line 194: | ||
* Vaginal cones (specifically for stress incontinence) | * Vaginal cones (specifically for stress incontinence) | ||
==== Overactive Bladder | {{#ev:youtube|l_PM-wN116Q}}<ref>AskDoctorJo. Stop Stress Urinary Incontinence With 5 Easy Exercises. Available from: https://www.youtube.com/watch?v=l_PM-wN116Q [last accessed 25/1/2022]</ref> | ||
Initial treatment for overactive bladder will include pharmacological therapy, bladder retraining, pelvic floor exercises and lifestyle modification.<ref>Abdel-Fattah M, Chapple C, Guerrero K, Dixon S, Cotterill N, Ward K et al. [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05661-3#Abs1 Female Urgency, Trial of Urodynamics as Routine Evaluation (FUTURE study): a superiority randomised clinical trial to evaluate the effectiveness and cost-effectiveness of invasive urodynamic investigations in management of women with refractory overactive bladder symptoms]. Trials. 2021;22(1):745. </ref> In particular, the focus may be on fluid modification, | |||
=== Overactive Bladder === | |||
Initial treatment for overactive bladder will include pharmacological therapy, bladder retraining, pelvic floor exercises and lifestyle modification.<ref>Abdel-Fattah M, Chapple C, Guerrero K, Dixon S, Cotterill N, Ward K et al. [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05661-3#Abs1 Female Urgency, Trial of Urodynamics as Routine Evaluation (FUTURE study): a superiority randomised clinical trial to evaluate the effectiveness and cost-effectiveness of invasive urodynamic investigations in management of women with refractory overactive bladder symptoms]. Trials. 2021;22(1):745. </ref> In particular, the focus may be on fluid modification, avoiding potential triggers and bladder retraining.<ref>Basu M. Management of overactive bladder. Obstetrics, Gynaecology & Reproductive Medicine. 2020;30(1:1-5.</ref> | |||
{{#ev:youtube|14OSCEA0Fgk}}<ref>St George's University Hospitals NHS Foundation Trust. Bladder Retraining. https://www.youtube.com/watch?v=14OSCEA0Fgk [last accessed 25/1/2022]</ref> | |||
=== Constipation === | |||
It has been found that using a foot stool is an effective method to encourage defecation in constipated patients. Patients should also be encouraged to adopt a position where the upper body is bent forward.<ref>Takano S. Nakashima M. Tsuchino M. Nakao Y. Watanabe A. Influence of foot stool on defecation : a prospective study. Pelviperineology. 2018;37:101-3.</ref> | |||
{{#ev:youtube|QDk93cvZAuk}}<ref>Michelle Kenway. Natural Constipation Relief in 3 Easy Steps ("MOO to POO"). Available from: https://www.youtube.com/watch?v=QDk93cvZAuk [last accessed 25/1/2022]</ref> | |||
== Resources - Pelvic Physiotherapy Special Interest Groups == | |||
* '''Australia''' | |||
** [https://australian.physio/membership/national-groups/womens-mens-and-pelvic-health Australian Physiotherapy Association - Women's, Men's and Pelvic Health] | |||
* '''Canada''' | |||
** [https://www.womenshealthcpa.com/ Canadian Physiotherapy Association - Women's Health] | |||
* '''New Zealand''' | |||
** [https://pnz.org.nz/pwmh Physiotherapy New Zealand - Pelvic Womens and Mens Health] | |||
* '''South Africa''' | |||
** [https://www.saphysio.co.za/membership-groups/special-interest-groups/pelvic-womens-health-physiotherapy-group/ South African Society of Physiotherapists - Pelvic and Women's Health Physiotherapy Group] | |||
* '''United Kingdom''' | |||
** [https://thepogp.co.uk/ Pelvic Obstetric and Gynaecological Physiotherapy] | |||
* '''United States''' | |||
**[https://aptapelvichealth.org/ American Physical Therapy Assocation - Pelvic health] | |||
* '''World Physiotherapy''' | |||
** [https://world.physio/subgroups/pelvic-womens-health International Organization of Physical Therapists in Pelvic and Women's Health (IOPTPWH)] | |||
== References == | == References == | ||
[[Category: | [[Category:Plus Content]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Womens Health]] | [[Category:Womens Health]] | ||
[[Category:Pelvic Health]] | [[Category:Pelvic Health]] | ||
Latest revision as of 07:00, 23 November 2022
Top Contributors - Jess Bell, Kim Jackson, Tarina van der Stockt, Carin Hunter and Nupur Smit Shah
Introduction[edit | edit source]
This page aims to provide an introductory discussion of the physiotherapy assessment and treatment of the pelvic floor. Please note that further training is required through a reputable pelvic health education company before attempting the techniques discussed in this page. See the Resources section at the bottom of this page for links to pelvic and women's health special interest groups.
Clinic Environment[edit | edit source]
Before discussing the actual assessment and treatment of female pelvic health patients, it is useful to consider the environment in which you will be conducting your sessions. Where possible, it is important to be mindful of the clinic environment as the treatment setting has been shown to have an impact on a client’s health outcomes.[1][2][3] The physical environment can help a client feel relaxed, safe and empowered or, conversely, feel stressed, threatened and tense.[4][5] For instance:
- Daylight and windows have been shown to reduce fatigue and depression. Where this is not possible, indoor plants, aquariums, or nature-themed artworks can help to reduce stress[3][5]
- The colour scheme can also have an impact:[5]
- Blue and green can promote relaxation and balance
- Yellow and orange can energise or activate a space
For more information on evidence-based design in healthcare settings, please have a look at the following articles:
- Environmental needs, barriers, and facilitators for optimal healing in the postoperative process: a qualitative study of patients' lived experiences and perceptions[1]
- A review of the impact of physical environmental factors on users[2]
- Creating optimal healing environments in a health care setting[3]
Creating a healing environment can be particularly important for women’s health clients as they may present with trauma, shame, embarrassment or other emotions associated with their condition.[4]
The Initial Assessment[edit | edit source]
Prior to the initial assessment, it can be helpful to collect some initial information about your client by sending them:[4]
- Forms and questionnaires
- Validated outcome measures
- Psychosocial inventories
There are many different Patient Report Outcome measures (PROs) for pelvic floor dysfunction. They can be used to:[6]
- Screen for conditions
- Determine the impact of these conditions on an individual's quality of life
- Evaluate the effectiveness of a treatment
- Determine if an individual is satisfied with a treatment
The Pelvic Floor Disorders Consortium[7] have found that the following outcome measures can be useful:
- To assess the severity of faecal incontinence the Cleveland Clinic Florida Incontinence Score and the St. Mark’s Incontinence Score can be used together
- To assess the severity of constipation, the Patient Assessment of Constipation and the Constipation Severity Instrument can be used together
- To assess stress and overflow incontinence, the Short Form of the Urogenital Distress Inventory can be used (this is in the final combined IMPACT tool discussed by Bordeianou et al.[7])
- The Short Form of the Pelvic Floor Distress Inventory, which is also in the final combined IMPACT tool, can be used to determine the impact of bowel and bladder dysfunction, and pelvic organ prolapse symptoms
For more information on these outcomes, please see the full article here.
Subjective Evaluation[edit | edit source]
Like any physiotherapy session, you must first complete a subjective assessment. During this assessment, it is necessary to actively listen to your client and gain an understanding of why she is coming to see you.[4]
It has been suggested that motivational interviewing techniques may be beneficial for pelvic physiotherapy patients.[8] Motivational interviewing is defined as:
"A collaborative conversation style for strengthening a person's own motivation and commitment to change."[9]
It is an evidence-based intervention that helps to encourage health behaviour change. It has been used in areas such as weight loss, smoking cessation, alcohol consumption, and blood sugar control.[10] It is also becoming more popular in physiotherapy practice.[11] To learn more about motivational interview, please click here.
Other techniques that can be helpful during the subjective interview include:[4]
- Asking open-ended questions
- Being curious / enquiring questioning
- Reflecting back to the client and summarising what has been said
- Listening without judgement
- Aiming to understand goals and what success would mean for the client
- Finding out about the impact of the client's condition on her life, work, relationships, emotions etc
- Asking about the client’s theories in order to gain insight into her beliefs about her condition
Establishing rapport, cultivating trust and safety and allowing the patient to feel heard are key goals of the initial assessment.[4]
Objective Evaluation of the External Body[edit | edit source]
The external evaluation helps you to understand how the wider systems or structures may relate to pelvic floor dysfunction. It can also help to increase your client’s trust in your physical handling of her body.
While you may not be able to do everything in one session, you may choose to evaluate:[4]
- Alignment
- Posture
- Movement patterns
- Breathing strategies
- Neural screen
- Abdominal wall function
- Abdominal viscera
- Spinal, hip, pelvic movements and range of motion
- Muscle strength and endurance
- Thorax
- Myofascial quality
- External scars
- The pressure system
- Motor control strategies
- Pelvic floor muscle function (externally)
Objective Evaluation of the Pelvic Floor[edit | edit source]
Please note that each country / state will have different rules and regulations about who can perform an internal examination. Many areas require specific post-graduate training. Please make sure you are familiar with the regulations / requirements in your own area before performing an internal examination and make sure you complete the necessary training.
According to Abe-Takahashi et al.,[14] the most common method of evaluating the pelvic floor muscles is digital vaginal penetration, which will be discussed below.
Other methods include:[4]
- Real-time ultrasound: a safe, simple, cheap, and readily accessible technique[15] that can be used to assess pelvic floor contractions[16]
- Perineometer: a simple, minimally invasive, low-cost tool that is used to measure pressure changes in the vagina after a voluntary contraction of the pelvic floor muscles[17]
Before evaluating the pelvic floor, you must discuss with your client the purpose of the examination and explain what is involved, including the risks, benefits and alternatives in order to obtain informed consent. Your client may choose to decline an internal assessment.[4]
If your client does proceed with an internal assessment, you should invite her feedback about what she is feeling.
Ask about:[4]
- Symptom reproduction
- Pain
- Pressure
- Sensitivity
- Referral patterns
Before the assessment, set up the treatment table with sheets for draping, gloves and lubricant. It is important to provide an opportunity for your client to remove her undergarments in private.[4]
Remember to wash your hands prior to beginning the assessment.
During the assessment:[4]
- Observe the perineum, superficial pelvic floor muscles, vulva and then look at how the client reacts to palpation of these superficial pelvic floor elements
- Active tests
- Provide cues to encourage pelvic floor engagement (e.g. “try to stop an imaginary stream of pee”)
- Assess for pelvic organ prolapse if appropriate (see below)
- A detailed discussion of the examination and assessment of pelvic organ prolapse is available here
- If a prolapse is suspected, a pelvic examination is required to determine the location / extent of the prolapse. The medical assessment is described as follows by Inglesia et al:[20]
- The vaginal opening and perineal body are observed while the client does a Valsalva manoeuvre
- A speculum is used to assess the vaginal apex (cervix or vaginal cuff) and vaginal length is recorded
- The client is asked to perform another Valsalva manoeuvre and the speculum is slowly removed in order to assess apical descent
- The anterior and posterior vaginal walls are then examined
- Measurements may be taken and the prolapse can be classified (i.e. using the POP-Q)[20]
- Then gently introduce one or two fingers into the introitus and assess tissues internally, from superficial to deep checking for:
- Muscle tone
- Spasm
- Structure
- Position
- Compliance
- Tissue quality
- Tissue texture
- Scarring
- Tender areas
- Partial / complete levator ani muscle avulsion
- Assess muscle function
- Assess responsiveness, lift, range of motion, strength, endurance and coordination
- Compare sides
- Observe accessory muscle recruitment
- Assess for strain or Valsalva with the cue to lift the pelvic floor
- It may be useful to check, either vaginally or rectally, the impact of different actions, such as breathing, transversus abdominis engagement or coughing, on the pelvic floor
- Pelvic floor muscle strength is graded using a Modified Oxford Grading Scale:[17][21]
- 0 = no contraction
- 1 = a flicker
- 2 = weak
- 3 = moderate contraction with a lift
- 4 = good contraction with a lift
- 5 = strong contraction with a lift
The following video demonstrates a pelvic floor examination. Please click through to watch this video on YouTube if you want to find out more.
During an internal examination, you will typically have your client hook-lying or side-lying.[4] You can, however, also assess specific elements of pelvic floor muscle function in standing.[4][23] Because standing is a more functional position, it can provide a more accurate understanding of how the pelvic floor functions in relation to gravity or under load.
Treatment[edit | edit source]
The treatment strategy must relate to the client’s goals and focus on what is important to her. This can help to encourage overall engagement. It is also important to encourage a client to feel connected to her body and feel that she has the power to change her system.[4]
The initial treatment begins with awareness and increasing somatic awareness. This mind-body reconnection strategy is significant because women with pelvic floor conditions may have some “disconnect” to their pelvic floor. Awakening / reconnecting the pelvic floor is, therefore, a necessary starting point.[4]
After reconnecting, it is possible to start to create a supple, dynamic, flexible, healthy, pain-free, strong, and resilient pelvic floor.[4]
Treatment may focus on the following:[4]
- Education
- Increasing somatic awareness
- Neuromuscular facilitation
- Improving pelvic biomechanics and synergies
- Improving flexibility and mobility of the pelvic floor muscles
- Increasing endurance and functional strength
- Integrated inner core retraining
- Teaching pressure management strategies
- Bladder and bowel retraining
- Manual therapy techniques
- Myofascial work
- Breath work
- Motor control training
- Down-regulating the nervous system
- Re-mapping the brain
- Pain management strategies
- Acupuncture or dry needling
It is important to adopt a bio-psycho-social-spiritual lens when working with women. Exploring how emotional health, mental health, relational health and spiritual health influence physical health is vital in these patients. Alongside this, it is important to consider how factors such as sleep, nutrition, hydration and movement, interact when working to restore pelvic health.[4]
Specific Bladder and Bowel Retraining Techniques[edit | edit source]
Urinary Incontinence[edit | edit source]
Conservative approaches to managing urinary incontinence include behavioural and lifestyle modifications, pelvic floor retraining and using specific mechanical devices.[24]
Specific techniques include:[24]
- Kegel exercises
- Functional electrical stimulation (FES) may be a useful adjunct to pelvic floor retraining
- Vaginal cones (specifically for stress incontinence)
Overactive Bladder[edit | edit source]
Initial treatment for overactive bladder will include pharmacological therapy, bladder retraining, pelvic floor exercises and lifestyle modification.[26] In particular, the focus may be on fluid modification, avoiding potential triggers and bladder retraining.[27]
Constipation[edit | edit source]
It has been found that using a foot stool is an effective method to encourage defecation in constipated patients. Patients should also be encouraged to adopt a position where the upper body is bent forward.[29]
Resources - Pelvic Physiotherapy Special Interest Groups[edit | edit source]
- Australia
- Canada
- New Zealand
- South Africa
- United Kingdom
- United States
- World Physiotherapy
References[edit | edit source]
- ↑ 1.0 1.1 Hesselink G, Smits M, Doedens M, Nijenhuis SMT, van Bavel D, van Goor H et al. Environmental needs, barriers, and facilitators for optimal healing in the postoperative process: a qualitative study of patients' lived experiences and perceptions. HERD. 2020 Jul;13(3):125-39.
- ↑ 2.0 2.1 Huisman ERCM, Morales E, van Hoof J, Kort HSM. Healing environment: A review of the impact of physical environmental factors on users. Building and Environment. 2012;58:70-80.
- ↑ 3.0 3.1 3.2 Zborowsky T, Kreitzer MJ. Creating optimal healing environments in a health care setting [Internet]. Minnesota Medicine [cited 9 January 2022]. Available from: https://www.minnesotamedicine.com/clinical-health-affairs/creating-optimal-healing-environments-in-a-health-care-setting/
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 Afolabi I. Physiotherapy Assessment and Treatment of the Pelvic Floor Course. Plus , 2022.
- ↑ 5.0 5.1 5.2 La Torre MA. Creating a healing environment. Perspectives in psychiatric care. 2006;42(4):262-4.
- ↑ Habashy E, Mahdy AE. Patient-reported outcome measures (PROMs) in pelvic floor disorders. Curr Urol Rep. 2019;20(5):22.
- ↑ 7.0 7.1 Bordeianou LG, Anger JT, Boutros M, Birnbaum E, Carmichael JC, Connell KA et al. Measuring pelvic floor disorder symptoms using patient-reported instruments: proceedings of the Consensus Meeting of the Pelvic Floor Consortium of the American Society of Colon and Rectal Surgeons, the International Continence Society, the American Urogynecologic Society, and the Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction. Dis Colon Rectum. 2020;63(1):6-23.
- ↑ Navarro-Brazález B, Vergara-Pérez F, Prieto-Gómez V, Sánchez-Sánchez B, Yuste-Sánchez MJ, Torres-Lacomba M. What influences women to adhere to pelvic floor exercises after physiotherapy treatment? A qualitative study for individualized pelvic health care. J Pers Med. 2021;11(12):1368.
- ↑ Miller WR, Rollnick S. Motivational interviewing: helping people change. 3rd ed. New York: Guilford Press, 2013.
- ↑ Kopp SL, Ramseier CA, Ratka-Krüger P, Woelber JP. Motivational Interviewing As an Adjunct to Periodontal Therapy-A Systematic Review. Front Psychol. 2017;8:279.
- ↑ Lindson‐Hawley N, Thompson TP, Begh R. Motivational interviewing for smoking cessation. Cochrane Database of Systematic Reviews. 2015(3).
- ↑ Clinical Advisor. How to Use Motivational Interviewing to Encourage Behavior Change. Available from: https://www.youtube.com/watch?v=6t3tU8-OA1M[last accessed 9/1/2022]
- ↑ Bill Matulich. Introduction to Motivational Interviewing. Available from: https://www.youtube.com/watch?v=s3MCJZ7OGRk [last accessed 9/1/2022]]
- ↑ Abe-Takahashi Y, Kitta T, Ouchi M, Okayauchi M, Chiba H, Higuchi M et al. Reliability and validity of pelvic floor muscle strength assessment using the MizCure perineometer. BMC Womens Health. 2020;20(1):257.
- ↑ Dietz HP. Pelvic floor ultrasound. Curr Surg Rep. 2013;1:167-81.
- ↑ Thompson JA, O’Sullivan PB, Briffa K, Neumann P. Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. International Urogynecology Journal. 2005 Aug 1;16(4):285-92.
- ↑ 17.0 17.1 Angelo PH, Varella LRD, de Oliveira MCE, Matias M, de Azevedo M., de Almeida et al. A manometry classification to assess pelvic floor muscle function in women. PLoS One. 2017;12(10):e0187045.
- ↑ Lifecare Pilates. Using Real Time Ultrasound Imaging to assess Pelvic floor function. Available from: https://www.youtube.com/watch?v=nrt7SqoUSZ4 [last accessed 9/1/2022]
- ↑ CityImaging. Pelvic Floor Assessment by Ultrasound. Available from: https://www.youtube.com/watch?v=6VDe8kI2W5c [last accessed 9/1/2022]
- ↑ 20.0 20.1 Iglesia CB, Smithling KR. Pelvic organ prolapse. Am Fam Physician. 2017;96(3):179-85.
- ↑ Chevalier F, Fernandez-Lao C, Cuesta-Vargas AI. Normal reference values of strength in pelvic floor muscle of women: a descriptive and inferential study. BMC Womens Health. 2014;14:143.
- ↑ OBGYN Academy. Assessment of the Pelvic Floor Musculature. Available from: https://www.youtube.com/watch?v=b19x9AVCUgc [last accessed 9/1/2022]
- ↑ Bø K, Finckenhagen HB. Is there any difference in measurement of pelvic floor muscle strength in supine and standing position? Acta Obstet Gynecol Scand. 2003;82(12):1120-4.
- ↑ 24.0 24.1 Robert M. Ross S. No. 186-Conservative Management of Urinary Incontinence. Journal of Obstetrics and Gynaecology Canada. 2018;40(2):e119-e125.
- ↑ AskDoctorJo. Stop Stress Urinary Incontinence With 5 Easy Exercises. Available from: https://www.youtube.com/watch?v=l_PM-wN116Q [last accessed 25/1/2022]
- ↑ Abdel-Fattah M, Chapple C, Guerrero K, Dixon S, Cotterill N, Ward K et al. Female Urgency, Trial of Urodynamics as Routine Evaluation (FUTURE study): a superiority randomised clinical trial to evaluate the effectiveness and cost-effectiveness of invasive urodynamic investigations in management of women with refractory overactive bladder symptoms. Trials. 2021;22(1):745.
- ↑ Basu M. Management of overactive bladder. Obstetrics, Gynaecology & Reproductive Medicine. 2020;30(1:1-5.
- ↑ St George's University Hospitals NHS Foundation Trust. Bladder Retraining. https://www.youtube.com/watch?v=14OSCEA0Fgk [last accessed 25/1/2022]
- ↑ Takano S. Nakashima M. Tsuchino M. Nakao Y. Watanabe A. Influence of foot stool on defecation : a prospective study. Pelviperineology. 2018;37:101-3.
- ↑ Michelle Kenway. Natural Constipation Relief in 3 Easy Steps ("MOO to POO"). Available from: https://www.youtube.com/watch?v=QDk93cvZAuk [last accessed 25/1/2022]