Adult Spastic Cerebral Palsy: A Case Study Amidst A Lack of Evidence: Difference between revisions
Leena Barisa (talk | contribs) No edit summary |
No edit summary |
||
| Line 229: | Line 229: | ||
To reach his functional goals we targeted three main areas with interventions: | To reach his functional goals we targeted three main areas with interventions: | ||
# Gait training | |||
## With the goal of being able to ambulate with the use of a gait aid independently for 150 | |||
# Upper extremity fine motor training | |||
## To address the client’s desire to be able to participate in video games and use technology such as a cell phone with a touch screen | |||
# Aerobic conditioning | |||
## To allow the client to participate in daily activities such as getting around the house, spending time with friends etc. without feeling tired | |||
==== Techniques used: ==== | ==== Techniques used: ==== | ||
===== Gait Training: ===== | ===== 1. Gait Training: ===== | ||
- | '''0-8 Weeks Treadmill''' '''Training''' | ||
o A study by Hesse et al.,<ref name=":5">Hesse S., Bertelt C., Jahnke M. T., Schaffrin A., Baake P., Malezic M., et al. Treadmill Training With Partial Body Weight Support Compared With Physiotherapy in Nonambulatory Hemiparetic Patients. Stroke. 1995 Jun 1;26(6):976–81.</ref> shows that among individuals who are non ambulatory and have hemiparesis, weighted body treadmill training and can be effective in restoring normal walking abilities in a shorter amount of time compared to land training. This therapy has also been used in children with spastic cerebral palsy with good outcomes<ref>Schindl MR, Forstner C, Kern H, Hesse S. Treadmill Training With Partial Body Weight Support in Nonambulatory Patients With Cerebral Palsy. 2000;81:6.</ref>. We decided to begin our patient’s gait training with weighted treadmill training as follows: | o A study by Hesse et al.,<ref name=":5">Hesse S., Bertelt C., Jahnke M. T., Schaffrin A., Baake P., Malezic M., et al. Treadmill Training With Partial Body Weight Support Compared With Physiotherapy in Nonambulatory Hemiparetic Patients. Stroke. 1995 Jun 1;26(6):976–81.</ref> shows that among individuals who are non ambulatory and have hemiparesis, weighted body treadmill training and can be effective in restoring normal walking abilities in a shorter amount of time compared to land training. This therapy has also been used in children with spastic cerebral palsy with good outcomes<ref>Schindl MR, Forstner C, Kern H, Hesse S. Treadmill Training With Partial Body Weight Support in Nonambulatory Patients With Cerebral Palsy. 2000;81:6.</ref>. We decided to begin our patient’s gait training with weighted treadmill training as follows: | ||
* Started patient in a sling supported over a treadmill while unweighting the client to 30% of their body weight and was gradually progressed to full weight bearing as soon as possible. The patient was not to be sitting in the sling at any point throughout the therapy<ref name=":5" />. | ** Started patient in a sling supported over a treadmill while unweighting the client to 30% of their body weight and was gradually progressed to full weight bearing as soon as possible. The patient was not to be sitting in the sling at any point throughout the therapy<ref name=":5" />. | ||
* The treadmill was set to a comfortable walking speed. One therapist and a PTA controlled the movement of the pelvis and lower limbs through space in a controlled manner in order to instruct the patient on the feeling of a proper gait cycle for 10 minutes which served as the warm up. | ** The treadmill was set to a comfortable walking speed. One therapist and a PTA controlled the movement of the pelvis and lower limbs through space in a controlled manner in order to instruct the patient on the feeling of a proper gait cycle for 10 minutes which served as the warm up. | ||
* The patient then walked without the use of the therapist for another 10-20 minutes at a slightly increased speed, followed by a cool down. | ** The patient then walked without the use of the therapist for another 10-20 minutes at a slightly increased speed, followed by a cool down. | ||
* The goal with this therapy was to gradually increase the amount of weight the patient could bear, progressing to full weight bearing status and use of the handrails during walking with the hope that this would increase the patient’s ability to ambulate correctly and regain walking ability<ref name=":5" />. | ** The goal with this therapy was to gradually increase the amount of weight the patient could bear, progressing to full weight bearing status and use of the handrails during walking with the hope that this would increase the patient’s ability to ambulate correctly and regain walking ability<ref name=":5" />. | ||
'''9-12 Weeks Parallel bars training''' | |||
o Gait training was performed initially for 5 minutes per day and progressed by 5 minutes per week from weeks 9-16 | o Gait training was performed initially for 5 minutes per day and progressed by 5 minutes per week from weeks 9-16 | ||
| Line 260: | Line 254: | ||
o Once client progressed to 4-5 continuous steps within the parallel bars, we incorporated alternate tasks such as turning head to look while ambulating, releasing once hand from the rail, walking over obstacles and counting backwards by threes from 97 | o Once client progressed to 4-5 continuous steps within the parallel bars, we incorporated alternate tasks such as turning head to look while ambulating, releasing once hand from the rail, walking over obstacles and counting backwards by threes from 97 | ||
'''17-24 Weeks Rhythmic auditory stimulation''' | |||
* This was implemented once the patient progressed to the level of working on gait speed and cadence. Research shows this to be a beneficial method for increasing cadence, velocity and step length in patients with spastic CP<ref name=":6">Kim SJ, Kwak EE, Park ES, Cho S-R. Differential effects of rhythmic auditory stimulation and neurodevelopmental treatment/Bobath on gait patterns in adults with cerebral palsy: a randomized controlled trial. Clinical Rehabilitation. 2012 Oct;26(10):904–14.</ref>. | |||
* This involved 30-minute gait sessions performed 3 times per week from weeks 17-24 | |||
* The client was initially asked to walk at their own pace in their bare feet for 30 meters while the therapist counted their steps/minute to get the cadence. The tempo of a metronome beat was then set to the client’s cadence as their foot hit the ground. A simple rhythmic music pattern was then selected and synchronized to the metronome beats for the client to ambulate to<ref name=":6" />. | |||
===== 2. Upper Extremity Fine Motor Training: ===== | ===== 2. Upper Extremity Fine Motor Training: ===== | ||
'''0-4 Weeks Mirror therapy and Motor Imagery''' '''Training''' | |||
* Initially used while the patient was working on strengthening exercises specific to the wrist and hand. Therapy lasted 4 weeks and was performed for 1 hour 3 times a week. | |||
* Motor imagery theory is predicted to be a prerequisite for motor planning<ref name=":8">Steenbergen B, Crajé C, Nilsen DM, Gordon AM. Motor imagery training in hemiplegic cerebral palsy: a potentially useful therapeutic tool for rehabilitation. Developmental Medicine & Child Neurology. 2009;51(9):690–6.</ref>. Before we began with motor execution training of the upper extremity, we implemented motor planning/imagery techniques with the client in order train the cognitive aspects of action behaviour in the hope that this would positively benefit the client’s ability to execute the movements. | |||
* This form of therapy has been studied in adult stroke populations and is hypothesized by Steenbergen et al. to potentially be an effective form of rehabilitation in the CP population<ref name=":8" />. | |||
* This therapy involved the use of a mirror box whereby the patient placed their unaffected limb opposite the box and performed wrist extension and flexion finger abduction and adduction and ulnar and radial deviation. The patient was instructed to imagine that they were performing the movements bilaterally, with the correct timing and sequencing of the movement. | |||
* The therapy also involved the therapist instructing the patient to imagine themselves performing functional tasks such as tying their shoes, using a cell phone and loading a dishwasher as previous studies using this therapy suggest<ref name=":8" /> and this was in line with the patient’s goals. | |||
'''4-16 Weeks Computer Gaming Exercises''' | |||
o Because of the patient’s expression for the need to be able to interact with computers and use digital technology, we attempted to make the fine motor upper extremity training for him meaningful by incorporating the use of computer games. To do this we used miniBird sensor technology consistent with the case study done by Szturm et al.<ref>Szturm T, Peters JF, Otto C, Kapadia N, Desai A. Task-specific rehabilitation of finger-hand function using interactive computer gaming. Archives of Physical Medicine & Rehabilitation. 2008 Nov;89(11):2213–7.</ref>. | o Because of the patient’s expression for the need to be able to interact with computers and use digital technology, we attempted to make the fine motor upper extremity training for him meaningful by incorporating the use of computer games. To do this we used miniBird sensor technology consistent with the case study done by Szturm et al.<ref>Szturm T, Peters JF, Otto C, Kapadia N, Desai A. Task-specific rehabilitation of finger-hand function using interactive computer gaming. Archives of Physical Medicine & Rehabilitation. 2008 Nov;89(11):2213–7.</ref>. | ||
| Line 283: | Line 272: | ||
o The fine motor intervention began with hand manipulation exercises incorporating various objects of differing sizes, weights and textures. The object selected was attached to the sensor and then the patient chose a computer game to apply the motions to. These games had a range of activity levels and included tracing mazes, drawing exercises, and functional tasks such as placing objects in cupboards, card flipping and stereognosis similar to the techniques described in Brown et al.<ref>Brown SH, Lewis CA, McCarthy JM, Doyle ST, Hurvitz EA. The Effects of Internet-Based Home Training on Upper Limb Function in Adults With Cerebral Palsy. Neurorehabilitation and Neural Repair. 2010 Jul;24(6):575–83.</ref>. The patient began with games at slower speeds, requiring less precision and visual-spatial planning and progressed by increasing these parameters. | o The fine motor intervention began with hand manipulation exercises incorporating various objects of differing sizes, weights and textures. The object selected was attached to the sensor and then the patient chose a computer game to apply the motions to. These games had a range of activity levels and included tracing mazes, drawing exercises, and functional tasks such as placing objects in cupboards, card flipping and stereognosis similar to the techniques described in Brown et al.<ref>Brown SH, Lewis CA, McCarthy JM, Doyle ST, Hurvitz EA. The Effects of Internet-Based Home Training on Upper Limb Function in Adults With Cerebral Palsy. Neurorehabilitation and Neural Repair. 2010 Jul;24(6):575–83.</ref>. The patient began with games at slower speeds, requiring less precision and visual-spatial planning and progressed by increasing these parameters. | ||
o The intervention was performed 3 times a week for 45 hour at a time from 4-16 weeks from the commencement of therapy | o The intervention was performed 3 times a week for 45 hour at a time from 4-16 weeks from the commencement of therapy. | ||
'''16-24 Weeks Internet-Based Exercises''' | |||
* Following that the patient was instructed and set up with the equipment to perform similar tasks at home using a computer guided game system designed by the therapist. The therapist was available by a webcam to ensure the patient was performing the tasks correctly. | |||
http://home.cc.umanitoba.ca/~petersii/wren/computer-assisted-rehabilitation-exercise-system-for-finger-hand-and-arm-functions.html | http://home.cc.umanitoba.ca/~petersii/wren/computer-assisted-rehabilitation-exercise-system-for-finger-hand-and-arm-functions.html | ||
===== 3. Aerobic Conditioning: ===== | ===== 3. Aerobic Conditioning: ===== | ||
* We incorporated aerobic conditioning with the patient to help him increase his ability to participate in activities with friends and family. This involved: | |||
* Aerobic exercises and sports activities to improve general cardiovascular fitness<ref name=":7" /> to allow him to complete more functional activities without need for resting was combined with patient education on the importance of exercising as well as discussion regarding barriers to implementing physical activity in the patient’s life<ref name=":7" /> | |||
* We incorporated a '''graded exercise program''' of aerobic conditioning. We started the patient off with recumbent biking for 15 minutes at a mild-moderate intensity (3METs). The volume of activity was increased by 20% each week for a total of 4 weeks, followed by a regression of the time back to 15 minutes and an increase in the intensity. This was continued for a total of 24 weeks | |||
== Outcome == | == Outcome == | ||
Revision as of 19:48, 9 May 2019
Abstract[edit | edit source]
This fictional case is presented in order to share the impact that a physiotherapy intervention can have on the body structure, activity, and participation of an adult with spastic cerebral palsy. Additionally, this case adds to the limited evidence and case studies done to examine adults with cerebral palsy, a population that is severely underreported on. This fictional 24 year old patient with acquired right side hemiplegic spastic cerebral palsy was referred to physiotherapy due to a recent decline in his walking abilities and functional ability. He presented with physical impairments and was classified as a level 3 on the GMFCS. The interventions used were based on the ICF model to address the body structure, activity and participation components.This case demonstrates the importance of physiotherapy in chronic conditions such as cerebral palsy, and the changes that exercise based interventions can have for a adult who is deteriorating due to this condition.
Introduction[edit | edit source]
Cerebral palsy (CP) is a non-progressive permanent condition that is associated with a variety of movement, mobility and postural challenges as well as occasionally neurological changes. Despite CP being a lifelong condition the majority of research is based on children with little to no attention to those with CP whom are 18 years of age or older [1] despite a trend toward increased life expectancy[2]. As individuals with CP age they are at risk for secondary impairments, including stiffness, pain, fatigue and decreased mobility. These challenges can lead to loss of mobility and participation in early adulthood and continues into one’s later years. According to Bottos et al. (2001), between 30% and 52% of adults with CP will experience deterioration in their ability to ambulate[3]. This loss is most often seen in adults 20 and 40 years of age[3] . Loss of mobility will often lead to a decrease in participation in activities of daily living (ADLs) as well as overall quality of life. There has been two systematic reviews regarding the effects of physical activity, fitness and participation of adults with CP [4] however there is little research regarding the effects of physiotherapy interventions and mobility/participation in adults with CP. There is much research regarding children and their physical therapy experience but the adult population remains understudied. This fictional case study follows a 24 year old male with acquired CP whom experienced a deterioration of his gait and ability to participate in ADLs when he entered young adulthood. He was ranked a level 3 on the Gross Motor Classification Scale. The physiotherapy program implemented in this case study hopes to share with physiotherapists the impact that physical therapy can have on the mobility, participation in ADLs and overall quality of life for young adults with CP in lieu of the lack of research in this area.
Subjective Assessment[edit | edit source]
During the subjective assessment, the patient’s parents were present to assist the patient in answering questions. The patient was referred to physiotherapy from his family doctor because of his difficulty in managing the physical symptoms of his cerebral palsy and recent functional decline as a result of a decline in walking ability. The patient was previously using forearm crutches for ambulation but has recently transitioned to using a posterior posture four wheeled walker due to his recent decline in walking ability. The patient has been experiencing symptoms of right sided hemiplegic spastic cerebral palsy since the age of one due to a bout of encephalitis, a common cause of postnatally acquired cerebral palsy[5] . The condition has affected mostly his right arm and leg, leading to motor and sensory impairments, pain, and has led to secondary low back pain[6] . Commonly associated with his condition, the patient has occasional seizures that are well managed by medication and a mild-moderate cognitive impairment that limits his ability to learn, comprehend and remember[6] . The patient lives with both parents in a one storey home. The patient graduated from high school at the age of 21 and now attends a day program a few days a week and works part time as an office assistant. Having this job is very important to the patient and a very important factor for adults with cerebral palsy[7] . The patient is able to complete the majority of his ADLs, such as dressing, feeding, bathing and walking with assistive devices; however, he and his parents are noticing increasingly that he is limited by pain, physical limitations and fatigue. In his instrumental activities of daily living (IADLs), the patient requires assistance, which is common for many individuals with cerebral palsy [8]. The patient does not currently participate in any structured physical activity and walks only when needed due to increased fatigue and associated difficulty with movement. The patient appears to have very low motivation to be involved in the community and with physical activity. The patient and his parents would like to reverse his decline in walking function, returning to using his forearm crutches and hopefully improve to be able to perform ADLs more independently.
Medications: Baclofen and Diazepam
Objective Assessment[edit | edit source]
The patient appeared to be underweight, have mild dysarthria and difficulty managing saliva [8]. Objectively, the patient presents with right arm resting posture of shoulder adduction, elbow, wrist and finger flexion, and forearm pronation [8]. Resting right leg posture showed slight hip and knee flexion, and significant plantarflexion of the ankle[8]. The patient had increased tone and spasticity in the right upper limb and lower limb throughout the available range of motion as well as decreased passive range of motion with hip and knee extension, hip abduction, elbow and wrist extension, shoulder abduction and forearm supination [8]. There was also a notable contracture of the gastroc-soleus complex [8]. The patient had reduced strength in both the right upper and lower extremities[8]. Left side strength and range of motion was within normal limits. The patient had impaired sensation in the right upper and lower extremities, with decreased 2 point discrimination, proprioception, and astereognosis. Deep tendon reflexes were brisk with clonus and the Babinski sign was present. The presentation of decreased sensation and hyperreflexia are common in people with spastic cerebral palsy [6]. During gait, the patient used his posterior posture four wheeled walker. The patient demonstrated circumduction and adduction of the right hip during the swing phase. Initial contact was made on metatarsal heads, demonstrating foot equinus. The patient had a flexed and stiff right knee and hip throughout the gait cycle, and anterior pelvic tilt. The patient's gait was slow and he demonstrated shortened stride length, decreased stance time on the right side and minimal trunk movement. The patient’s gait pattern was similar to those previously described in cerebral palsy [9]. Please see the Physiopediapage on the classification of gait patterns in CP for more information on common gait patterns and how to classify them. [Classification of Gait Patterns in Cerebral Palsy: https://www.physio-pedia.com/Classification_of_Gait_Patterns_in_Cerebral_Palsy]. There is a severe lack of information regarding tools validated to use to assess gait in this population, which is why we chose to assess the patient via observation.
Outcome Measures at Baseline
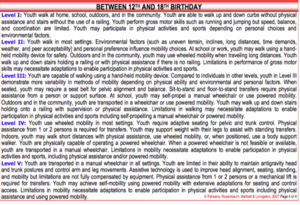
Gross Motor Function Classification System (GMFCS):
The GMFCS is a classification tool used in children with cerebral palsy up to age 18[10]. The classification for this patient was based off of the description in figure 1 and 2 of level 3 for children between 12 and 18, as there is currently no classification system for adults with cerebral palsy[10]. The patient is classified as a level 3 within this system.
For more information on this scale please refer to
To see a video demonstrating this system please refer to
SF-36 Health Survey:
The SF-36 health survey is used to measure a patient's health quality of life. This assessment can be separated into 8 separate domains. Results for this patient according to the 8 domains are presented here, and are common in patients with this presentation [11]. See appendix a. for full survey.
- Vitality (energy/Fatigue):score = 60
- Role limitations due to emotional problems: score = 100
- Social functioning: score = 75
- Emotional well-being: score = 80
- Bodily Pain: score = 65
- Physical functioning: score = 50
- Role limitations due to physical problems: score = 100
- General Health: score= 50
For more information about this survey please refer to
https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/scoring.html
BMI:
The patient has a height of 5’5 inches and a weight of 110 lbs, making his BMI 18.3. This BMI indicates that the patient is underweight [12], which is a common presentation in adults with cerebral palsy, as they often have trouble eating[8] .
FIM:
See appendix a. For full chart.
- Self care: score = 37
- Sphincter control: score = 14
- Transfers: score = 18
- Locomotion: score = 12
- Social Cognition: score = 10
- Communication: score = 12
Total FIM score = 103
Results for this outcome measure were predicted using Gannotti et al.’s[13] and Sandström et al.’s [14] articles.
For more information on the FIM please visit https://physio-pedia.com/Functional_Independence_Measure_(FIM)
6 minute walk test:
There is little consensus in the literature as to which balance tests are valid in the population of adults with cerebral palsy. However this test is has been shown to be reliable in adults with cerebral palsy[15] and it is used by researchers to record the effectiveness of their intervention with a population of people with cerebral palsy (average age of 15.5 years old)[16].
Meters walked in 6 minutes: 239 m
For more information in the 6 minute walk test please see
https://www.physio-pedia.com/Six_Minute_Walk_Test_/_6_Minute_Walk_Test
BEST:
There is little consensus in the literature as to which balance tests are valid in the population of adults with cerebral palsy. However this test is used by researchers when examining an adult population with spastic cerebral palsy [17]and so we will use it here.
The following indicates the 6 subsystems measured using the BEST test. The score is presented as a percentage of the total possible score in each section.
- biomechanical constraints: score =57
- stability limits/verticality: score =76
- anticipatory postural adjustments: score =39
- postural responses: score=28
- sensory orientation: score=64
- stability in gait:score=67
Results for this outcome measure were predicted using Opheim et al.’s [17]article.
For more information in the BESTest please see https://physio-pedia.com/Balance_Evaluation_Systems_Test_(BESTest)
Clinical Impression[edit | edit source]
Physiotherapy Diagnosis:
Functional motor impairments affecting right side and resulting in decreased ability to ambulate and engage in activities of daily living.
Problem list:
- Weakness from impaired voluntary motor control due to lack of coordinated agonist and antagonist muscle contraction
- Constant plantar flexion causing difficulties with gait due to high tone and contracture in plantar flexors
- High spasticity in right arm leading to decreased ROM and inability to participate in ADLs
- Decreased ability to ambulate independently and thus decreased ability to engage in activities of daily living due to impaired voluntary movements, balance, and spasticity[18].
Intervention[edit | edit source]
Patient-centred treatment goals[edit | edit source]
Short term (0-8 weeks)[edit | edit source]
- Ability to have less mobile joints with high spaciticy passively moved with enough range to allow for skin hygiene by the end of 4 weeks
- Ability to remain upright after small internal perturbations with moderate support by the end of 4 weeks
- Able to stand independently and walk with the use of a gait aid by the end of 8 weeks
- Able to manipulate larger, lighter objects such as an empty cup with spastic right side by the end of 8 weeks
Long term goals (9-24 weeks)[edit | edit source]
- Able to remain upright after moderate internal perturbations to increase independence with ambulation after 16 weeks
- Maintain available ROM in joints affected by spasticity in 24 weeks to facilitate ambulation and prevent contractures
- Able to perform and regain ability to perform certain BADLs, such those in the SF-36, in 24 weeks by increasing strength and endurance
- Take 5 steps between parallel bars without use of hands on the bars and without loss of balance, in 16 weeks
- Able to ambulate for 20min without experiencing fatigue and with limited assistance from caregivers to increase ability to do ADLs in 24 weeks time
- Manipulate both smaller and heavier objects such as utensils and/or pots with spastic right side by the end of 24 weeks
- Able to use technological devices such as a video game remote and smart phone to participate in social events by the end of 24 weeks
Intervention approach: body, structure, and function, ICF Domain[edit | edit source]
For more information on the ICF domains please see [https://physio-pedia.com/ICF_and_RPS_within_Cerebral_Palsy]
To reach his body, structure, and function goals that are the basis for more functional goals presented in the next section we targeted three main areas with interventions
- Strengthening
- With the goal increasing gait and ADL abilities
- Range of motion
- With the goal of caring for skin and easing contractures
- Balance
- With the goal increasing gait and ADL abilities
Techniques used:[edit | edit source]
1. Strengthening[edit | edit source]
- Strengthening was incorporated from 0-24 weeks
- Weight and resistance were increased as needed when the exercises no longer challenged the patient.
| Joint | Muscles | Exercises |
| Shoulder
[19] * |
Biceps brachii | Biceps curls with light dumbells secured to hands as needed
10 reps, 3 sets, 3 times a week, to an intensity of light fatigue by the end of the day |
| Triceps brachii | Triceps brachii extensions with light resistance theraband, secured to hands as needed.
10 reps, 3 sets, 3 times a week, to an intensity of light fatigue by the end of the day | |
| Pectoralis major | Seated chest press with light resistance therabands, secured to hands as needed.
10 reps, 3 sets, 3 times a week, to an intensity of light fatigue by the end of the day | |
| Deltoid | Seated arm abduction with light resistance therabands, secured to hands as needed.
10 reps, 3 sets, 3 times a week, to an intensity of light fatigue by the end of the day | |
| Hip | Flexors | Seated hip flexion with progression including resistance band as needed
10reps, 3 sets, 3 times a day, 3 days a week, to an intensity of light fatigue by end of the day |
| Ankle | Dorsiflexors | Seated dorsiflexion strengthening with light resistance theraband
10reps, 3 sets, 3 times a day, 3 days a week, to an intensity of light fatigue by end of the day |
*Article specifies muscle groups and parameters but not specific exercises. Exercises were thus chosen by us editors as appropriate for patient.
2. Stretching[edit | edit source]
- Stretching was incorporated from 0-24 weeks.
- Stretches were done to maintain range.
- Held for 20s done 3 times and repeated 3 times a day to an intensity of a light stretch unless otherwise specified.
| Joint | Muscle Group | Stretch |
| Shoulder | Adductors | Passive shoulder abduction by therapist or caregiver |
| Wrist and hand | Wrist flexors | Passive wrist flexion by therapist or caregiver or his unaffected arm |
| Finger flexors | Passive finger flexion by therapist or caregiver or his unaffected arm | |
| Forearm pronators | Passive forearm pronation by therapist or caregiver or his unaffected arm | |
| Hip | Adductors | Lying supine with knees out to the sides |
| Flexors | Lying prone | |
| Knee | Flexors | Lying prone with very light weight on ankles to extend knees |
| Ankle | Plantar flexors | Treadmill walking on an incline for 30min everyday to decrease joint contractures. Progression included increasing the incline weekly[20]. |
3. Balance[edit | edit source]
- Balance training was incorporated from 0 to 24 weeks
Exercise: Balance via APA training as per the Su and Chow[21] study with parameters determined by implementing therapists in this case study
- Trunk rotation tasks standing supported such as reaching across the body to increase ability to maintain balance while doing tasks.
- 10 reps, 3 sets, 3 times a day, 3 days a week, to an intensity of a mild challenge to support himself
- Balance exercises were progressed by increasing perturbations when the previous ones no longer challenged the patient.
Intervention Approach: Activity and Participation[edit | edit source]
To address all domains under the ICF, we also implemented functional training exercises that helped our client reach his activity goals leading to attainment of independent participation in daily activities.
To reach his functional goals we targeted three main areas with interventions:
- Gait training
- With the goal of being able to ambulate with the use of a gait aid independently for 150
- Upper extremity fine motor training
- To address the client’s desire to be able to participate in video games and use technology such as a cell phone with a touch screen
- Aerobic conditioning
- To allow the client to participate in daily activities such as getting around the house, spending time with friends etc. without feeling tired
Techniques used:[edit | edit source]
1. Gait Training:[edit | edit source]
0-8 Weeks Treadmill Training
o A study by Hesse et al.,[22] shows that among individuals who are non ambulatory and have hemiparesis, weighted body treadmill training and can be effective in restoring normal walking abilities in a shorter amount of time compared to land training. This therapy has also been used in children with spastic cerebral palsy with good outcomes[23]. We decided to begin our patient’s gait training with weighted treadmill training as follows:
- Started patient in a sling supported over a treadmill while unweighting the client to 30% of their body weight and was gradually progressed to full weight bearing as soon as possible. The patient was not to be sitting in the sling at any point throughout the therapy[22].
- The treadmill was set to a comfortable walking speed. One therapist and a PTA controlled the movement of the pelvis and lower limbs through space in a controlled manner in order to instruct the patient on the feeling of a proper gait cycle for 10 minutes which served as the warm up.
- The patient then walked without the use of the therapist for another 10-20 minutes at a slightly increased speed, followed by a cool down.
- The goal with this therapy was to gradually increase the amount of weight the patient could bear, progressing to full weight bearing status and use of the handrails during walking with the hope that this would increase the patient’s ability to ambulate correctly and regain walking ability[22].
9-12 Weeks Parallel bars training
o Gait training was performed initially for 5 minutes per day and progressed by 5 minutes per week from weeks 9-16
o This therapy involved a series of exercises including forward stepping, backward stepping, tandem stepping, as well as taking steps with a narrow BoS. Each was practiced for 4-5 steps each or until the client was at the end of the parallel bars
o Once client progressed to 4-5 continuous steps within the parallel bars, we incorporated alternate tasks such as turning head to look while ambulating, releasing once hand from the rail, walking over obstacles and counting backwards by threes from 97
17-24 Weeks Rhythmic auditory stimulation
- This was implemented once the patient progressed to the level of working on gait speed and cadence. Research shows this to be a beneficial method for increasing cadence, velocity and step length in patients with spastic CP[24].
- This involved 30-minute gait sessions performed 3 times per week from weeks 17-24
- The client was initially asked to walk at their own pace in their bare feet for 30 meters while the therapist counted their steps/minute to get the cadence. The tempo of a metronome beat was then set to the client’s cadence as their foot hit the ground. A simple rhythmic music pattern was then selected and synchronized to the metronome beats for the client to ambulate to[24].
2. Upper Extremity Fine Motor Training:[edit | edit source]
0-4 Weeks Mirror therapy and Motor Imagery Training
- Initially used while the patient was working on strengthening exercises specific to the wrist and hand. Therapy lasted 4 weeks and was performed for 1 hour 3 times a week.
- Motor imagery theory is predicted to be a prerequisite for motor planning[25]. Before we began with motor execution training of the upper extremity, we implemented motor planning/imagery techniques with the client in order train the cognitive aspects of action behaviour in the hope that this would positively benefit the client’s ability to execute the movements.
- This form of therapy has been studied in adult stroke populations and is hypothesized by Steenbergen et al. to potentially be an effective form of rehabilitation in the CP population[25].
- This therapy involved the use of a mirror box whereby the patient placed their unaffected limb opposite the box and performed wrist extension and flexion finger abduction and adduction and ulnar and radial deviation. The patient was instructed to imagine that they were performing the movements bilaterally, with the correct timing and sequencing of the movement.
- The therapy also involved the therapist instructing the patient to imagine themselves performing functional tasks such as tying their shoes, using a cell phone and loading a dishwasher as previous studies using this therapy suggest[25] and this was in line with the patient’s goals.
4-16 Weeks Computer Gaming Exercises
o Because of the patient’s expression for the need to be able to interact with computers and use digital technology, we attempted to make the fine motor upper extremity training for him meaningful by incorporating the use of computer games. To do this we used miniBird sensor technology consistent with the case study done by Szturm et al.[26].
o The fine motor intervention began with hand manipulation exercises incorporating various objects of differing sizes, weights and textures. The object selected was attached to the sensor and then the patient chose a computer game to apply the motions to. These games had a range of activity levels and included tracing mazes, drawing exercises, and functional tasks such as placing objects in cupboards, card flipping and stereognosis similar to the techniques described in Brown et al.[27]. The patient began with games at slower speeds, requiring less precision and visual-spatial planning and progressed by increasing these parameters.
o The intervention was performed 3 times a week for 45 hour at a time from 4-16 weeks from the commencement of therapy.
16-24 Weeks Internet-Based Exercises
- Following that the patient was instructed and set up with the equipment to perform similar tasks at home using a computer guided game system designed by the therapist. The therapist was available by a webcam to ensure the patient was performing the tasks correctly.
3. Aerobic Conditioning:[edit | edit source]
- We incorporated aerobic conditioning with the patient to help him increase his ability to participate in activities with friends and family. This involved:
- Aerobic exercises and sports activities to improve general cardiovascular fitness[4] to allow him to complete more functional activities without need for resting was combined with patient education on the importance of exercising as well as discussion regarding barriers to implementing physical activity in the patient’s life[4]
- We incorporated a graded exercise program of aerobic conditioning. We started the patient off with recumbent biking for 15 minutes at a mild-moderate intensity (3METs). The volume of activity was increased by 20% each week for a total of 4 weeks, followed by a regression of the time back to 15 minutes and an increase in the intensity. This was continued for a total of 24 weeks
Outcome[edit | edit source]
Outcome Measures Post Intervention
Gross Motor Function Classification System (GMFCS):
Level 3
SF-36 Health Survey:
- Vitality (energy/Fatigue):score = 80
- Role limitations due to emotional problems: score = 200
- Social functioning: score = 125
- Emotional well-being: score = 120
- Bodily Pain: score = 90
- Physical functioning: score = 200
- Role limitations due to physical problems: score = 200
- General Health: score= 50
BMI:
5’5 inches and a weight of 120 lbs, making his BMI 20.0.
FIM:
See appendix a. For full chart.
- Self care: score = 40
- Sphincter control: score = 14
- Transfers: score = 20
- Locomotion: score = 13
- Social Cognition: score = 12
- Communication: score = 13
Total FIM score = 112
6 minute walk test:
Meters walked in 6 minutes: 302 m
BEST:
I. biomechanical constraints: score =65
II. stability limits/verticality: score =79
III. anticipatory postural adjustments: score =50
IV. postural responses: score=55
V. sensory orientation: score=82
VI. stability in gait:score=70
Discussion[edit | edit source]
This 24 year old patient with CP present to physiotherapy to improve his ability to ambulate, perform ADLs and reduce pain. After 24 weeks of physiotherapy treatment the patient showed on measurable improvements in gait and balance and is more functional and is able to perform ADLs more independently. The patient was discharged with a home exercise program after 24 weeks as he had met all of his goals.
This case study is highly transferable to other similar cases. The patient discussed in the case above represents a very common presentation of individuals with CP. The large majority of people experience spastic CP as this patient did. As well, this patient had many of the common symptoms associated with the condition (3-Odding). This indicates that this case will likely be applicable to the majority of young adults with CP..
The interventions utilized during this 24 weeks treatment plan successfully showed that it is possible to increase independence with structural and function interventions in young adults with CP. These interventions can be impactful in their functional ability to perform ADLs independently. This case study also reiterated that for interventions to be successful they need to be to goal oriented and as well as meaningful to the patient. This was shown in the study above and is important to consider that when designing interventions particularly to populations/patients who are lacking in motivation.
A final implication of this study is in regards to the lack of evidence and research within this population. There is very little guiding material for practicing physiotherapists in regards to working with this patient population. The above case study shows that when there is limited research regarding validated outcome measures, certain measures that have been validated in children (18 and younger) with CP are still used in adult populations both in clinic and research. The case study above shows that this is a successful way to approach the assessment and reassessment of young adults with CP.
Overall, this case was a success and is highly relevant to the current literature and transferable to similar cases, individual patients and populations. This case continues to add to the limited pool of knowledge regarding physiotherapy with young adults with CP. However the greatest implication of this case was that it shows that in situations where patients present with conditions where there is limited evidence on interventions, the utilizations of validated interventions from similar populations with similar symptoms and presentation, success can be found.
Figure References[edit | edit source]
(1) CanChild Centre for Childhood Disability Research.GMFCS – E & R Gross Motor Function Classification System Expanded and Revised. Classification system [internet]. Institute for Applied Health Sciences, McMaster University;2007[cited 2019 May]. Available from:https://canchild.ca/system/tenon/assets/attachments/000/000/058/original/GMFCS-ER_English.pdf
- ↑ Peterson, M., Lukasik, L., Muth, T., Esposito, P., Haapala, H., Gordon, P.,... & Hurvitz, E. (2013). REcumbent Cross-Training is a Feasible and Safe Mode of Physical Activity for Significantly Motor Impaired Adults with Cerebral Palsy. Archive of Physical Medicine and Rehabilitaiton, (94), 401-407.
- ↑ Struass, D., Brooks, J., Rosenbloom, L. & Shavelle, R. (2008). Life expectancy in cerebral palsy: an update. Developmental Medicine and Child Neurology, 50(7).
- ↑ 3.0 3.1 Bottos, M., Feliciangeli, A., Sciuto, L., Gericke, C., & Vianello, A. (2001). Functional status of adults with cerebral palsy and implications for treatment of children. Developmental Medicine and Child Neurology, 43(8), 516–528.
- ↑ 4.0 4.1 4.2 Slaman, J., Roebroeck, M., van der Slot, W., Twisk, J., Wensink, A., Stam, H., van den Berg-Emons, R., and Learn 2 Move Research Group. (2014). Can a Lifestyle Intervention Improve Physical Fitness in Adolescents and Young Adults with Spastic Cerebral Palsy? A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation, 95, 1646-1655.
- ↑ Reddihough DS, Collins KJ. The epidemiology and causes of cerebral palsy. Australian Journal of Physiotherapy. 2003 Jan 1;49(1):7-12. PMID: 12600249
- ↑ 6.0 6.1 6.2 Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disability and Rehabilitation. 2006 Jan 1;28(4):183-91. PMID: 16467053
- ↑ National Institute for Health and Care Excellence. (2008). Cerebral palsy in adults, NICE guideline. Retrieved from: https://www.nice.org.uk/guidance/ng119/resources/cerebral-palsy-in-adults-pdf-66141606816709
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 Rapp CE, Torres MM. The adult with cerebral palsy. Archives of Mamily medicine. 2000 May 1;9(5):466. PMID: 10810953
- ↑ Dobson F, Morris ME, Baker R, Graham HK. Gait classification in children with cerebral palsy: a systematic review. Gait & posture. 2007 Jan 1;25(1):140-52.
- ↑ 10.0 10.1 Palisano RJ, Rosenbaum P, Bartlett D, Livingston MH. Content validity of the expanded and revised Gross Motor Function Classification System. Developmental Medicine & Child Neurology. 2008;50:744-50. PMID: 18834387
- ↑ Morgan PE, Soh SE, McGinley JL. Health-related quality of life of ambulant adults with cerebral palsy and its association with falls and mobility decline: a preliminary cross sectional study. Health and quality of life outcomes. 2014 Dec;12(1):132.PMID: 25176595
- ↑ Bhaumik S, Watson JM, Thorp CF, Tyrer F, McGrother CW. Body mass index in adults with intellectual disability: distribution, associations and service implications: a population‐based prevalence study. Journal of Intellectual Disability Research. 2008 Apr;52(4):287-98.PMID: 18339091
- ↑ Gannotti ME, Gorton III GE, Nahorniak MT, Masso PD. Gait and participation outcomes in adults with cerebral palsy: A series of case studies using mixed methods. Disability and health journal. 2013 Jul 1;6(3):244-52.PMID: 23769484
- ↑ Sandström K. Adults with cerebral palsy: living with a lifelong disability (Doctoral dissertation, Linköping University Electronic Press).2009.URN: urn:nbn:se:liu:diva-15771
- ↑ Andersson C, Asztalos L, Mattsson E. Six-minute walk test in adults with cerebral palsy. A study of reliability. Clinical rehabilitation. 2006 Jun;20(6):488-95.PMID: 16892931
- ↑ Brien M, Sveistrup H. An intensive virtual reality program improves functional balance and mobility of adolescents with cerebral palsy. Pediatric Physical Therapy. 2011 Oct 1;23(3):258-66.PMID: 21829120
- ↑ 17.0 17.1 Opheim A, Jahnsen R, Olsson E, Stanghelle JK. Balance in relation to walking deterioration in adults with spastic bilateral cerebral palsy. Physical Therapy. 2012 Feb 1;92(2):279-88. PMID: 22033070
- ↑ Opheim, Arve, Jahnsen, Reidun, Olsson, Elisabeth, et al. Walking function, pain, and fatigue in adults with cerebral palsy: a 7-year follow-up study. 2009;51(5):381-8.
- ↑ Hutzler Y, Rodrıguez BL, Mendoza Laiz N, Dıez I, Barak S. The effects of an exercise training program on hand and wrist strength, and function, and activities of daily living, in adults with severe Cerebral Palsy. 2013;34(12):4343-54.
- ↑ Lorentzen J, Kirk H, Fernandez-Lago H, Frisk R, Scharff Nielsen N, Jorsal M, et al. Treadmill training with an incline reduces ankle joint stiffness and improves active range of movement during gait in adults with cerebral palsy. Disability & Rehabilitation. 2017;39(10):987-93.
- ↑ Su IYW, Chow DHK. Anticipatory Postural Adjustments in Standing Reach Tasks Among Middle-Aged Adults With Diplegic Cerebral Palsy. Journal of Motor Behavior. 2016;48(4):309-18.
- ↑ 22.0 22.1 22.2 Hesse S., Bertelt C., Jahnke M. T., Schaffrin A., Baake P., Malezic M., et al. Treadmill Training With Partial Body Weight Support Compared With Physiotherapy in Nonambulatory Hemiparetic Patients. Stroke. 1995 Jun 1;26(6):976–81.
- ↑ Schindl MR, Forstner C, Kern H, Hesse S. Treadmill Training With Partial Body Weight Support in Nonambulatory Patients With Cerebral Palsy. 2000;81:6.
- ↑ 24.0 24.1 Kim SJ, Kwak EE, Park ES, Cho S-R. Differential effects of rhythmic auditory stimulation and neurodevelopmental treatment/Bobath on gait patterns in adults with cerebral palsy: a randomized controlled trial. Clinical Rehabilitation. 2012 Oct;26(10):904–14.
- ↑ 25.0 25.1 25.2 Steenbergen B, Crajé C, Nilsen DM, Gordon AM. Motor imagery training in hemiplegic cerebral palsy: a potentially useful therapeutic tool for rehabilitation. Developmental Medicine & Child Neurology. 2009;51(9):690–6.
- ↑ Szturm T, Peters JF, Otto C, Kapadia N, Desai A. Task-specific rehabilitation of finger-hand function using interactive computer gaming. Archives of Physical Medicine & Rehabilitation. 2008 Nov;89(11):2213–7.
- ↑ Brown SH, Lewis CA, McCarthy JM, Doyle ST, Hurvitz EA. The Effects of Internet-Based Home Training on Upper Limb Function in Adults With Cerebral Palsy. Neurorehabilitation and Neural Repair. 2010 Jul;24(6):575–83.