Acute post-surgical management of the amputee: Difference between revisions
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
== Goals of Acute Post-surgical Rehabilitation == | == Goals of Acute Post-surgical Rehabilitation == | ||
*Obtain maximum independence | *Obtain maximum independence | ||
*Prevent oedema | *Prevent oedema | ||
| Line 21: | Line 20: | ||
*Sensory reeducation | *Sensory reeducation | ||
*Support the client psychologically | *Support the client psychologically | ||
<br> | |||
It is intended that prior to any treatment, an [[Assessment of the amputee|assessment]] will be carried out by the physiotherapist. In this early stage, a functional assessment can be done including both upper-limb, lower-limb and trunk in order to evaluate the patient potential to carry out activities such as transfer, wheelchair mobility and ambulation (with or without prosthesis)<ref name="ICRC" /> | It is intended that prior to any treatment, an [[Assessment of the amputee|assessment]] will be carried out by the physiotherapist. In this early stage, a functional assessment can be done including both upper-limb, lower-limb and trunk in order to evaluate the patient potential to carry out activities such as transfer, wheelchair mobility and ambulation (with or without prosthesis)<ref name="ICRC" /> | ||
== Treatment Modalities == | == Treatment Modalities == | ||
Treatment modalities to prevent complications include: | Treatment modalities to prevent complications include: | ||
*Breathing exercises | *Breathing exercises | ||
*AROM | *AROM | ||
| Line 41: | Line 38: | ||
*Positioning | *Positioning | ||
*ADL | *ADL | ||
*Walking and wheelchair use | *Walking and wheelchair use | ||
=== Breathing Exercises === | === Breathing Exercises === | ||
Deep breathing exercises and relaxation exercises will help to increase vital capacity, decrease anxiety and prevent bronchopneumonia. | Deep breathing exercises and relaxation exercises will help to increase vital capacity, decrease anxiety and prevent bronchopneumonia. | ||
=== Active Range of Motion (AROM) === | === Active Range of Motion (AROM) === | ||
Amputated side (from the 1st post op day unless the post surgical dressing restricts motion): | Amputated side (from the 1st post op day unless the post surgical dressing restricts motion): | ||
*First Hip flexion, extension, ADD, ABD | *First Hip flexion, extension, ADD, ABD | ||
*Knee flexion exercises (for below-knee amputations (BKA) | *Knee flexion exercises (for below-knee amputations (BKA) | ||
<br> | |||
Amputated side (from the 3rd post op day) | Amputated side (from the 3rd post op day) | ||
*To reduce oedema BKA amputee should perform alternate knee flexion and extension. | *To reduce oedema BKA amputee should perform alternate knee flexion and extension. | ||
*The knee disarticulation and TF amputee should perform alternate hip flexion and extension, hip ADD and ABD. | *The knee disarticulation and TF amputee should perform alternate hip flexion and extension, hip ADD and ABD. | ||
<br> | |||
These active exercises must be performed at regular intervals during the day (10 repetitions per hour).<br>Bilateral activities often achieve a more vigorous contraction on the amputated side. | These active exercises must be performed at regular intervals during the day (10 repetitions per hour).<br>Bilateral activities often achieve a more vigorous contraction on the amputated side. | ||
| Line 66: | Line 59: | ||
<div class="col-md-6">{{#ev:youtube|ny8c37E3aIU|250}} <div class="text-right"><ref>Ottobock. How to prevent muscle contractures through moving the residual limb?</ref></div></div> | <div class="col-md-6">{{#ev:youtube|ny8c37E3aIU|250}} <div class="text-right"><ref>Ottobock. How to prevent muscle contractures through moving the residual limb?</ref></div></div> | ||
</div> | </div> | ||
=== Resistance Exercises === | === Resistance Exercises === | ||
From the 1st post op day | From the 1st post op day | ||
*Isometric contraction of the quadriceps (BKA) | *Isometric contraction of the quadriceps (BKA) | ||
*Isometric contraction of gluteal muscles, adductors and hip internal rotation | *Isometric contraction of gluteal muscles, adductors and hip internal rotation | ||
*Strengthening exercises of the sound lower limb (in progression) | *Strengthening exercises of the sound lower limb (in progression) | ||
<br> | |||
From the 3rd post-op day | From the 3rd post-op day | ||
*Resistance exercises of the upper limbs | *Resistance exercises of the upper limbs | ||
*Resistance exercises of the torso | *Resistance exercises of the torso | ||
{{#ev:youtube|BtU7woXwG0g|250}} <div class="text-right"><ref>Ottobock. Muscle strengthening after amputation. Jan 2019</ref></div> | {{#ev:youtube|BtU7woXwG0g|250}} <div class="text-right"><ref>Ottobock. Muscle strengthening after amputation. Jan 2019</ref></div> | ||
=== Passive Range of Motion === | === Passive Range of Motion === | ||
Passive extension of a TT residual limb.<ref name="icrc">Prosthetic gait analysis, a course manual for physiotherapists, ICRC, 2014</ref><br> | Passive extension of a TT residual limb.<ref name="icrc">Prosthetic gait analysis, a course manual for physiotherapists, ICRC, 2014</ref><br> | ||
<gallery widths="100px" heights="140px"> | <gallery widths="100px" heights="140px"> | ||
| Line 91: | Line 79: | ||
File: PROM2.png | File: PROM2.png | ||
File: PROM3.png | File: PROM3.png | ||
</gallery> | |||
The physiotherapist's hands should be positioned as proximal as possible to avoid any contact with the end of the stump, which is a very sensitive area. | The physiotherapist's hands should be positioned as proximal as possible to avoid any contact with the end of the stump, which is a very sensitive area. | ||
=== Massage, Tapping, Desensitisation, and Scar Mobilisation === | === Massage, Tapping, Desensitisation, and Scar Mobilisation === | ||
Desensitisation is believed to reduce [[Amputation Pain Rehabilitation|pain]], help with tolerance and touch in the residual limb and may help the patient with an [[Amputations|amputation]] adjust to his or her new body image that now includes limb loss. Massage and tapping can be started early on and could be done over the soft dressing or when it is off.<ref name=":0">''Rossbach P.'' Care of Your Wounds After Amputation Surgery. Amputee Coalition. Available from: https://www.amputee-coalition.org/resources/after-amputation-surgery/ [Accessed 23 Nov 2017]</ref> All these techniques could be done by the therapist and also taught to the patient/family member to do. Also, instruct the patient how to perform desensitization and distraction techniques to reduce the phantom pain. | Desensitisation is believed to reduce [[Amputation Pain Rehabilitation|pain]], help with tolerance and touch in the residual limb and may help the patient with an [[Amputations|amputation]] adjust to his or her new body image that now includes limb loss. Massage and tapping can be started early on and could be done over the soft dressing or when it is off.<ref name=":0">''Rossbach P.'' Care of Your Wounds After Amputation Surgery. Amputee Coalition. Available from: https://www.amputee-coalition.org/resources/after-amputation-surgery/ [Accessed 23 Nov 2017]</ref> All these techniques could be done by the therapist and also taught to the patient/family member to do. Also, instruct the patient how to perform desensitization and distraction techniques to reduce the phantom pain. | ||
<br> | |||
*Massage<ref name=":0" /> | *Massage<ref name=":0" /> | ||
**[[Massage]] the entire residual limb with 1 or 2 hands by doing soft gentle kneading. Be cautious over the sutured area. | **[[Massage]] the entire residual limb with 1 or 2 hands by doing soft gentle kneading. Be cautious over the sutured area. | ||
| Line 126: | Line 113: | ||
== Stump Management == | == Stump Management == | ||
The ideal stump is one that is well-healed, has good vascular supply, soft and mobile scars, minimal pain, minimal oedema, a length sufficient for biomechanical leverage but not too long to restrict choices for prosthetic components, and large surface areas for distribution of pressure. While the surgery plays a large part in creating the ideal stump, Physiotherapy is required to maximise chances of achieving this ideal. | The ideal stump is one that is well-healed, has good vascular supply, soft and mobile scars, minimal pain, minimal oedema, a length sufficient for biomechanical leverage but not too long to restrict choices for prosthetic components, and large surface areas for distribution of pressure. While the surgery plays a large part in creating the ideal stump, Physiotherapy is required to maximise chances of achieving this ideal. | ||
| Line 132: | Line 118: | ||
=== Post-operative Dressing === | === Post-operative Dressing === | ||
Post operative dressings are used to protect the limb, reduce swelling, promote limb maturation and prevent contractures. There are two major classifications of post operative dressing that are commonly used: | Post operative dressings are used to protect the limb, reduce swelling, promote limb maturation and prevent contractures. There are two major classifications of post operative dressing that are commonly used: | ||
*'''Soft Dressings''' | *'''Soft Dressings''' | ||
**Descriptive studies indicate several disadvantages of soft dressings, such as high local or proximal pressure, tendency to loosen or fall off, limited mobilization, and extended hospital stays. | **Descriptive studies indicate several disadvantages of soft dressings, such as high local or proximal pressure, tendency to loosen or fall off, limited mobilization, and extended hospital stays. | ||
| Line 154: | Line 138: | ||
=== Oedema Control (Shrinking) === | === Oedema Control (Shrinking) === | ||
In the BACPAR Guidelines for oedema management in lower limb amputees<ref name="BACPAR">Elizabeth Bouch, Katie Burns, Elizabeth Geer, Matthew Fuller and Anna Rose. [https://bacpar.csp.org.uk/system/files/guidance_v.8_0.pdf Guidance for the multi disciplinary team on the management of postoperative residuum oedema in lower limb amputees]. BACPAR</ref> they conclude that based on the best current available evidence Rigid/semi-Rigid dressings should be used when expertise, time and resources allow; the benefits are well documented in the literature. The PPAM aid, compression socks and stump boards have been shown to have some evidence base for oedema control and may be used in addition or in the absence of Rigid dressings dependent on clinical judgement. However, these modalities are not necessarily primarily intended for use for oedema control. Their advantages include preparation for prosthetic rehabilitation, reduction in flexion deformities and maintenance/improvement in muscle tone and are important components of amputee rehabilitation. Compression socks and the PPAM aid are the only tools available for transfemoral amputees. Although compression socks are widely used as a form of oedema control there is very limited evidence on aspects such as the timing of the application, who should assess the appropriateness and the frequency it should be worn for. It is suggested that further research is required in order to offer more clarity for clinicians in these areas.<ref name="BACPAR" /> | In the BACPAR Guidelines for oedema management in lower limb amputees<ref name="BACPAR">Elizabeth Bouch, Katie Burns, Elizabeth Geer, Matthew Fuller and Anna Rose. [https://bacpar.csp.org.uk/system/files/guidance_v.8_0.pdf Guidance for the multi disciplinary team on the management of postoperative residuum oedema in lower limb amputees]. BACPAR</ref> they conclude that based on the best current available evidence Rigid/semi-Rigid dressings should be used when expertise, time and resources allow; the benefits are well documented in the literature. The PPAM aid, compression socks and stump boards have been shown to have some evidence base for oedema control and may be used in addition or in the absence of Rigid dressings dependent on clinical judgement. However, these modalities are not necessarily primarily intended for use for oedema control. Their advantages include preparation for prosthetic rehabilitation, reduction in flexion deformities and maintenance/improvement in muscle tone and are important components of amputee rehabilitation. Compression socks and the PPAM aid are the only tools available for transfemoral amputees. Although compression socks are widely used as a form of oedema control there is very limited evidence on aspects such as the timing of the application, who should assess the appropriateness and the frequency it should be worn for. It is suggested that further research is required in order to offer more clarity for clinicians in these areas.<ref name="BACPAR" /> | ||
| Line 170: | Line 153: | ||
=== Wound Healing === | === Wound Healing === | ||
Wound healing is always a cause of concern, but especially in the dysvascular population. Adequately controlling oedema of the stump can assist with healing, but some evidence also supports the use of [http://www.scielo.br/pdf/jvb/v6n3/v6n3a09 low intensity laser in order to facilitate and speed up wound healing] in diabetic patients <ref name="johannesson" />. However the exact dosages for optimal effect has not yet been established. | Wound healing is always a cause of concern, but especially in the dysvascular population. Adequately controlling oedema of the stump can assist with healing, but some evidence also supports the use of [http://www.scielo.br/pdf/jvb/v6n3/v6n3a09 low intensity laser in order to facilitate and speed up wound healing] in diabetic patients <ref name="johannesson" />. However the exact dosages for optimal effect has not yet been established. | ||
=== Pain === | === Pain === | ||
Pain is a very common physiological stressor that occurs during the acute postoperative period and affects the patient’s ability to learn new skills <ref name="lusardi" />. Adequately controlling the new amputee’s levels of pain greatly facilitates their early rehabilitation <ref name="lusardi" /> . Physiotherapists should take this into consideration, and treat patients shortly after receiving their pain medication. Controlling oedema in the residual limb through positioning also assists in relieving acute postoperative pain <ref name="lusardi" />. Various physiotherapy interventions are used for the management of phantom limb pain, but very few of these have been studied to prove their efficacy in the research literature <ref name="mulvey">Mulvey MR, Radford HE, Fawkner HJ, Hirst L, Neumann V, Johnson MI. Transcutaneous electrical nerve stimulation for phantom pain and stump pain in adult amputees. Pain Practice. 2013; 13(4):289-96. fckLRdoi: 10.1111/j.1533-2500.2012.00593.x</ref>. One of the few physiotherapy modalities that has been proven to be effective for the management of phantom limb pain, is a 60 minute application of [[Transcutaneous Electrical Nerve Stimulation (TENS)|Transcutaneous Electrical Nerve Stimulation]] (TENS) <ref name="bryant" />. | Pain is a very common physiological stressor that occurs during the acute postoperative period and affects the patient’s ability to learn new skills <ref name="lusardi" />. Adequately controlling the new amputee’s levels of pain greatly facilitates their early rehabilitation <ref name="lusardi" /> . Physiotherapists should take this into consideration, and treat patients shortly after receiving their pain medication. Controlling oedema in the residual limb through positioning also assists in relieving acute postoperative pain <ref name="lusardi" />. Various physiotherapy interventions are used for the management of phantom limb pain, but very few of these have been studied to prove their efficacy in the research literature <ref name="mulvey">Mulvey MR, Radford HE, Fawkner HJ, Hirst L, Neumann V, Johnson MI. Transcutaneous electrical nerve stimulation for phantom pain and stump pain in adult amputees. Pain Practice. 2013; 13(4):289-96. fckLRdoi: 10.1111/j.1533-2500.2012.00593.x</ref>. One of the few physiotherapy modalities that has been proven to be effective for the management of phantom limb pain, is a 60 minute application of [[Transcutaneous Electrical Nerve Stimulation (TENS)|Transcutaneous Electrical Nerve Stimulation]] (TENS) <ref name="bryant" />. | ||
| Line 180: | Line 161: | ||
=== Patient Information === | === Patient Information === | ||
A series of useful patient information guides from the [http://www.amputee-coalition.org/ Amputee Coalition]. | A series of useful patient information guides from the [http://www.amputee-coalition.org/ Amputee Coalition]. | ||
*{{pdf|Perioperative_Pain_Management_Preview.pdf |Perioperative_Pain_Management_Preview}} | *{{pdf|Perioperative_Pain_Management_Preview.pdf |Perioperative_Pain_Management_Preview}} | ||
*{{pdf|Avoiding_Secondary_Pain_Preview.pdf|Avoiding_Secondary_Pain_Preview}} | *{{pdf|Avoiding_Secondary_Pain_Preview.pdf|Avoiding_Secondary_Pain_Preview}} | ||
| Line 189: | Line 168: | ||
*{{pdf|Care_of_Your_Wounds_Preview.pdf|Care_of_Your_Wounds_Preview}} | *{{pdf|Care_of_Your_Wounds_Preview.pdf|Care_of_Your_Wounds_Preview}} | ||
== Bed Mobility | == Bed Mobility== | ||
*Bridging | *Bridging | ||
*Rolling | *Rolling | ||
| Line 204: | Line 183: | ||
== Transfers == | == Transfers == | ||
*Standing pivot transfer (for a patient that can participate only partially) | *Standing pivot transfer (for a patient that can participate only partially) | ||
*Backwards forwards transfer (for patient with a bilateral amputation) | *Backwards forwards transfer (for patient with a bilateral amputation) | ||
| Line 223: | Line 201: | ||
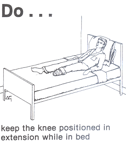
=== Positioning === | === Positioning === | ||
The main goal of a good positioning at any time is to prevent adjacent joint contractures. | The main goal of a good positioning at any time is to prevent adjacent joint contractures. | ||
*For trans-tibial amputee complete knee extension and flexion is needed and | *For trans-tibial amputee complete knee extension and flexion is needed and | ||
*For the trans-femoral amputee and knee disarticulation amputee - the full ROM of the hip, especially extension and adduction. | *For the trans-femoral amputee and knee disarticulation amputee - the full ROM of the hip, especially extension and adduction. | ||
| Line 232: | Line 208: | ||
Patient should be advised on how to position themselves while sitting and lying in the hospital bed or standing to prevent contractures. | Patient should be advised on how to position themselves while sitting and lying in the hospital bed or standing to prevent contractures. | ||
*For trans tibial: avoid as much as possible long position with a knee flexion (cushion under the knee for example) | *For trans tibial: avoid as much as possible long position with a knee flexion (cushion under the knee for example) | ||
*For trans femoral: avoid position with hip flexion and abduction (cushion under the stump for example). <br> | *For trans femoral: avoid position with hip flexion and abduction (cushion under the stump for example). <br> | ||
| Line 268: | Line 243: | ||
<div class="row"><div class="col-md-6"> {{#ev:youtube|YBi5t2ulhLA|250}} <div class="text-middle"><ref>Using Crutches After Lower Limb Amputation. Available from: https://youtu.be/YBi5t2ulhLA</ref></div></div> | <div class="row"><div class="col-md-6"> {{#ev:youtube|YBi5t2ulhLA|250}} <div class="text-middle"><ref>Using Crutches After Lower Limb Amputation. Available from: https://youtu.be/YBi5t2ulhLA</ref></div></div> | ||
</div> | </div> | ||
== Resources == | == Resources == | ||
*[http://www.austpar.com/portals/acute_care/post-op.php Post-Operative Physiotherapy] from AustPAR | *[http://www.austpar.com/portals/acute_care/post-op.php Post-Operative Physiotherapy] from AustPAR | ||
*Van Velzen AD, Nederhand MJ, Emmelot CH, IJzerman MJ. Early treatment of trans-tibial amputees: retrospective analysis of early fitting and elastic bandaging. Prosthetics and orthotics international. 2005 Apr;29(1):3-12. Available at: https://www.roessingh.nl/downloads/Early_treatment_of_trans-tibial_amputees_retrospective_analysis_of_early_fitting_and_elastic_bandaging.pdf | *Van Velzen AD, Nederhand MJ, Emmelot CH, IJzerman MJ. Early treatment of trans-tibial amputees: retrospective analysis of early fitting and elastic bandaging. Prosthetics and orthotics international. 2005 Apr;29(1):3-12. Available at: https://www.roessingh.nl/downloads/Early_treatment_of_trans-tibial_amputees_retrospective_analysis_of_early_fitting_and_elastic_bandaging.pdf | ||
| Line 277: | Line 252: | ||
== References == | == References == | ||
<references /> | <references /> | ||
| Line 283: | Line 257: | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Rehabilitation Protocols]] | [[Category:Rehabilitation Protocols]] | ||
[[Category:Positioning]] | |||
Revision as of 13:09, 7 April 2023
Original Editor - Liezel Wegner as part of the World Physiotherapy Network for Amputee Rehabilitation Project
Top Contributors - Admin, Tarina van der Stockt, Tony Lowe, Aicha Benyaich, Kim Jackson, Naomi O'Reilly, Sheik Abdul Khadir, Andeela Hafeez, Rucha Gadgil, Olajumoke Ogunleye and Jorge Rodríguez Palomino
Introduction[edit | edit source]
It is important to remember that the earlier the onset of rehabilitation, the greater the potential for success will be. The patient needs to receive physiotherapy treatment early to avoid complications such as joint contractures, pathological scars and depressed psychological state. The main post-surgical complications are cardio-vascular, residual limb pain and phantom sensation, oedema, contracture and wound dehiscence. [1]
Goals of Acute Post-surgical Rehabilitation [edit | edit source]
- Obtain maximum independence
- Prevent oedema
- Maintain joint ROM
- Prevent amyotrophy (muscle atrophy)
- Increase the muscular activation
- Prevent muscular weakness
- Prevent bronchopneumonia
- Prevent pressure sores
- Control pain
- Sensory reeducation
- Support the client psychologically
It is intended that prior to any treatment, an assessment will be carried out by the physiotherapist. In this early stage, a functional assessment can be done including both upper-limb, lower-limb and trunk in order to evaluate the patient potential to carry out activities such as transfer, wheelchair mobility and ambulation (with or without prosthesis)[1]
Treatment Modalities[edit | edit source]
Treatment modalities to prevent complications include:
- Breathing exercises
- AROM
- Resistance exercises
- PROM
- Desensitising techniques
- Stump management
- Dressings
- Prevention of oedema
- Wound healing
- Pain
- Bed mobility and transfers
- Positioning
- ADL
- Walking and wheelchair use
Breathing Exercises[edit | edit source]
Deep breathing exercises and relaxation exercises will help to increase vital capacity, decrease anxiety and prevent bronchopneumonia.
Active Range of Motion (AROM)[edit | edit source]
Amputated side (from the 1st post op day unless the post surgical dressing restricts motion):
- First Hip flexion, extension, ADD, ABD
- Knee flexion exercises (for below-knee amputations (BKA)
Amputated side (from the 3rd post op day)
- To reduce oedema BKA amputee should perform alternate knee flexion and extension.
- The knee disarticulation and TF amputee should perform alternate hip flexion and extension, hip ADD and ABD.
These active exercises must be performed at regular intervals during the day (10 repetitions per hour).
Bilateral activities often achieve a more vigorous contraction on the amputated side.
Resistance Exercises[edit | edit source]
From the 1st post op day
- Isometric contraction of the quadriceps (BKA)
- Isometric contraction of gluteal muscles, adductors and hip internal rotation
- Strengthening exercises of the sound lower limb (in progression)
From the 3rd post-op day
- Resistance exercises of the upper limbs
- Resistance exercises of the torso
Passive Range of Motion[edit | edit source]
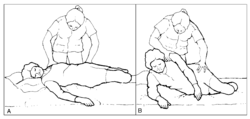
Passive extension of a TT residual limb.[5]
The physiotherapist's hands should be positioned as proximal as possible to avoid any contact with the end of the stump, which is a very sensitive area.
Massage, Tapping, Desensitisation, and Scar Mobilisation[edit | edit source]
Desensitisation is believed to reduce pain, help with tolerance and touch in the residual limb and may help the patient with an amputation adjust to his or her new body image that now includes limb loss. Massage and tapping can be started early on and could be done over the soft dressing or when it is off.[6] All these techniques could be done by the therapist and also taught to the patient/family member to do. Also, instruct the patient how to perform desensitization and distraction techniques to reduce the phantom pain.
- Massage[6]
- Massage the entire residual limb with 1 or 2 hands by doing soft gentle kneading. Be cautious over the sutured area.
- Once the sutures or clips are removed you can increase the pressure on the deeper muscles and soft tissue.
- 5 Minutes 3-4 a day or as needed to reduce phantom limb pain.
- Gently massage the proximal residual limb, to include pressure points in the inguinal region
- Tapping [6]
- The residual limb should be tapped with fingertips (not the fingernails).
- When the sutures or clips are still in then gentle tapping could be done over the suture line
- This could also be done over the Rigid or soft dressing
- Once the sutures are removed a slapping motion could be done on the residual limb
- Desensitisation[6]
- This helps to make the residual limb less sensitive to touch and will improve the tolerance to touch.
- 2-3 times a day when the soft dressing is off (this could be done during or after bathing)
- Start by using a soft material, like a cotton ball, to gently rub the skin in circular motions.
- Progress by using a rougher material, like a paper towel, and then progress to a towel or cloth until you can tolerate these materials.
- Scar Mobilisation[6]
- This will keep the scar from adhering to the underlying tissue as it could be the cause of pain and blisters when the patient starts wearing a prosthesis.
- Performed when the soft dressing or compression is off.
- The patient can do this daily when taking a bath
- Place two fingers over a bony portion and by keeping the fingers on the same spot make a circular motion for 1 minute.
- Repeat this over and around the bone on the residual limb
- After wound healing, this could be done over the incision line to mobilise the scar tissue
Stump Management[edit | edit source]
The ideal stump is one that is well-healed, has good vascular supply, soft and mobile scars, minimal pain, minimal oedema, a length sufficient for biomechanical leverage but not too long to restrict choices for prosthetic components, and large surface areas for distribution of pressure. While the surgery plays a large part in creating the ideal stump, Physiotherapy is required to maximise chances of achieving this ideal.
One of the main acute post-operative factors affecting the time to prosthetic fitting and the speed of rehabilitation, is the wound healing of the stump, especially in the vulnerable vascular compromised population[8]. Oedema in the residual limb is also a common complication after LLA surgery[9]. Controlling the amount of oedema post-surgically is vital for promoting wound-healing, pain control, protecting the incision during rehabilitation and assisting in shaping the stump for prosthetic fitting[10]. Traditionally soft dressings or non-adhesive elastic bandages are used to prevent oedema of the stump post-surgically, but no evidence supports the use of these bandages[11][12]. The use of immediate post-surgical Rigid or semi-Rigid dressings to prevent acute oedema have increased in popularity in the developed world and is well supported by evidence in the literature[10][11].
Post-operative Dressing[edit | edit source]
Post operative dressings are used to protect the limb, reduce swelling, promote limb maturation and prevent contractures. There are two major classifications of post operative dressing that are commonly used:
- Soft Dressings
- Descriptive studies indicate several disadvantages of soft dressings, such as high local or proximal pressure, tendency to loosen or fall off, limited mobilization, and extended hospital stays.
- Controlled studies found that the frequency of uncomplicated healing rates, postoperative pain, the eventual use of a prosthesis, and mortality were not significantly different between soft and Rigid types of dressings[13].
- Rigid Dressings - Rigid dressings have been used as best practice for post-operative stump management for many years.
- They come in 2 types:
- non removable thigh length casts, which protect the stump and maintain the knee in extension; and
- removable Rigid dressings where the cast enclose the stump to just below the knee, thus allowing the amputee to have knee flexion, and are easily removable to allow inspection of the stump. (for evidence of use see[13])
- Some of the reported benefits of the Rigid dressing include the promotion of wound healing, shaping of the stump, pain management, protection against trauma during falls, stump volume control and increased speed of prosthetic fitting[10][11].
- The conventional method of application of Rigid dressings is a plaster cast Rigid dressing that is usually applied in theatre under anaesthesia. This method has proven to be effective, but often surgeons choose not to opt for this method of Rigid dressing since it is time-consuming, and requires some skill to apply[14]
- They come in 2 types:
- Removable Rigid Dressing (Semi-Rigid Dressing)
- An alternative vacuum-formed removable Rigid dressing has proven to be as effective as the conventional Rigid dressing in a randomized controlled trial, and is a useful alternative to the plaster casting method[8].
- The advantages of this Removable Rigid Dressing include the ease of application and ease of access for wound inspection[8][15]. This dressing can be used for 5-7 days after surgery.
- Prefabricated removable dressings also exist (see image)
- Reichmann et al reviewed the available (15) articles on the use of Removable Rigid Dressings (RRDs) and found the following:[15]
- When compared to soft dressing, RRDs is better as it leads to improved healing times, less oedema, shaping of the residual limb, prevention of knee flexion contractures, and prevents trauma to the amputated limb.
- According to this review, non weight bearing RRDs should be the first option in the treatment of below knee amputees after surgery
Oedema Control (Shrinking)[edit | edit source]
In the BACPAR Guidelines for oedema management in lower limb amputees[16] they conclude that based on the best current available evidence Rigid/semi-Rigid dressings should be used when expertise, time and resources allow; the benefits are well documented in the literature. The PPAM aid, compression socks and stump boards have been shown to have some evidence base for oedema control and may be used in addition or in the absence of Rigid dressings dependent on clinical judgement. However, these modalities are not necessarily primarily intended for use for oedema control. Their advantages include preparation for prosthetic rehabilitation, reduction in flexion deformities and maintenance/improvement in muscle tone and are important components of amputee rehabilitation. Compression socks and the PPAM aid are the only tools available for transfemoral amputees. Although compression socks are widely used as a form of oedema control there is very limited evidence on aspects such as the timing of the application, who should assess the appropriateness and the frequency it should be worn for. It is suggested that further research is required in order to offer more clarity for clinicians in these areas.[16]
Another option is the use of a post-op silicone liner:[17]
- it is applied after the Removable Rigid Dressing is taken off
- the same level of compression is applied to the residuum even if different people apply it
- it decreases oedema and shapes the residuum for prosthetic fitting
- helps with pain relief
- fast track the rehabilitation process
- It can be sterilized
- the liner size is prescribed according to the circumference of the residuum and can be changed when the oedema decreases
- Disadvantages are: the cost involved, as the oedema goes down another size silicone liner needs to be applied, not readily available
Wound Healing[edit | edit source]
Wound healing is always a cause of concern, but especially in the dysvascular population. Adequately controlling oedema of the stump can assist with healing, but some evidence also supports the use of low intensity laser in order to facilitate and speed up wound healing in diabetic patients [8]. However the exact dosages for optimal effect has not yet been established.
Pain[edit | edit source]
Pain is a very common physiological stressor that occurs during the acute postoperative period and affects the patient’s ability to learn new skills [10]. Adequately controlling the new amputee’s levels of pain greatly facilitates their early rehabilitation [10] . Physiotherapists should take this into consideration, and treat patients shortly after receiving their pain medication. Controlling oedema in the residual limb through positioning also assists in relieving acute postoperative pain [10]. Various physiotherapy interventions are used for the management of phantom limb pain, but very few of these have been studied to prove their efficacy in the research literature [18]. One of the few physiotherapy modalities that has been proven to be effective for the management of phantom limb pain, is a 60 minute application of Transcutaneous Electrical Nerve Stimulation (TENS) [9].
For more information see the pain management of the amputee page.
Patient Information[edit | edit source]
A series of useful patient information guides from the Amputee Coalition.
- Perioperative_Pain_Management_Preview
- Avoiding_Secondary_Pain_Preview
- Living_with_Residual_Limb_Pain_Preview
- Living_with_Phantom_Limb_Pain_Preview_(1)
- Care_of_Your_Wounds_Preview
Bed Mobility[edit | edit source]
- Bridging
- Rolling
- Sitting up in bed
- Scooting over to the side in lying and sitting
- Moving up and down on the bed.
- Push-ups using arms (after drain has been removed)
- Balance in sitting on the side or with legs on the bed[19]
Transfers[edit | edit source]
- Standing pivot transfer (for a patient that can participate only partially)
- Backwards forwards transfer (for patient with a bilateral amputation)
- Lateral transfer with a sliding board transfer
Positioning[edit | edit source]
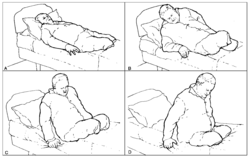
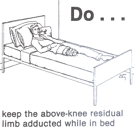
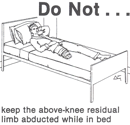
The main goal of a good positioning at any time is to prevent adjacent joint contractures.
- For trans-tibial amputee complete knee extension and flexion is needed and
- For the trans-femoral amputee and knee disarticulation amputee - the full ROM of the hip, especially extension and adduction.
Full ROM will ease prosthetic fitting and ambulation. [1]
Patient should be advised on how to position themselves while sitting and lying in the hospital bed or standing to prevent contractures.
- For trans tibial: avoid as much as possible long position with a knee flexion (cushion under the knee for example)
- For trans femoral: avoid position with hip flexion and abduction (cushion under the stump for example).
Bed Positioning for Trans-femoral [22]
Bed Positioning for Trans-tibial [22]
Sitting in a Wheelchair for Trans-tibial [22]
Wheelchair Management[edit | edit source]
- Teach the patient how to propel the wheelchair safely
- Provide a stump boar/ knee extender for patients with a below or through knee amputation
- A seat belt might be necessary for patients with poor balance, or a very high or bilateral above knee amputations
- A patient that is confused should be monitored[19]
Mobilising with Crutches or a Walking Frame[edit | edit source]
- Some patients may not want to use a wheelchair, especially young, agile and fit patients [19]
- Make sure you explain to the patient the dangers of the dependent position (residual limb hanging down) in the early post op phase as this may increase oedema, pain and healing time. [19]
- Use a gait belt with mobilising and transfers when using
- When mobilising the patient should have the Rigid Removable Dressing on to protect the limb
- Give education on preventing falls
Resources[edit | edit source]
- Post-Operative Physiotherapy from AustPAR
- Van Velzen AD, Nederhand MJ, Emmelot CH, IJzerman MJ. Early treatment of trans-tibial amputees: retrospective analysis of early fitting and elastic bandaging. Prosthetics and orthotics international. 2005 Apr;29(1):3-12. Available at: https://www.roessingh.nl/downloads/Early_treatment_of_trans-tibial_amputees_retrospective_analysis_of_early_fitting_and_elastic_bandaging.pdf
- Rigid Dressings from AustPAR
- Amputee Care - The Use of Post-Operative Rigid Dressings for Trans-Tibial Amputees. Department of Health, NSW
- Rigid removable dressing. Amputee Information. Physiotherapy Department, The Queen Elizabeth Hospital, Woodville West, SA
References[edit | edit source]
- ↑ 1.0 1.1 1.2 International Committee of the Red Cross (ICRC), ICRC physiotherapy reference manual: prothetic gait analysis, 2014
- ↑ Ottobock. First exercises after amputation. Jan 2019
- ↑ Ottobock. How to prevent muscle contractures through moving the residual limb?
- ↑ Ottobock. Muscle strengthening after amputation. Jan 2019
- ↑ Prosthetic gait analysis, a course manual for physiotherapists, ICRC, 2014
- ↑ 6.0 6.1 6.2 6.3 6.4 Rossbach P. Care of Your Wounds After Amputation Surgery. Amputee Coalition. Available from: https://www.amputee-coalition.org/resources/after-amputation-surgery/ [Accessed 23 Nov 2017]
- ↑ YouTube Video. AmputeeOT: Massage, Scar Mobilization, Desensitization, and End-Bearing Exercises for New Amputees. Available from: https://youtu.be/AqmKhuT-mWw [Accessed 23 Nov 2017]
- ↑ 8.0 8.1 8.2 8.3 Johannesson A, Larsson G, Oberg,T Atroshi, I. Comparison of vacuum-formed removable rigid dressing with conventional rigid dressing after transtibial amputation. Acta Orthopeadica 2008;79(3); 361-369
- ↑ 9.0 9.1 Bryant G. Stump Care. The American Journal of Nursing 2001; 101(2); 67-71
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 Lusardi MM, Postoperative and preprosthetic care. In Lusardi, MM, Jorge, M and Nielsen, CC editors. Orthotics and Prosthetics in Rehabilitation, Third Edition. Missouri: Elsevier, 2013.p. 532-594.
- ↑ 11.0 11.1 11.2 Nawijn SE, Van der Linde H, Emmelot CH, Hofstad CJ. Stump management after transtibial amputation: a systematic review. Prosthetics and Orthotics International 2005; 29(1); 13-26.
- ↑ Smith DG, McFarland LV, Sangeorzan BJ, Reiber GE, Czerniecki JM. Postoperative dressing and management strategies for transtibial amputations: A critical review. Journal of Rehabilitation Research Development 2003; 40; 213-224. Available at: https://pdfs.semanticscholar.org/4013/c8651aa3be7c9e26dff68253082fd9f3215d.pdf [Accessed 10 Oct 2017]
- ↑ 13.0 13.1 Clinical Practice Guideline for Rehabilitation of Lower Limb Amputation (full version). Department of Veterans Affairs, Department of Defence, 2007, page 72-73
- ↑ Johannesson A, Larsson G, Ramstrand N, Lauge-Pedersen H, Wagner P, Atroshi I. Outcomes of a standardized surgical and rehabilitation program in trans-tibial amputation for peripheral vascular disease: A 10 year prospective cohort study. The American Journal of Physical Medicine and Rehabilitation / Association of Academic Physiatrists 2010; 89(4); 293-303.
- ↑ 15.0 15.1 Reichmann JP, Stevens PM, Rheinstein J, Kreulen CD. Removable Rigid Dressings for Postoperative Management of Transtibial Amputations: A Review of Published Evidence. PM&R. 2018 May 1;10(5):516-23.
- ↑ 16.0 16.1 Elizabeth Bouch, Katie Burns, Elizabeth Geer, Matthew Fuller and Anna Rose. Guidance for the multi disciplinary team on the management of postoperative residuum oedema in lower limb amputees. BACPAR
- ↑ Johannesson A, Larsson GU, Öberg T. From major amputation to prosthetic outcome: a prospective study of 190 patients in a defined population. Prosthetics and orthotics international. 2004 Jan 1;28(1):9-21. Available at: https://www.researchgate.net/publication/8534355_From_major_amputation_to_prosthetic_outcome_A_prospective_study_of_190_patients_in_a_defined_population[Accessed 11 Oct 2017]
- ↑ Mulvey MR, Radford HE, Fawkner HJ, Hirst L, Neumann V, Johnson MI. Transcutaneous electrical nerve stimulation for phantom pain and stump pain in adult amputees. Pain Practice. 2013; 13(4):289-96. fckLRdoi: 10.1111/j.1533-2500.2012.00593.x
- ↑ 19.0 19.1 19.2 19.3 Barbara Engstrom and Catherine Van de Ven. Therapy for Amputees, 3rd Edition. 1999.
- ↑ YouTube Video. Northshore Sota. 2x Amputee Sliding Board MinA WC to Bed. Available from: https://youtu.be/k3nQfbx1ASk [last accessed 2/12/17]
- ↑ YouTube Video. Wheelchair Transfer - Amputee Life Hack. Available from: https://youtu.be/ngM3bgdsR2g [last accessed 4/13/19]
- ↑ 22.0 22.1 22.2 Bella J. May, AMPUTATIONS AND PROSTHETICS, F.A Davis Company, 2rd édition, 1996
- ↑ Using Crutches After Lower Limb Amputation. Available from: https://youtu.be/YBi5t2ulhLA