American Spinal Injury Association (ASIA) Impairment Scale: Difference between revisions
No edit summary |
No edit summary |
||
| Line 24: | Line 24: | ||
== Sensory Examination == | == Sensory Examination == | ||
Key [https://asia-spinalinjury.org/wp-content/uploads/2016/02/Key_Sensory_Points.pdf sensory points] are readily located in relation to bony anatomical landmarks in the dermatomes C2 - S5. They are tested bilaterally using light touch (LT) and pin-prick (PP) [sharp | Key [https://asia-spinalinjury.org/wp-content/uploads/2016/02/Key_Sensory_Points.pdf sensory points] are readily located in relation to bony anatomical landmarks in the dermatomes C2 - S5. They are tested bilaterally using light touch (LT) and pin-prick (PP) [sharp/dull discrimination]. Equipment common to clinical settings are used, such as a cotton tip applicator for light touch and either a neuro-tip or safety pin for pin-prick. Appreciation of light touch and pin prick sensation at each of the key points is made in comparison to sensation on the patient’s cheek as a normal frame of reference.<ref name="Burns et al" /> | ||
'''Sensory examination | '''Sensory examination performance tips:''' | ||
* Light touch sensation is tested | * '''Light touch sensation''' is tested a wisp of cotton stroked once across an area not to exceed 1cm of skin while the patient maintains eyes closed or has their vision blocked. | ||
* Pin prick sensation (sharp/dull discrimination) is performed with a disposable safety pin | * '''Pin-prick sensation''' (sharp/dull discrimination) is performed with a disposable safety pin; using the pointed end to test for sharp and the rounded end of the pin for dull. | ||
** In testing for pin-prick appreciation, the examiner must determine if the patient can correctly and reliably discriminate between sharp and dull sensation at each key sensory point. If in doubt, 8 out of 10 correct answers are suggested as a standard for accuracy; as this reduces the probability of correct guessing to less than 5%. | |||
** A score of 0 is recorded for inability to distinguish between dull and sharp sensation or when the patient is unable to feel when being touched by the pin. | |||
** A score of 1 is recorded when sharp/dull sensation is impaired. In this case, the patient reliably distinguishes between the sharp and dull ends of the pin, but states that the intensity of sharpness is different in the key sensory point than the feeling of sharpness on the face. The intensity may be greater or lesser than the feeling on the face. | |||
'''A three-point scale is used for scoring:''' | '''A three-point scale is used for scoring:''' | ||
Revision as of 22:00, 18 June 2023
Original Editor - Daphne Jackson.
Top Contributors - Naomi O'Reilly, Arnold Fredrick D'Souza, Stacy Schiurring, Kim Jackson, Jess Bell, Admin, Abbey Wright, Olajumoke Ogunleye, Tarina van der Stockt and Rucha Gadgil
Introduction[edit | edit source]
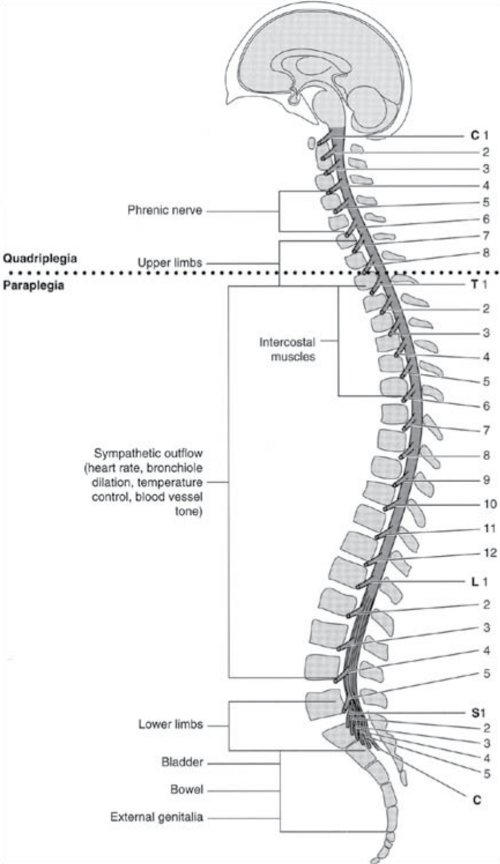
A traumatic spinal cord injury is a life changing event which can have a physical and emotional impairments for patients. The global incidence of traumatic spinal injury is approximately 10.5 cases per 100,000 persons. According to a 2022 systematic review and meta-analysis, the incidence of traumatic spinal injuries occurs in greater numbers in countries with low and middle income (13.69 per 100,000 persons) compared to countries with high income (8.72 per 100,000 persons).[1]
For a review of spinal cord injury, please read this article.
Spinal Cord Injury can severely impair or cease the conduction of sensory and motor signals, as well as functions of the autonomic nervous system. A systematic examination of dermatomes and myotomes, thus, would allow a clinician to determine the affected segments of the spinal cord.
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI), commonly referred to as the ASIA Exam, was developed by the American Spinal Injury Association (ASIA).[2]
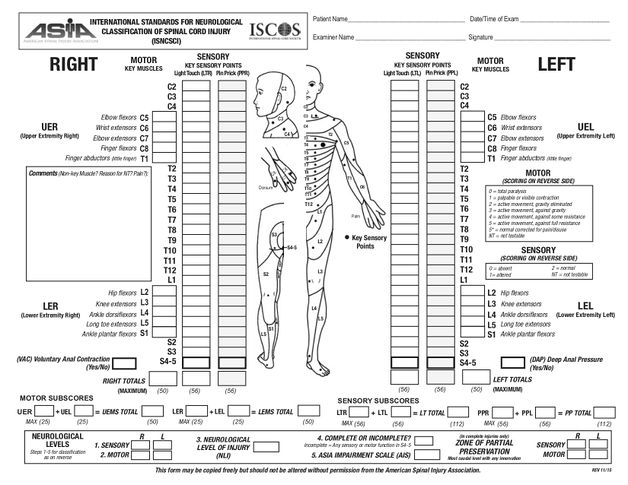
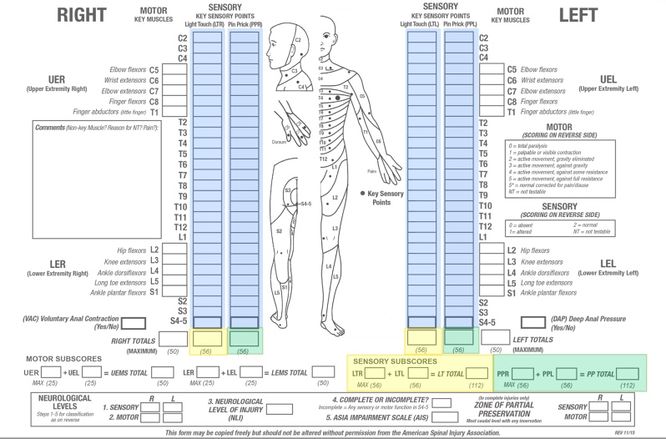
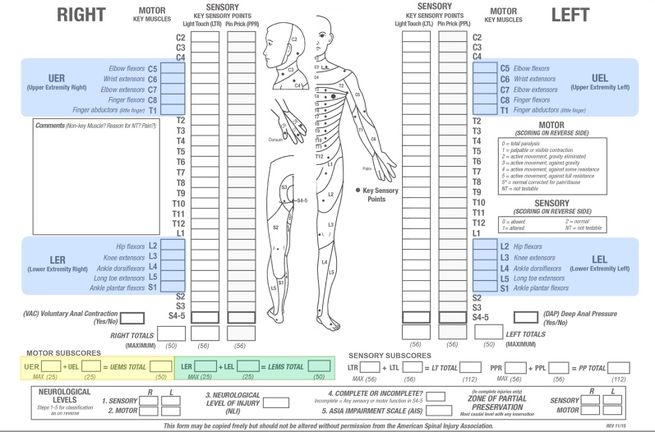
The ASIA exam is a standardised physical examination consisting of a (1) myotomal-based motor examination, (2) dermatomal-based sensory examination, and (3) an anorectal examination. Upon completion of these three components, an injury grade and level are assigned. This designation can then be used for rehabilitation prognosis, to guide treatment interventions, and aid in multidisciplinary communication.
The aim of the ASIA scale is to provide (1) standardized and detailed documentation of the SCI neurological level of injury, (2) guidance for radiographic assessment and treatment, and (3) to determine if the SCI is complete or incomplete.[3]
Sensory Examination[edit | edit source]
Key sensory points are readily located in relation to bony anatomical landmarks in the dermatomes C2 - S5. They are tested bilaterally using light touch (LT) and pin-prick (PP) [sharp/dull discrimination]. Equipment common to clinical settings are used, such as a cotton tip applicator for light touch and either a neuro-tip or safety pin for pin-prick. Appreciation of light touch and pin prick sensation at each of the key points is made in comparison to sensation on the patient’s cheek as a normal frame of reference.[3]
Sensory examination performance tips:
- Light touch sensation is tested a wisp of cotton stroked once across an area not to exceed 1cm of skin while the patient maintains eyes closed or has their vision blocked.
- Pin-prick sensation (sharp/dull discrimination) is performed with a disposable safety pin; using the pointed end to test for sharp and the rounded end of the pin for dull.
- In testing for pin-prick appreciation, the examiner must determine if the patient can correctly and reliably discriminate between sharp and dull sensation at each key sensory point. If in doubt, 8 out of 10 correct answers are suggested as a standard for accuracy; as this reduces the probability of correct guessing to less than 5%.
- A score of 0 is recorded for inability to distinguish between dull and sharp sensation or when the patient is unable to feel when being touched by the pin.
- A score of 1 is recorded when sharp/dull sensation is impaired. In this case, the patient reliably distinguishes between the sharp and dull ends of the pin, but states that the intensity of sharpness is different in the key sensory point than the feeling of sharpness on the face. The intensity may be greater or lesser than the feeling on the face.
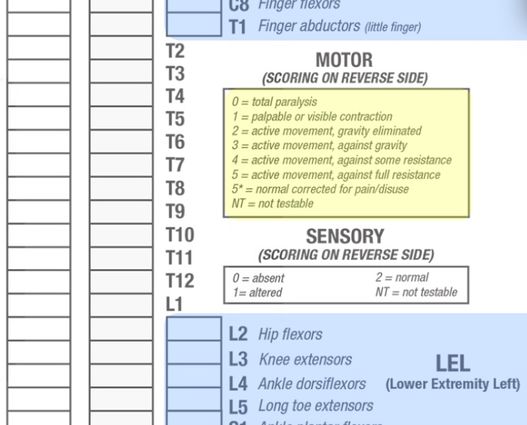
A three-point scale is used for scoring:
| 0 | = | Absent |
| 1 | = | Altered - Impaired or Partial Appreciation, including Hyperesthesia |
| 2 | = | Normal or Intact - Similar as on the Cheek |
| NT | = | Not Testable |
Not testable is recorded when a key sensory point is not able to be assessed for any reason, such as a cast, burn, or amputation. When this occurs, the sensory scores for that side of the body and the total sensory score cannot be determined. The neurological level should still be determined as accurately as possible, however the sensory score and impairment grade (discussed below) should be retested and determined at a later date.
| Level | Description of Key Points for Sensory Testing |
|---|---|
| C2 | 1 cm lateral to Occipital Protuberance |
| C3 | Supraclavicular Fossa at Midclavicular Line |
| C4 | Over Acromioclavicular Joint |
| C5 | Lateral Side Antecubital Fossa just Proximal to Elbow Crease |
| C6 | Dorsal Surface of Proximal Phalanx of the Thumb |
| C7 | Dorsal Surface of Proximal Phalanx of the Middle Finger |
| C8 | Dorsal Surface of Proximal Phalanx of the Little Finger |
| T1 | Medial Side Antecubital Fossa, just Proximal to Medical Epicondyle of Humerus |
| T2 | Apex of Axilla |
| T3 | Midclavicular Line and 3rd Intercostal Space |
| T4 | Midclavicular Line and 4th Intercostal Space at Nipple Line |
| T5 | Midclavicular Line and 5th Intercostal Space Midway between T4 & T6 |
| T6 | Midclavicular Line and 6th Intercostal Space at the level of Xiphisternum |
| T7 | Midclavicular Line and 7th Intercostal Space Midway between T6 & T8 - Quarter Distance between Level Xiphisternum & Umbilicus |
| T8 | Midclavicular Line and 8th Intercostal Space Midway between T6 & T10- Half Distance between Level Xiphisternum & Umbilicus |
| T9 | Midclavicular Line and 9th Intercostal Space Midway between T8 & T10 - Three Quarters Distance between Level Xiphisternum & Umbilicus |
| T10 | Midclavicular Line and 10th Intercostal Space at the Level of Umbilicus |
| T11 | Midclavicular Line and 11th Intercostal Space Midway between T10 & T12 - Midway between Level of Umbilicus & Inguinal Ligament |
| T12 | Midclavicular Line Over Midpoint Inguinal Ligament |
| L1 | Midway between Sensory Point at T12 & L1 |
| L2 | Anterior-Medial Thigh at the Midpoint drawn connecting Midpoint of Inguinal Ligament & Medial Femoral Condyle |
| L3 | Medial femoral Condyle above the Knee |
| L4 | Medial Malleolus |
| L5 | Dorsal Foot at 3rd Metatarsal Phalangeal Joint |
| S1 | Lateral Aspect of Calcaneus |
| S2 | Midpoint of Popliteal Fossa |
| S3 | Over Ischial Tuberosity or Infragluteal Fold |
| S4 - 5 | Perianal Area < 1cm Lateral to Mucocutaneous Junction |
Information in the above table is adapted from the 2011 version of International Standards for Neurological Classification of Spinal Cord Injury.[3]
| Deep Anal Pressure (DAP) |
|---|
| The examiner’s gloved and lubricated index finger applies a gentle pressure to the internal anorectal wall which is innervated by the somatosensory components of the pudendal nerve S4/5. Perceived pressure is graded as absent or present. Any reproducible pressure sensation felt in the anal area during this part of the exam signifies that the patient has a sensory incomplete lesion. Evaluation of DAP is not necessarily required in individuals who have light touch or pin-prick sensation at S4-5, as they already have a designation for a sensory incomplete injury.[3] |
Special Topic: Digital Rectal Exam (DRE) in the Research
There is growing evidence that the use of the DRE in the assessment of traumatic spinal cord injury lacks validity and reliability. A 2022 systematic review found that the sensitivity ranged from 0-50% for DRE in detecting both SCI and urethral injuries in adult trauma populations. They found the use of DRE in trauma patients has limited or no validity and reliability in assessing for spinal cord and urethral injuries, and ultimately did not influence the management of these injuries.[4]
Another study by Beeton found that DRE had poor sensitivity and specificity for SCI and did not recommend it as a screening tool with this patient population.[5]
As of now, the 2019 version of the ASIA exam continues to utilise the DRE as part of SCI assessment and classification.
Sensory Level[edit | edit source]
It is defined as the most caudal, intact dermatome for both light touch and pin-prick (sharp/dull discrimination) sensation. The sensory level is determined by performing an examination of the key sensory points within each of the 28 dermatomes on each side of the body, as above, and may be different for the right and left side. The sensory level is the intact dermatome level located immediately above the first dermatome level with impaired or absent light touch or pin-prick sensation, and should be determined for each side of the body as the right and left sides may differ.
Up to four sensory levels may be generated for each dermatome: Right Pin-prick, Right Light Touch, Left Pin-prick and Left Light Touch. The overall single sensory level is the most rostral intact sensory point.[3]
Sensory Score[edit | edit source]
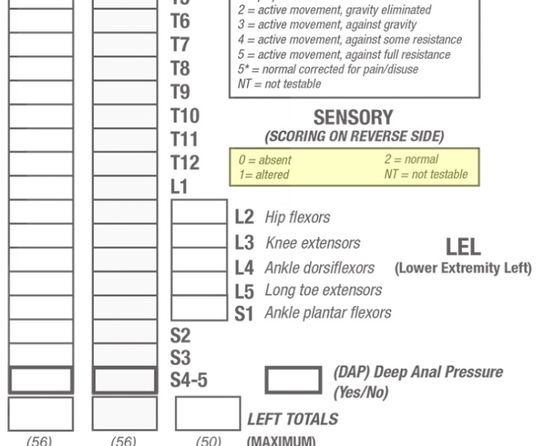
Sensory scores of each dermatome for pin-prick and light touch can be summed across dermatomes and sides of body, right and left, to generate two summary sensory scores: Pin-prick and Light Touch. Normal sensation for each modality is assigned a score of 2. A score of 2 for each of the 28 key sensory points for Light Touch on each side of the body would result in a maximum score of 56 for Light Touch. A score of 2 for each of the 28 key sensory points for Pin-Prick on each side of the body would result in a maximum score of 56 for Pin-Prick. The Total Maximum Sensory Score is 112. The Sensory Score provides a means of numerically documenting changes in sensory function, but cannot be calculated if any required key sensory point is Not Testable.[3]
Motor Examination[edit | edit source]
Key Motor Functions of the 10 Paired Myotomes C5 - T1 and L2 - S1 are tested bilaterally. Improper positioning and stabilization can lead to substitution by other muscles, and will not accurately reflect the muscle function being graded.[3]
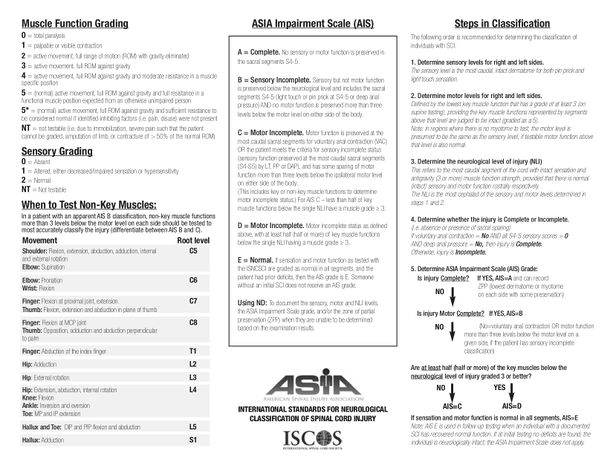
A Six-Point Scale is used for scoring:
| 0 | = | Total Paralysis |
| 1 | = | Palpable or Visible Contraction |
| 2 | = | Active Movement, Full Range of Motion with Gravity Eliminated |
| 3 | = | Active Movement, Full Range of Motion Against Gravity |
| 4 | = | Active Movement, Full Range of Movement against Gravity and Moderate Resistance in a Muscle Specific Position |
| 5 | = | Normal Active Movement, Full Range of Motion Against Gravity and Full Resistance in a Muscle Specific Position expected from an Unimpaired Person |
| 5* | = | Normal Active Movement, Full Range of Motion Against Gravity and Sufficient Resistance to be considered normal if identified Inhibiting Factors i.e., pain, disuse were not present |
| NT | = | Not Testable i.e., due to Immobilization, Severe pain such that the patient cannot be graded, Amputation of Limb, or Contracture of >50% of the Range of Motion |
Patient should be supine-lying for testing, except for the rectal examination that can be performed side-lying. This ensures consistency across tests to allow for a valid comparison from acute stage through to rehabilitation. Each key muscle function should be examined in a cephalo-caudal sequence. Ensure to stabilize both above and below the joint to prevent any muscle substitution during the testing. Move the joints through their full range of movement prior to completing manual muscle testing (MMT), as above, to rule out any pain, spasticity, or contracture which might impact the scores. The hip should not be allowed to actively or passively flex beyond 90° due to the increased kyphotic stress placed on the lumbar spine in any individual with a suspected acute traumatic injury below the T8 level. Instead unilateral, isometric exam should be completed to ensure the contralateral hip remains extended to stabilize the pelvis.[3]
| Level | Key Muscle Function & Muscles | Description of Muscle Function Testing Position for Grade 4 or 5 |
|---|---|---|
| C5 | Elbow Flexion
|
Elbow Flexed at 90, Forearm Supinated |
| C6 | Wrist Extension
|
Full Wrist Extension |
| C7 | Elbow Extension
|
Shoulder Neutral Rotation, Adducted at 90 Flexion with Elbow at 45 Flexion |
| C8 | Flexion of Middle Finger
|
Full Flexed Distal Phalanx with Proximal Finger Joint Stabilised in Extension |
| T1 | Abduction of Little Finger
|
Full Abduction Fingers |
| L2 | Hip Flexion
|
Hip Flexed at 90 |
| L3 | Knee Extension
|
Knee Flexed at 15 |
| L4 | Ankle Dorsiflexion
|
Full Dorsiflexion |
| L5 | Long Toe Extensors
|
Full Extension 1st Toe |
| S1 | Ankle Plantarflexion
|
Hip Neutral with Full Knee Extension and Full Ankle Plantarflexion |
| Voluntary Anal Contraction |
|---|
| The External Anal Sphincter, innervated by the somatic motor components of the Pudendal Nerve S2-4) should be tested on the basis of reproducible voluntary contractions around the examiner's gloved and lubricated index finger, by instructing the patient to “squeeze the finger as if to hold back a bowel movement". A contraction is graded as Absent or Present. A voluntary anal contraction during this part of the exam signifies that the patient has a Motor Incomplete injury. Examiners should be careful to distinguish between voluntary anal contraction from reflex anal contraction, which tends to be produced only with the Valsalva Maneuver.[3] |
Motor Level[edit | edit source]
The Motor Level is defined by the lowest key muscle function that has a grade of at least 3 (on supine testing), providing the key muscle functions represented by segments above that level are judged to be intact (graded as a 5). The motor level is determined, as above, by examining the key muscle function within each of the 10 myotomes on each side of the body, and may be different for the right and left side. In regions where there is no myotome that are clinically testable i.e., C1 to C4, T2 to L1, and S2 to S5, the Motor Level is presumed to be the same as the Sensory Level, if testable motor function above that level is also normal.[3]
Example 1:
If the sensory level is C4, and there is no C5 motor function strength (or strength graded <3), the motor level is C4.
Example 2:
If the sensory level is C4, with C5 key muscle function strength graded as 4, the motor level would be C5 because the strength at C5 is at least 3 with the “muscle function” above considered normal: presumably if there was a C4 key muscle function it would be graded as normal since the sensation at C4 is intact.
Motor Score[edit | edit source]
Motor scores for each myotome can be summed across myotomes and sides of body, right and left, to generate a single motor score for each of the upper limbs and lower limbs. Normal strength is assigned a grade of 5 for each muscle function. A score of 5 for each of the five key muscle functions of the upper extremity would result in a maximum score of 25 for each extremity, totaling 50 for the upper limbs. A score of 5 for each of the five key muscle functions of the lower extremity would result in a maximum score of 25 for each extremity, totaling 50 for the lower limbs. In previous versions of a total motor score of 100 for all extremities was calculated but construct validity of the Motor Score as a measure of recovery following spinal cord injury and as an outcome measure for clinical trials is greater when Upper Extremity and Lower Extremity Motor Scores are scored independently and not summated together, therefore it is now recommended to consider Upper Extremity and Lower Extremity Scores separately. The Motor Score, provide a means of numerically documenting changes in motor function, but cannot be calculated if any required muscle function is Not Testable.[3]
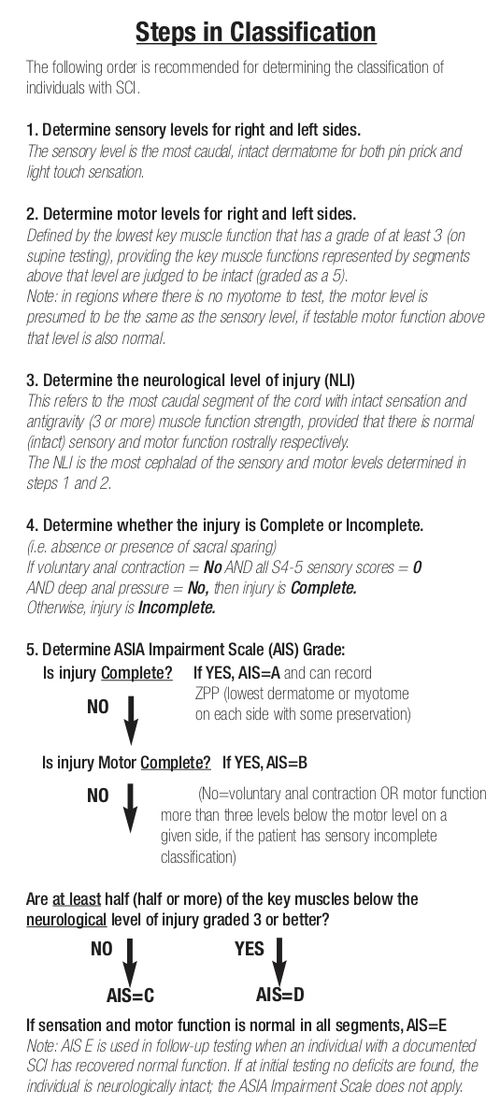
Determination of Neurological Level of Injury[edit | edit source]
The Neurological Level of Injury is determined by identifying the most caudal segment of the cord with intact sensation and antigravity muscle function strength (Grade 3 or more) on both sides of the body, provided that there is normal, intact sensory and motor function rostrally (Grade 5).
Sensory Level refers to the most caudal, intact dermatome for both light touch and pin-prick sensation (Score = 2).
Motor Level refers to the most caudal myotome with a key muscle function of at least Grade 3 on Motor Examination.
If there is a discrepancy between the most caudal intact section between the four possible levels of Right-Sensory Level, Left-Sensory Level, Right-Motor Level, or Left-Motor Level, the Neurological Level of Injury is considered the most cephalad segment of these four levels.[3]
ASIA Impairment Scale (AIS)[edit | edit source]
Spinal Cord Injuries are classified in general terms of being neurologically “Complete” or “Incomplete” based upon Sacral Sparing, which refers to the presence of Sensory or Motor Function in the most Caudal Sacral Segments i.e. preservation of light touch or pin prick sensation at S4-5 Dermatome, Deep Anal Pressure or Voluntary Anal Sphincter Contraction.[3]
Complete Injury: Absence of Sacral Sparing i.e. No Sensory and Motor Function at S4-5
Incomplete Injury: Presence of Sacral Sparing i.e. Partial preservation of Sensory and/or Motor Function at S4-5
Sensory Incomplete: Sacral Sparing of Sensory Function
Motor Incomplete: Sacral Sparing of Motor Function or Sacral Sparing of Sensory and Motor Function more than 3 Levels below Injury
The following ASIA Impairment Scale (AIS) designation is used in grading the degree of impairment:
| Grade | Type of Injury | Description of Injury |
|---|---|---|
| A | Complete | No Sensory or Motor Function is preserved in the Sacral Segments S4-S5 |
| B | Sensory Incomplete | Sensory but not Motor Function is preserved below the neurological level and includes the Sacral Segments S4-S5,
AND No Motor Function is preserved more than three levels below the Motor Level on either side of the body |
| C | Motor Incomplete | Motor Function is preserved below the Neurological Level
AND More than half of key muscle functions below the Neurological Level of Injury have a muscle grade less than 3 (Grades 0-2) |
| D | Motor Incomplete | Motor function is preserved below the neurological level
AND At least half (half or more) of key muscle functions below the NLI have a muscle grade ≥ 3 |
| E | Normal | If sensation and motor function as tested with the ISNCSCI are graded as normal in all segments
AND the patient had prior deficits Then the AIS Grade is E. |
| *Someone without a Spinal Cord Injury does not receive an AIS Grade. | ||
Incomplete injuries are further categorized under 5 types as per their clinical presentation. They are:
- Brown-Sequard Syndrome
- Anterior Cord Syndrome
- Posterior Cord Syndrome
- Conus Medullaris Syndrome
- Cauda Equina Syndrome
Zone of Partial Preservation[edit | edit source]
Earlier, the Zone of Partial Preservation (ZPP) was only used with Complete Injuries ASIA Impairment Scale - Grade A (AIS A).[3] With the 2019 revision, the ZPP now applies to all cases regardless of the grades of AIS.[2] ZPP refers to the dermatomes and myotomes caudal to the sensory or motor level that remain partially innervated. The extent of the Sensory or Motor ZPP is determined by the most caudal segment with some sensory or motor function respectively, and should be recorded for both right and left sides and for sensory and motor function.[3]
Example: If the left sensory level is C6, and some sensation extends from C7 through T1, then “T1” is recorded in the right sensory ZPP block on the worksheet.
Motor ZPP is recorded in Incomplete injuries with absent VAC. Sensory ZPP is recorded in the absence of sensory function in S4-5 (LT and PP), as long as DAP is not present. In the presence of DAP, Sensory ZPP should be noted as “not applicable (NA)”. In the absence of DAP, Sensory ZPP can be recorded if there is absence of LT and PP sensation at S4-5, while it should be noted as “not applicable (NA)” if there is presence of LT or PP sensation at S4-5.[2]
Steps in Classification[edit | edit source]
Psychometrics[edit | edit source]
Reliability[edit | edit source]
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) Sensory and Motor examinations are reliable when conducted by a trained examiner.[8] Both interrater and intrarater reliability were found to be excellent.[9][10] Formal training in the administration of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) Standards has been shown to improve the accuracy of the examiner’s classification.[11] Use of the 2013 Worksheet Revision provides significantly better classification performance and a reduction in misclassification of Motor Level and Neurological Level of Injury since its introduction, except at C2 - 4 Level, which has been suggested may be linked to the body-side based grouping of myotomes and dermatomes on the same horizontal alignment. As such it is recommended that any future revision of the worksheet should maintain the same graphical aspect in the layout.[12]
Validity[edit | edit source]
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) are validated for injury classification.[13] Construct validity of the ASIA Motor Score as a measure of recovery following spinal cord injury and as an outcome measure for clinical trials is greater when Upper Extremity and Lower Extremity Motor Scores are scored independently and not summated together.[13]
Importance of Patient Explanation[edit | edit source]
The ASIA Exam should be completed within 72 hours of the spinal cord injury to reliably predict recovery. The examination is extremely uncomfortable and confusing for individuals, particularly because they have recently gone through significant trauma. Explaining why we do the test and what is it entails is vital to make individuals more comfortable during the exam.[11]
The clinician must inform subjects that this test will help us determine the location of injury to the spinal cord, its severity, and gauge prognosis through time.[3] Often, the International Standards for Neurological Classification of Spinal Cord Injury and ASIA Impairment Scale paint a different picture in comparison to what is seen on an MRI or CT scan.
Resources[edit | edit source]
International Standards for Neurological Classification of Spinal Cord Injury: Assessment Forms
- ASIA Impairment Scale: International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) Assessment Form
- ASIA Impairment Scale: Autonomic Standards Assessment Form
International Standards for Neurological Classification of Spinal Cord Injury: Sensory and Motor Guides
ASIA E-Learning Centre InSTeP: International Standards
- To promote the teaching and competent use of the Standards, ASIA with contribution from the International Spinal Cord Society has developed the International Standards Training e-Learning Program or InSTeP.
ASIA E-Learning Centre ASTeP: Autonomic Anatomy & Function
- The goal of this training for the Autonomic Standards is to learn normal autonomic functions, understand the changes in autonomic functions following spinal cord injury (SCI) and use the Autonomic Assessment to document and classify remaining autonomic neurological function.
References[edit | edit source]
- ↑ Golestani A, Shobeiri P, Sadeghi-Naini M, Jazayeri SB, Maroufi SF, Ghodsi Z, Dabbagh Ohadi MA, Mohammadi E, Rahimi-Movaghar V, Ghodsi SM. Epidemiology of traumatic spinal cord injury in developing countries from 2009 to 2020: A systematic review and meta-analysis. Neuroepidemiology. 2022 May 5;56(4):219-39.
- ↑ 2.0 2.1 2.2 ASIA and ISCoS International Standards Committee. The 2019 revision of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)-What's new? Spinal Cord. 2019 Oct;57(10):815-817.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 Burns S, Biering-Sørensen F, Donovan W, Graves D, Jha A, Johansen M, Jones L, Krassioukov A, Kirshblum, Mulcahey MJ, Schmidt Read M, Waring W. International Standards for Neurological Classification of Spinal Cord Injury, Revised 2011. Top Spinal Cord Inj Rehabil 2012;18(1):85-99.
- ↑ Docimo S, Diggs L, Crankshaw L, Lee Y, Vinces F. No evidence supporting the routine use of digital rectal examinations in trauma patients. Indian Journal of Surgery. 2015 Aug;77:265-9.
- ↑ Beeton G, Alter N, Zagales R, Wajeeh H, Elkbuli A. The benefits and clinical application of the digital rectal exam in trauma populations: Towards enhancing patient safety and quality outcomes. The American Journal of Emergency Medicine. 2022 Nov 8.
- ↑ UCTeach Ortho. ASIA Impairment Scale. Available from: https://youtu.be/hO9hADODTw8[last accessed 30/10/18]
- ↑ SCIREWebVideo . Common Errors Made During the ISNCSCI Examination (ASIA Exam). Available from: https://www.youtube.com/watch?v=PpgGzIhCpuI[last accessed 30/10/18]
- ↑ Marino R, Jones L, Kirshblum S, Tal J, Dasgupta A. Reliability and repeatability of the motor and sensory examination of the international standards for neurological classification of spinal cord injury. J Spinal Cord Med 2008;31(2)166-170.
- ↑ Clifton G, Donovan W, Dimitrijevic M et al. Omental transposition in chronic spinal cord injury. Spinal Cord 1996; 34:193–203.
- ↑ Savic G, Bergström EM, Frankel HL, Jamous MA, Jones PW. Inter-rater reliability of motor and sensory examinations performed according to American Spinal Injury Association standards. Spinal Cord. 2007;45(6):444-51.
- ↑ 11.0 11.1 Schuld C, Wiese J, Franz S, Putz C, Stierle I, Smoor I, Weidner N, EMSCI Study Group, Rupp RR. Effect of formal training in scaling, scoring and classification of the international standards for neurological classification of spinal cord injury. Spinal Cord 2013;51(4):282-8.
- ↑ Schuld C, Franz S, Brüggemann K, Heutehaus L, Weidner N, Kirshblum SC, Rupp R. International Standards for Neurological Classification of Spinal Cord Injury: Impact of the Revised Worksheet (Revision 02/13) on Classification Performance. The Journal of Spinal Cord Medicine. 2016 Sep 2;39(5):504-12.
- ↑ 13.0 13.1 Graves D, Frankiewicz RG, Donovan WH. Construct validity and dimensional structure of the ASIA motor scale. J Spinal Cord Med 2006;29(1):39-45.