Acute Coronary Syndrome: Difference between revisions
Haseel Bhatt (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (48 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original | '''Original Editor '''- [[User:Haseel Bhatt|Haseel Bhatt]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
[[File:ACS scheme.jpeg|right|frameless|399x399px]] | |||
Acute coronary syndrome (ACS) is a group of cardiac diagnoses along a spectrum of severity due to the interruption of [[Coronary Artery|coronary blood flow]] to the myocardium, which in decreasing severity are: | |||
# ST elevation [[Myocardial Infarction|myocardial infarction]] (STEMI): Very serious type of heart attack during which one of the [[Anatomy of the Human Heart|heart]]’s major arteries is blocked. The classic heart attack. | |||
# Non-ST elevation [[Myocardial Infarction|myocardial infarction]] (NSTEMI): The "intermediate" form of ACS, a blockage either occurs in a minor coronary artery or causes partial obstruction of a major coronary artery. Symptoms can be the same as STEMI but the heart damage is far less extensive<ref>Very Well Health [https://www.verywellhealth.com/non-st-segment-elevation-myocardial-infarction-nstemi-1746017 Non-ST Segment Myocardial Infarction] Overview Available from:https://www.verywellhealth.com/non-st-segment-elevation-myocardial-infarction-nstemi-1746017 (accessed 26.5.2021)</ref>. | |||
# Unstable [[angina]]: Thrombus partially or intermittently occludes the coronary artery. | |||
== | Stable angina is not considered an ACS.<ref name=":0">Radiopedia ACS Available: https://radiopaedia.org/articles/acute-coronary-syndrome<nowiki/>(accessed 26.5.2021)</ref><ref name="ART2">Aragam, K.G. & Bhatt, D.L., 2011. Antiplatelet therapy in acute coronary syndromes. Journal of cardiovascular pharmacology and therapeutics, 16(1), pp.24–42</ref> | ||
ACS is a type of [[Coronary Artery Disease (CAD)|coronary artery disease]] (CAD), which is responsible for one-third of total deaths in people older than 35. Some forms of CAD can be asymptomatic, but '''ACS is always symptomatic'''.<ref name=":1">Singh A, Museedi AS, Grossman SA. [https://www.ncbi.nlm.nih.gov/books/NBK459157/ Acute coronary syndrome].Available from: https://www.ncbi.nlm.nih.gov/books/NBK459157/<nowiki/>(accessed 26.5.20210</ref><br> | |||
== [[Epidemiology, Prevalence and Incidence|Epidemiology]] == | |||
[[File:Causes of death worldwide 2011.png|right|frameless]] | |||
Of all patients who present to emergency departments with symptoms of ACS, only 20-25% will have ACS confirmed as their discharge diagnosis.<ref name=":0" /> | |||
* Acute coronary syndromes (ACS) and sudden death cause most ischaemic heart disease(IHD)-related deaths, which represent 1.8 million deaths per year. | |||
* The incidence of IHD in general, and of ACS, increases with [[Cardiovascular Considerations in the Older Patient|age]] although, on average, this occurs 7–10 years earlier in men compared with women. | |||
* ACS occurs far more often in men than in women below the age of 60 years but women represent the majority of patients over 75 years of age. | |||
* The risk of acute coronary events in life is related to the exposure to traditional cardiovascular risk factors. | |||
* Huge differences within European and world regions can be found in the incidence and prevalence of IHD and ACS as well as in case fatality rates.<ref>Davies MJ. The pathophysiology of acute coronary syndromes. Heart. 2000 Mar 1;83(3):361-6.Available from: https://oxfordmedicine.com/view/10.1093/med/9780198784906.001.0001/med-9780198784906-chapter-305<nowiki/>Accessed 26.5.2021</ref>.<br> | |||
== Aetiology == | == Aetiology == | ||
[[File:Coronary Artery Disease.png|right|frameless]] | |||
The most common cause by far is [[Atherosclerosis|atherosclerotic plaque]] rupture in coronary artery disease. Other less common causes include: | |||
# Aortic or coronary artery dissection | |||
# Vasculitis | |||
# [[Connective Tissue Disorders|Connective tissue disorders]] | |||
# Drugs: [[Prescription Drug Abuse (Narcotic Painkillers)|cocaine]] | |||
# Coronary artery spasm<ref name=":0" /><br> | |||
== | == Evaluation == | ||
[[File:Normal ecg one wavelength.png|right|frameless]] | |||
The first step of evaluation: [[Electrocardiogram|ECG]], helps differentiate between STEMI and NSTEMI unstable angina. American Heart Association guidelines maintain that any patient with complaints suspicious of ACS should get an ECG within 10 minutes of arrival. | |||
* Cath lab should be activated as soon as STEMI is confirmed in a percutaneous coronary intervention (PCI) center. | |||
* Cardiac enzymes especially troponin, CK-MB/CK ratio is important in assessing the NSTEMI versus myocardial ischemia without tissue destruction. | |||
* A [[Chest X-Rays|chest x-ray]] is useful in diagnosing causes other than [[Myocardial Infarction|MI]] presenting with chest pain like [[pneumonia]] and [[pneumothorax]]. The same applies for [[blood]] work like [[Blood Tests|complete blood count]] (CBC), chemistry, liver function test, and lipase which can help differentiate intraabdominal pathology presenting with chest pain.<ref name=":1" /> | |||
* | |||
* | |||
* | |||
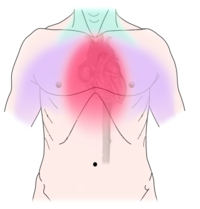
== Clinical Manifestations == | == Clinical Manifestations == | ||
[[File:Angina pectoris.png|right|frameless|209x209px]] | |||
See elaboration in these 3 links | |||
# [[Angina]] | |||
# [[Myocardial Infarction]] | |||
# [[Coronary Artery Disease (CAD)|Coronary Artery Disease]] | |||
== Management == | |||
[[File:Hospital.jpeg|right|frameless]] | |||
See also 3 links above | |||
''' | '''Reperfusion therapy''' | ||
*Diagnosis of STEMI requires emergent reperfusion therapy to restore normal blood flow through coronary arteries and limit infarct size. | |||
*PCI is associated with reduced mortality of approx. 30% and decreased risk of intracranial haemorrhage and [[stroke]] which makes it the best choice for elderly and those at risk for bleeding. | |||
*In optimal circumstances, the usage of PCI is able to achieve restored coronary artery flow in >90% of subjects. Fibrinolytic's restores normal coronary artery flow in 50–60% of subjects.<ref name="ART4">Davies, M.J., 2000. The pathophysiology of acute coronary syndromes. Heart (British Cardiac Society), 83, pp.361–366.</ref> | |||
'' | '''Oxygen''' | ||
*Supplemental [[Oxygen Therapy|oxygen]] should be given to patients with signs of [[Dyspnoea/Dyspnea|breathlessness]], heart failure, shock, or an arterial oxyhemoglobin saturation <94%.<ref name="ART4" /> | |||
'' | '''Nitroglycerin''' | ||
*Nitroglycerin has beneficial effects during suspected cases of ACS. It dilates the coronary arteries, peripheral arterial bed, and venous capacitance vessels. | |||
*The administration of nitroglycerin should be carefully considered in cases when administration would exclude the use of other helpful medications. | |||
*Patients with ischemic discomfort receive up to 3 doses (0.4 mg) over 3–5 min intervals, until chest discomfort is relieved or low blood pressure limits its use. | |||
*Nitroglycerin may be administered intravenously, orally, or topically. Clinicians should be cautious in cases of known inferior wall STEMI and suspected right ventricular involvement because patients require adequate right ventricle preload. A right-sided ECG should be performed to rule out right ventricular ischemia.<ref name="ART4" /> | |||
'''Anti-Platelet therapy''' | |||
*This is common management provided by other healthcare professionals. | |||
*This generally involves the utilisation of medications, predominately in tablet form. These drugs can be aspirin, adenosine diphosphate ADP)-receptor blockers and glycoprotein IIb/IIIa inhibitors, among others.<ref name="ART2" /> | |||
'''[[Beta-Blockers|Beta blockers]]''' | |||
*β-Adrenergic receptor blockers have shown to reduce mortality and decrease infarct size with early intravenous usage and can prevent arrhythmias. | |||
*β-Blockers reduce myocardial workload and oxygen demand by reducing contractility, heart rate, and arterial blood pressure.<ref name="ART4" /> | |||
''' | '''Anticoagulation''' | ||
*Anticoagulant medications such as unfractionated heparin (UFH), low-molecular-weight heparin (LMWH), or less commonly bivalirudin have been shown to decrease reinfarction following reperfusion therapy.<ref name="ART4" /> | |||
== Prevention | == Prevention and Lifestyle modification == | ||
[[File:Treadmill walk.jpg|right|frameless]] | |||
Acute coronary syndrome can best be prevented by better controlling modifiable risk factors such as; diet, exercise, management of [[hypertension]] and [[diabetes]] and [[Smoking Cessation and Brief Intervention|smoking cessation.]] In accordance with the NICE guidelines, clinicians should advise people to eat a Mediterranean-style diet, be [[Physical Activity|physically active]] for 20-30 minutes a day to the point of slight breathlessness, and provide assistance of smoking cessation interventions. Policy changes have taken effect in Scotland which showed a significant decrease the number of admissions for Acute Coronary Syndrome as a result of the The Smoking, Health and Social Care Act which prohibited smoking in all enclosed public places and workplaces. [[Cardiac Rehabilitation|Cardiac rehabilitation]] and education can improve mortality outcomes. | |||
== Physiotherapy == | |||
See links: | |||
[[Cardiac Rehabilitation]] | |||
[[Myocardial Infarction]] | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Glasgow_Caledonian_University_Project]] | |||
[[Category: | [[Category:Cardiopulmonary]] | ||
[[Category:Cardiovascular Disease]] | |||
[[Category:Cardiovascular Disease - Conditions]] | |||
Latest revision as of 14:35, 19 April 2022
Original Editor - Haseel Bhatt
Top Contributors - Haseel Bhatt, Kim Jackson, Lucinda hampton, Adam Vallely Farrell, Admin, Michelle Lee, 127.0.0.1 and WikiSysop
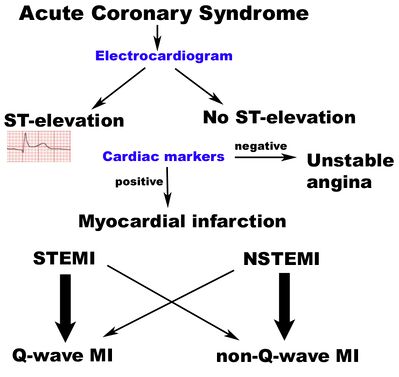
Definition/Description[edit | edit source]
Acute coronary syndrome (ACS) is a group of cardiac diagnoses along a spectrum of severity due to the interruption of coronary blood flow to the myocardium, which in decreasing severity are:
- ST elevation myocardial infarction (STEMI): Very serious type of heart attack during which one of the heart’s major arteries is blocked. The classic heart attack.
- Non-ST elevation myocardial infarction (NSTEMI): The "intermediate" form of ACS, a blockage either occurs in a minor coronary artery or causes partial obstruction of a major coronary artery. Symptoms can be the same as STEMI but the heart damage is far less extensive[1].
- Unstable angina: Thrombus partially or intermittently occludes the coronary artery.
Stable angina is not considered an ACS.[2][3]
ACS is a type of coronary artery disease (CAD), which is responsible for one-third of total deaths in people older than 35. Some forms of CAD can be asymptomatic, but ACS is always symptomatic.[4]
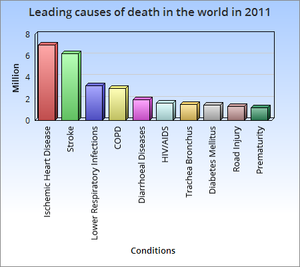
Epidemiology[edit | edit source]
Of all patients who present to emergency departments with symptoms of ACS, only 20-25% will have ACS confirmed as their discharge diagnosis.[2]
- Acute coronary syndromes (ACS) and sudden death cause most ischaemic heart disease(IHD)-related deaths, which represent 1.8 million deaths per year.
- The incidence of IHD in general, and of ACS, increases with age although, on average, this occurs 7–10 years earlier in men compared with women.
- ACS occurs far more often in men than in women below the age of 60 years but women represent the majority of patients over 75 years of age.
- The risk of acute coronary events in life is related to the exposure to traditional cardiovascular risk factors.
- Huge differences within European and world regions can be found in the incidence and prevalence of IHD and ACS as well as in case fatality rates.[5].
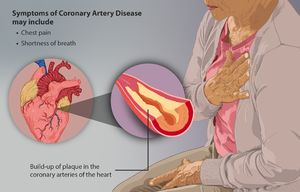
Aetiology[edit | edit source]
The most common cause by far is atherosclerotic plaque rupture in coronary artery disease. Other less common causes include:
- Aortic or coronary artery dissection
- Vasculitis
- Connective tissue disorders
- Drugs: cocaine
- Coronary artery spasm[2]
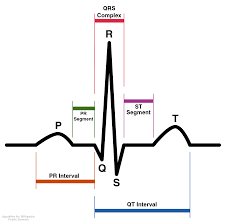
Evaluation[edit | edit source]
The first step of evaluation: ECG, helps differentiate between STEMI and NSTEMI unstable angina. American Heart Association guidelines maintain that any patient with complaints suspicious of ACS should get an ECG within 10 minutes of arrival.
- Cath lab should be activated as soon as STEMI is confirmed in a percutaneous coronary intervention (PCI) center.
- Cardiac enzymes especially troponin, CK-MB/CK ratio is important in assessing the NSTEMI versus myocardial ischemia without tissue destruction.
- A chest x-ray is useful in diagnosing causes other than MI presenting with chest pain like pneumonia and pneumothorax. The same applies for blood work like complete blood count (CBC), chemistry, liver function test, and lipase which can help differentiate intraabdominal pathology presenting with chest pain.[4]
Clinical Manifestations[edit | edit source]
See elaboration in these 3 links
Management[edit | edit source]
See also 3 links above
Reperfusion therapy
- Diagnosis of STEMI requires emergent reperfusion therapy to restore normal blood flow through coronary arteries and limit infarct size.
- PCI is associated with reduced mortality of approx. 30% and decreased risk of intracranial haemorrhage and stroke which makes it the best choice for elderly and those at risk for bleeding.
- In optimal circumstances, the usage of PCI is able to achieve restored coronary artery flow in >90% of subjects. Fibrinolytic's restores normal coronary artery flow in 50–60% of subjects.[6]
Oxygen
- Supplemental oxygen should be given to patients with signs of breathlessness, heart failure, shock, or an arterial oxyhemoglobin saturation <94%.[6]
Nitroglycerin
- Nitroglycerin has beneficial effects during suspected cases of ACS. It dilates the coronary arteries, peripheral arterial bed, and venous capacitance vessels.
- The administration of nitroglycerin should be carefully considered in cases when administration would exclude the use of other helpful medications.
- Patients with ischemic discomfort receive up to 3 doses (0.4 mg) over 3–5 min intervals, until chest discomfort is relieved or low blood pressure limits its use.
- Nitroglycerin may be administered intravenously, orally, or topically. Clinicians should be cautious in cases of known inferior wall STEMI and suspected right ventricular involvement because patients require adequate right ventricle preload. A right-sided ECG should be performed to rule out right ventricular ischemia.[6]
Anti-Platelet therapy
- This is common management provided by other healthcare professionals.
- This generally involves the utilisation of medications, predominately in tablet form. These drugs can be aspirin, adenosine diphosphate ADP)-receptor blockers and glycoprotein IIb/IIIa inhibitors, among others.[3]
- β-Adrenergic receptor blockers have shown to reduce mortality and decrease infarct size with early intravenous usage and can prevent arrhythmias.
- β-Blockers reduce myocardial workload and oxygen demand by reducing contractility, heart rate, and arterial blood pressure.[6]
Anticoagulation
- Anticoagulant medications such as unfractionated heparin (UFH), low-molecular-weight heparin (LMWH), or less commonly bivalirudin have been shown to decrease reinfarction following reperfusion therapy.[6]
Prevention and Lifestyle modification[edit | edit source]
Acute coronary syndrome can best be prevented by better controlling modifiable risk factors such as; diet, exercise, management of hypertension and diabetes and smoking cessation. In accordance with the NICE guidelines, clinicians should advise people to eat a Mediterranean-style diet, be physically active for 20-30 minutes a day to the point of slight breathlessness, and provide assistance of smoking cessation interventions. Policy changes have taken effect in Scotland which showed a significant decrease the number of admissions for Acute Coronary Syndrome as a result of the The Smoking, Health and Social Care Act which prohibited smoking in all enclosed public places and workplaces. Cardiac rehabilitation and education can improve mortality outcomes.
Physiotherapy[edit | edit source]
See links:
References[edit | edit source]
- ↑ Very Well Health Non-ST Segment Myocardial Infarction Overview Available from:https://www.verywellhealth.com/non-st-segment-elevation-myocardial-infarction-nstemi-1746017 (accessed 26.5.2021)
- ↑ 2.0 2.1 2.2 Radiopedia ACS Available: https://radiopaedia.org/articles/acute-coronary-syndrome(accessed 26.5.2021)
- ↑ 3.0 3.1 Aragam, K.G. & Bhatt, D.L., 2011. Antiplatelet therapy in acute coronary syndromes. Journal of cardiovascular pharmacology and therapeutics, 16(1), pp.24–42
- ↑ 4.0 4.1 Singh A, Museedi AS, Grossman SA. Acute coronary syndrome.Available from: https://www.ncbi.nlm.nih.gov/books/NBK459157/(accessed 26.5.20210
- ↑ Davies MJ. The pathophysiology of acute coronary syndromes. Heart. 2000 Mar 1;83(3):361-6.Available from: https://oxfordmedicine.com/view/10.1093/med/9780198784906.001.0001/med-9780198784906-chapter-305Accessed 26.5.2021
- ↑ 6.0 6.1 6.2 6.3 6.4 Davies, M.J., 2000. The pathophysiology of acute coronary syndromes. Heart (British Cardiac Society), 83, pp.361–366.