Achilles Tendinopathy Toolkit: Section F - Medical and Surgical Interventions: Difference between revisions
Kim Jackson (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| Line 10: | Line 10: | ||
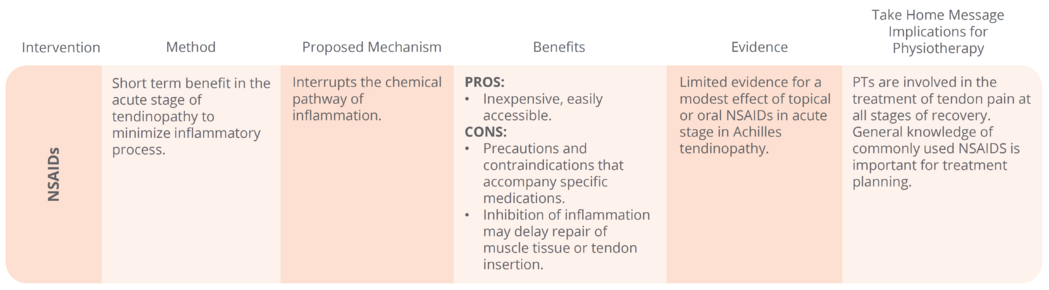
* [[NSAIDs|Non-steroidal anti-inflammatory drugs (NSAIDs)]] - these have antipyretic, anti-inflammatory and analgesic properties. In Achilles tendinopathy these are used in the acute stages to minimise the inflammatory process by interrupting the chemical pathway of inflammation.<ref>McLauchlan , G, Handoll, H. Interventions for treating acute and chronic Achilles tendinitis. Cochrane Collaboration of Systemic Reviews. 2009;2:1‐36.</ref><ref>Karlsson, J., Brorsson, A., & Silbernagel, K. (2014). Treatment of Chronic Achilles Tendinopathies. In G. Bentley (Ed.), European Instructional Lectures (Vol. 14, pp. 191-200): Springer Berlin Heidelberg.</ref> | * [[NSAIDs|Non-steroidal anti-inflammatory drugs (NSAIDs)]] - these have antipyretic, anti-inflammatory and analgesic properties. In Achilles tendinopathy these are used in the acute stages to minimise the inflammatory process by interrupting the chemical pathway of inflammation.<ref>McLauchlan , G, Handoll, H. Interventions for treating acute and chronic Achilles tendinitis. Cochrane Collaboration of Systemic Reviews. 2009;2:1‐36.</ref><ref>Karlsson, J., Brorsson, A., & Silbernagel, K. (2014). Treatment of Chronic Achilles Tendinopathies. In G. Bentley (Ed.), European Instructional Lectures (Vol. 14, pp. 191-200): Springer Berlin Heidelberg.</ref> | ||
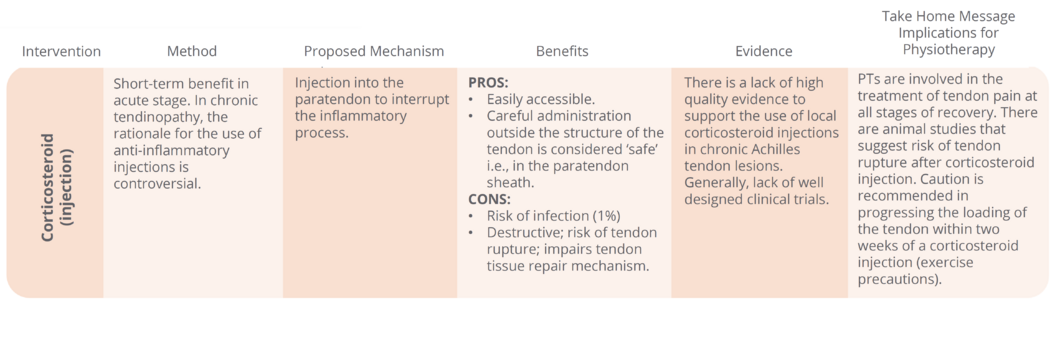
* [[Therapeutic Corticosteroid Injection|Corticosteroid (injection)]] - often prescribed to help relieve pain and inflammation in a localised area of the body. It involves an injection into the paratendon to interrupt the inflammatory process.<ref>DaCuz D, Geeson M, Allen M, Phair I. Achilles paratendonitis: an evaluation of steroid injection. Br J Sports Med. 1988;22(2):64‐65.</ref><ref>Shrier I, Matheson G, Kohl G. Achilles tendinitis: are corticosteroid injections useful or harmful? Clin J Sports Med. 1996;6(4):245‐250.</ref><ref>Fredberg U. Local corticosteroid injection in sport: a review of literature and guidelines for treatment. Scand J Med Sci Sports. 1997;7(3):131‐139.</ref><ref>Speed C. Corticosteroid injections in tendon lesions. Br Med J. 2001;323:382‐386.</ref> | [[File:Achilles Tendinopathy NSAIDS table.png|center|frameless|1049x1049px]] | ||
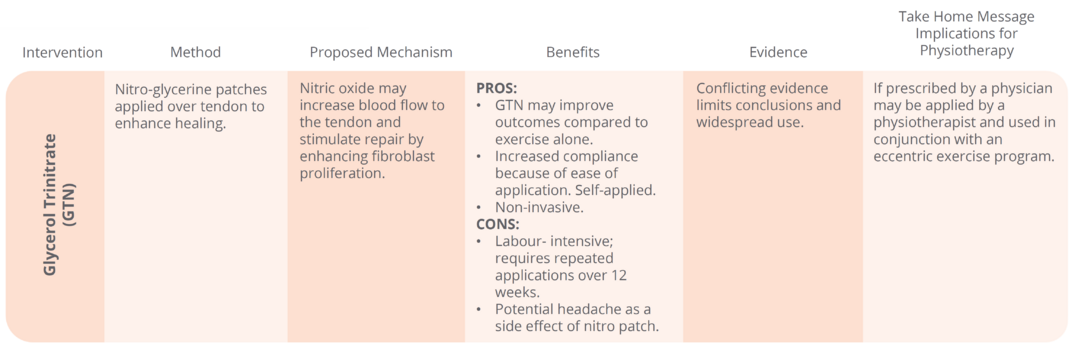
* [[Tendinopathy Treatment Adjuncts#Glyceryl Trinitrate .28GTN.29|Glycerol Trinitrate (GTN)]] - the theory behind the use of GTN is that nitric oxide may increase blood flow to the tendon and stimulate repair by enhancing fibroblast proliferation.<ref>Paoloni J, Appleyard R, Nelson J, Murrell G. Topical GTN treatment of chronic non‐insertional Achilles tendinopathy. A randomized, double‐blind, placebo‐controlled trial. Journal of Bone and Joint Surgery ‐ America. 2004;86‐A(5):916‐922.</ref><ref>Hunter G, Lloyd‐Smith R. Topical GTN for chronic Achilles tendinopathy. Clin J Sports Med. 2005;15(2):116‐117.</ref><ref>Paolini J, Murrell G. Three year follow‐up study of topical GTN treatment of chronic non‐insertional Achilles tendinopathy. Foot and Ankle International. 2007;28(10):1064‐1068.</ref><ref>Gambit E, Gonzalez‐Suarez C, Oquinena T, Agbyani R. Evidence on the effectiveness of topical nitroglycerin in the treatment of tendinopathies: a systemic review and meta‐analysis. Arch Phys Med Rehabil. 2010;91(8):1291‐1305.</ref><ref>Kane, T. P., Ismail, M., & Calder, J. D. (2008). Topical glyceryl trinitrate and noninsertional Achilles tendinopathy: a clinical and cellular investigation. Am J Sports Med, 36(6), 1160-1163. doi: 10.1177/0363546508314423</ref> | *[[Therapeutic Corticosteroid Injection|Corticosteroid (injection)]] - often prescribed to help relieve pain and inflammation in a localised area of the body. It involves an injection into the paratendon to interrupt the inflammatory process.<ref>DaCuz D, Geeson M, Allen M, Phair I. Achilles paratendonitis: an evaluation of steroid injection. Br J Sports Med. 1988;22(2):64‐65.</ref><ref>Shrier I, Matheson G, Kohl G. Achilles tendinitis: are corticosteroid injections useful or harmful? Clin J Sports Med. 1996;6(4):245‐250.</ref><ref>Fredberg U. Local corticosteroid injection in sport: a review of literature and guidelines for treatment. Scand J Med Sci Sports. 1997;7(3):131‐139.</ref><ref>Speed C. Corticosteroid injections in tendon lesions. Br Med J. 2001;323:382‐386.</ref> | ||
[[File:Achilles Tendinopathy Corticosteroid table.png|center|frameless|1055x1055px]] | |||
*[[Tendinopathy Treatment Adjuncts#Glyceryl Trinitrate .28GTN.29|Glycerol Trinitrate (GTN)]] - the theory behind the use of GTN is that nitric oxide may increase blood flow to the tendon and stimulate repair by enhancing fibroblast proliferation.<ref>Paoloni J, Appleyard R, Nelson J, Murrell G. Topical GTN treatment of chronic non‐insertional Achilles tendinopathy. A randomized, double‐blind, placebo‐controlled trial. Journal of Bone and Joint Surgery ‐ America. 2004;86‐A(5):916‐922.</ref><ref>Hunter G, Lloyd‐Smith R. Topical GTN for chronic Achilles tendinopathy. Clin J Sports Med. 2005;15(2):116‐117.</ref><ref>Paolini J, Murrell G. Three year follow‐up study of topical GTN treatment of chronic non‐insertional Achilles tendinopathy. Foot and Ankle International. 2007;28(10):1064‐1068.</ref><ref>Gambit E, Gonzalez‐Suarez C, Oquinena T, Agbyani R. Evidence on the effectiveness of topical nitroglycerin in the treatment of tendinopathies: a systemic review and meta‐analysis. Arch Phys Med Rehabil. 2010;91(8):1291‐1305.</ref><ref>Kane, T. P., Ismail, M., & Calder, J. D. (2008). Topical glyceryl trinitrate and noninsertional Achilles tendinopathy: a clinical and cellular investigation. Am J Sports Med, 36(6), 1160-1163. doi: 10.1177/0363546508314423</ref> | |||
[[File:Achilles Tendinopathy GTN table.png|center|frameless|1075x1075px]] | |||
| | |||
| | |||
== Injection Therapies == | == Injection Therapies == | ||
| Line 117: | Line 20: | ||
Chronic Achilles tendinopathy is associated with abnormal proliferation of neovessels in the ventral portion of the tendon, and along with accompanying neural tissue, is associated with pain in tendinopathy. The presence of neovessels can be visualized by use of ultrasound (US) (sonography). Grey‐scale US is a reliable method to assess tendon structure. Color Doppler or power Doppler has also been used to visualize blood flow. | Chronic Achilles tendinopathy is associated with abnormal proliferation of neovessels in the ventral portion of the tendon, and along with accompanying neural tissue, is associated with pain in tendinopathy. The presence of neovessels can be visualized by use of ultrasound (US) (sonography). Grey‐scale US is a reliable method to assess tendon structure. Color Doppler or power Doppler has also been used to visualize blood flow. | ||
Conservative treatment for Achilles tendinopathy is unsuccessful in 24‐45% of cases. US‐guided injections are becoming increasingly considered as part of ‘best practice’ for treatment of tendinopathies that have failed to respond to other conservative treatment. | Conservative treatment for Achilles tendinopathy is unsuccessful in 24‐45% of cases. US‐guided injections are becoming increasingly considered as part of ‘best practice’ for treatment of tendinopathies that have failed to respond to other conservative treatment. Injection therapy options include: | ||
|- | * [[Achilles Tendinopathy#Medical Management|Polidocanol]] - This is a vascular sclerosant that was originally developed as an anaesthetic and is often used in the treatment of varicose veins. It is used to disrupt neovessels and accompanying nerve structures associated with chronic tendinopathy. <ref>Ohberg L, Alfredson H. US‐guided sclerosis of neovessels in painful chronic Achilles tendinosis: pilot study of new treatment (original article). Br Med Association. 2001;p 1‐7.</ref><ref>Alfredson H, Ohberg L. Sclerosing injections to areas of neovascularization reduces pain in chronic Achilles tendinopathy: a double‐blinded randomized trial. Knee Surgery, Sports Traumatology, Arthroscopy. 2005;13:338‐344.</ref><ref>Alfredson H, Ohberg L, Zeisig E, Lorentzan R. Treatment of mid‐portion Achilles tendinosis: similar clinical results with US and CD‐guided surgery outside the tendon and sclerosing polidocanol injections. Knee Surgery, Sports Traumatology, Arthroscopy. 2007;15:1504‐1509.</ref><ref>Willberg L, Sunding K, Ohberg L, Forssblad M, Fahlstrom M, Alfredson H. Sclerosing injections to treat mid‐portion Achilles tendinosis: a randomized controlled study evaluating two different concentrations of polidocanol. Knee Surgery, Sports Traumatology, Arthroscopy. 2008;16:859‐864.</ref><ref>Wijesekera N, Chew N, Lee J, Mitchell A, et al. US‐guided treatment for chronic Achilles tendinopathy: an update and current status. Skeletal Radiology. 2010;39:425‐434.</ref><ref>van Sterkenburg M, Jonge M. Less promising results with sclerosing ethoxysclerol (polidocanol) injections for mid‐portion Achilles tendinopathy. Am J Sports Med. 2010;38(11):2226‐2232.</ref> | ||
[Insert Table from Toolkit] | |||
* Prolotherapy - This involves injecting an irritant solution, such as hypersomolar dextrose, into multiple sites around the tendon insertion. This stimulates a pro-inflammatory proliferative cell response to increase tissue healing and reduce pain.<ref>Ryan M, Wong A, Taunton J. Favorable outcomes after US‐guided intertendinous injection of hyerosmolar dextrose for chronic insertional and mid‐portion Achilles tendinitis. (Original research). Am J Roengentoloty. 2010;194:1047‐1053.</ref><ref name="Wijesekera 2010">Wijesekera N, Chew N, Lee J, Mitchell A, et al. US‐guided treatment for chronic Achilles tendinopathy: an update and current status. Skeletal Radiology. 2010;39:425‐434.</ref><ref>Yelland, M. J., Sweeting, K. R., Lyftogt, J. A., Ng, S. K., Scuffham, P. A., & Evans, K. A. (2011). Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: a randomised trial. Br J Sports Med, 45(5), 421-428. doi: 10.1136/bjsm.2009.057968</ref> | |||
[Insert Table from Toolkit] | |||
* [[Platelet-Rich Plasma (PRP) Therapy|Platelet Rich Plasma (PRP)]] and Autologous Whole Blood - This is known as regenerative medicine and involves reinjection, into the tendon, of the patient's own whole blood (autologous) or centrifugation of the blood to collect a concentrate of the platelets and plasma. The procedure promotes healing in areas of tendon degeneratiion.<ref name="Wijesekera 2010" /><ref>De Vos R, Weir A, et al. PRP injection for chronic Achilles tendinopathy. Journal of the American Medical Association. 2010;303(3):144‐149.</ref><ref>Engebretsen L, Steffen K, et al. IOC consensus paper on use of PRP in sports medicine. British Journal of Sports Medicine. 2010;44(15):1072‐1081.</ref><ref>De Jonge S, de Vos R, Weir A, et al. 1‐year follow‐up of PRP treatment in chronic Achilles tendinopathy: a double‐blind random placebo‐controlled trial. American Journal of Sports Medicine. 2011;39(8):1623‐1629.</ref><ref>Bell, K. J., Fulcher, M. L., Rowlands, D. S., & Kerse, N. (2013). Impact of autologous blood injections in treatment of mid-portion Achilles tendinopathy: double blind randomised controlled trial (Vol. 346).</ref> | |||
| | |||
[Insert Table from Toolkit] | |||
* High Volume Injection (HVI) or Hydrostatic Dissection - In this procedure a small volume of anaesthetic/steroid and high volume saline is delivered by ultrasound guided imaging. The pressure created by the volume of substance into the tendon sheath thought to disrupt the neovessel ingrowth, resetting the healing process and reducing pain.<ref>Chan O, O’Dowd D, Padhiar N, et al. High volume image guided injections in chronic Achilles tendinopathy. Disability and Rehabilitation. 2008;30:1697‐1708.</ref><ref>Maffulli, N., Spiezia, F., Longo, U. G., Denaro, V., & Maffulli, G. D. (2013). High volume image guided injections for the management of chronic tendinopathy of the main body of the Achilles tendon. Physical Therapy in Sport, 14(3), 163-167. doi: http://dx.doi.org/10.1016/j.ptsp.2012.07.002</ref><ref>Boesen, A., Boesen, M., Hansen, R., Malliaras, P., Chan, O., & Langberg, H. (2014). 61 High Volume Injection, Platelet Rich Plasma And Placebo In Chronic Achilles Tendinopathy–A Double Blind Prospective Study. British Journal of Sports Medicine, 48(Suppl 2), A39-A40.</ref> | |||
[Insert Table from Toolkit] | |||
== Dry Needling == | |||
| | [[Dry needling|Dry Needling]] involves using a fine hypodermic needle or acupuncture needle that does not involve the injection of a substance. The technique is sometimes referred to as "tendon fenestration"<ref>Housner J, Jacobsen J, Misko R. Sonographically guided percutaneous needle tenotomy for treatment of chronic tendinosis. Journal of Ultrasound Medicine. 2009;28(8):1187‐1192.</ref> The needle is inserted into the tendon a number of times which creates an haemorrhagic response. This is followed by an inflammatory response, granulation and healing. | ||
[Insert table]Surgical Approaches | |||
Surgical success rates are reported at 85% for Achilles tendinopathy that have failed to respond to conservative measures. | Surgical success rates are reported at 85% for Achilles tendinopathy that have failed to respond to conservative measures. | ||
=== | == Surgical Approaches == | ||
Surgical success rates are reported at 8% for Achilles tendinopathy that have failed to respond to conservative measures. | |||
* Percutaneous tenotomy - This technique involves a closed dissection of the tendon sheath by ultrasound guided percutaneous longitudinal internal tenotomy or an open surgical exposure of the tendon. <ref>Testa V, Capasso G, Benazzo F, Muffulli N. Management of Achilles tendinopathy by US‐guided percutaneous tenotomy. Medicine and Science in Sports and Exercise. 2002;34(4):573‐580.</ref><ref>Maffulli, N., Oliva, F., Testa, V., Capasso, G., & Del Buono, A. (2013). Multiple Percutaneous Longitudinal Tenotomies for Chronic Achilles Tendinopathy in Runners A Long-Term Study. The American journal of sports medicine, 41(9), 2151-2157.</ref> | |||
[Insert Table from Toolkit] | |||
* Surgical debridement - A central longitudinal incision is made to expose the tendon. The disorganised and fibrotic tendon tissue and adhesions is then excised with the application diathermy to destroy neovessels. The surgery creates granulation and repair, and removes the fibrotic tissue.<ref>Tallon C, Coleman B, Khan K, Maffulli N. Outcomes of surgery of chronic Achilles tendinopathy. Am J Sports Med. 2001;29(3):315‐320.</ref><ref>Maffulli, N., Del Buono, A., Testa, V., Capasso, G., Oliva, F., & Denaro, V. (2011). Safety and outcome of surgical debridement of insertional Achilles tendinopathy using a transverse (Cincinnati) incision. Journal of Bone & Joint Surgery, British Volume, 93(11), 1503-1507.</ref> | |||
[Insert Table from Toolkit] | |||
* Minimally invasive stripping - A small incision is made allowing a probe or scalpel to be inserted ventral to the tendon. The area of neovascularisation is stripped. This disrupts the abnormal blood/nerve supply, releases adhesions. <ref>Longo UG, Ramamurthy C, Denaro V, Maffulli N. Minimally invasive stripping for chronic Achilles tendinopathy. Disabil Rehabil. 2008;30(20‐22):1709‐13.</ref> | |||
== Resources == | |||
* Click to go back to the [[Achilles Tendinopathy Toolkit|Main Achilles Tendinopathy Toolkit page]] | * Click to go back to the [[Achilles Tendinopathy Toolkit|Main Achilles Tendinopathy Toolkit page]] | ||
* Click to go back to [[Achilles Tendinopathy Toolkit: Section A - Clinical Evaluation|Section A - Clinical Evaluation]] | * Click to go back to [[Achilles Tendinopathy Toolkit: Section A - Clinical Evaluation|Section A - Clinical Evaluation]] | ||
| Line 389: | Line 65: | ||
* Click to go back to [[Achilles Tendinopathy Toolkit: Section D - Exercise Programs|Section D - Exercise Programs]] | * Click to go back to [[Achilles Tendinopathy Toolkit: Section D - Exercise Programs|Section D - Exercise Programs]] | ||
* Click to go back to [[Achilles Tendinopathy Toolkit: Section E - Low Level Laser Therapy Dosage Calculation|Section E - Low Level Laser Therapy Dosage Calculation]] | * Click to go back to [[Achilles Tendinopathy Toolkit: Section E - Low Level Laser Therapy Dosage Calculation|Section E - Low Level Laser Therapy Dosage Calculation]] | ||
* [https://med-fom-clone-pt.sites.olt.ubc.ca/files/2021/10/ATT-Final-Version-Oct-19th-21.pdf#page=16&zoom=100,0,0 UBC Achilles Tendinopathy Toolkit] | |||
== | |||
= References = | = References = | ||
Revision as of 15:36, 22 July 2022
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (22/07/2022)
Introduction[edit | edit source]
The purpose of this document is to summarize common medical and surgical interventions which may be considered for the management of Achilles tendinopathy – particularly if it is not responding adequately to recommended conservative management strategies (see “Achilles Tendinopathy: Summary of the Evidence for Physical Therapy Interventions”).
Pharmacological Approaches[edit | edit source]
There is limited evidence, and in some cases no evidence, to support the use of pharmacological interventions in the treatment of achilles tendinopathy. The 3 most commonly used pharmacological approaches are:
- Non-steroidal anti-inflammatory drugs (NSAIDs) - these have antipyretic, anti-inflammatory and analgesic properties. In Achilles tendinopathy these are used in the acute stages to minimise the inflammatory process by interrupting the chemical pathway of inflammation.[1][2]
- Corticosteroid (injection) - often prescribed to help relieve pain and inflammation in a localised area of the body. It involves an injection into the paratendon to interrupt the inflammatory process.[3][4][5][6]
- Glycerol Trinitrate (GTN) - the theory behind the use of GTN is that nitric oxide may increase blood flow to the tendon and stimulate repair by enhancing fibroblast proliferation.[7][8][9][10][11]
Injection Therapies[edit | edit source]
Chronic Achilles tendinopathy is associated with abnormal proliferation of neovessels in the ventral portion of the tendon, and along with accompanying neural tissue, is associated with pain in tendinopathy. The presence of neovessels can be visualized by use of ultrasound (US) (sonography). Grey‐scale US is a reliable method to assess tendon structure. Color Doppler or power Doppler has also been used to visualize blood flow.
Conservative treatment for Achilles tendinopathy is unsuccessful in 24‐45% of cases. US‐guided injections are becoming increasingly considered as part of ‘best practice’ for treatment of tendinopathies that have failed to respond to other conservative treatment. Injection therapy options include:
- Polidocanol - This is a vascular sclerosant that was originally developed as an anaesthetic and is often used in the treatment of varicose veins. It is used to disrupt neovessels and accompanying nerve structures associated with chronic tendinopathy. [12][13][14][15][16][17]
[Insert Table from Toolkit]
- Prolotherapy - This involves injecting an irritant solution, such as hypersomolar dextrose, into multiple sites around the tendon insertion. This stimulates a pro-inflammatory proliferative cell response to increase tissue healing and reduce pain.[18][19][20]
[Insert Table from Toolkit]
- Platelet Rich Plasma (PRP) and Autologous Whole Blood - This is known as regenerative medicine and involves reinjection, into the tendon, of the patient's own whole blood (autologous) or centrifugation of the blood to collect a concentrate of the platelets and plasma. The procedure promotes healing in areas of tendon degeneratiion.[19][21][22][23][24]
[Insert Table from Toolkit]
- High Volume Injection (HVI) or Hydrostatic Dissection - In this procedure a small volume of anaesthetic/steroid and high volume saline is delivered by ultrasound guided imaging. The pressure created by the volume of substance into the tendon sheath thought to disrupt the neovessel ingrowth, resetting the healing process and reducing pain.[25][26][27]
[Insert Table from Toolkit]
Dry Needling[edit | edit source]
Dry Needling involves using a fine hypodermic needle or acupuncture needle that does not involve the injection of a substance. The technique is sometimes referred to as "tendon fenestration"[28] The needle is inserted into the tendon a number of times which creates an haemorrhagic response. This is followed by an inflammatory response, granulation and healing.
[Insert table]Surgical Approaches
Surgical success rates are reported at 85% for Achilles tendinopathy that have failed to respond to conservative measures.
Surgical Approaches[edit | edit source]
Surgical success rates are reported at 8% for Achilles tendinopathy that have failed to respond to conservative measures.
- Percutaneous tenotomy - This technique involves a closed dissection of the tendon sheath by ultrasound guided percutaneous longitudinal internal tenotomy or an open surgical exposure of the tendon. [29][30]
[Insert Table from Toolkit]
- Surgical debridement - A central longitudinal incision is made to expose the tendon. The disorganised and fibrotic tendon tissue and adhesions is then excised with the application diathermy to destroy neovessels. The surgery creates granulation and repair, and removes the fibrotic tissue.[31][32]
[Insert Table from Toolkit]
- Minimally invasive stripping - A small incision is made allowing a probe or scalpel to be inserted ventral to the tendon. The area of neovascularisation is stripped. This disrupts the abnormal blood/nerve supply, releases adhesions. [33]
Resources[edit | edit source]
- Click to go back to the Main Achilles Tendinopathy Toolkit page
- Click to go back to Section A - Clinical Evaluation
- Click to go back to Section B - Outcome Measures
- Click to go back to Section C - Summary of Evidence and Recommendations for Interventions
- Click to go back to Section D - Exercise Programs
- Click to go back to Section E - Low Level Laser Therapy Dosage Calculation
- UBC Achilles Tendinopathy Toolkit
References[edit | edit source]
- ↑ McLauchlan , G, Handoll, H. Interventions for treating acute and chronic Achilles tendinitis. Cochrane Collaboration of Systemic Reviews. 2009;2:1‐36.
- ↑ Karlsson, J., Brorsson, A., & Silbernagel, K. (2014). Treatment of Chronic Achilles Tendinopathies. In G. Bentley (Ed.), European Instructional Lectures (Vol. 14, pp. 191-200): Springer Berlin Heidelberg.
- ↑ DaCuz D, Geeson M, Allen M, Phair I. Achilles paratendonitis: an evaluation of steroid injection. Br J Sports Med. 1988;22(2):64‐65.
- ↑ Shrier I, Matheson G, Kohl G. Achilles tendinitis: are corticosteroid injections useful or harmful? Clin J Sports Med. 1996;6(4):245‐250.
- ↑ Fredberg U. Local corticosteroid injection in sport: a review of literature and guidelines for treatment. Scand J Med Sci Sports. 1997;7(3):131‐139.
- ↑ Speed C. Corticosteroid injections in tendon lesions. Br Med J. 2001;323:382‐386.
- ↑ Paoloni J, Appleyard R, Nelson J, Murrell G. Topical GTN treatment of chronic non‐insertional Achilles tendinopathy. A randomized, double‐blind, placebo‐controlled trial. Journal of Bone and Joint Surgery ‐ America. 2004;86‐A(5):916‐922.
- ↑ Hunter G, Lloyd‐Smith R. Topical GTN for chronic Achilles tendinopathy. Clin J Sports Med. 2005;15(2):116‐117.
- ↑ Paolini J, Murrell G. Three year follow‐up study of topical GTN treatment of chronic non‐insertional Achilles tendinopathy. Foot and Ankle International. 2007;28(10):1064‐1068.
- ↑ Gambit E, Gonzalez‐Suarez C, Oquinena T, Agbyani R. Evidence on the effectiveness of topical nitroglycerin in the treatment of tendinopathies: a systemic review and meta‐analysis. Arch Phys Med Rehabil. 2010;91(8):1291‐1305.
- ↑ Kane, T. P., Ismail, M., & Calder, J. D. (2008). Topical glyceryl trinitrate and noninsertional Achilles tendinopathy: a clinical and cellular investigation. Am J Sports Med, 36(6), 1160-1163. doi: 10.1177/0363546508314423
- ↑ Ohberg L, Alfredson H. US‐guided sclerosis of neovessels in painful chronic Achilles tendinosis: pilot study of new treatment (original article). Br Med Association. 2001;p 1‐7.
- ↑ Alfredson H, Ohberg L. Sclerosing injections to areas of neovascularization reduces pain in chronic Achilles tendinopathy: a double‐blinded randomized trial. Knee Surgery, Sports Traumatology, Arthroscopy. 2005;13:338‐344.
- ↑ Alfredson H, Ohberg L, Zeisig E, Lorentzan R. Treatment of mid‐portion Achilles tendinosis: similar clinical results with US and CD‐guided surgery outside the tendon and sclerosing polidocanol injections. Knee Surgery, Sports Traumatology, Arthroscopy. 2007;15:1504‐1509.
- ↑ Willberg L, Sunding K, Ohberg L, Forssblad M, Fahlstrom M, Alfredson H. Sclerosing injections to treat mid‐portion Achilles tendinosis: a randomized controlled study evaluating two different concentrations of polidocanol. Knee Surgery, Sports Traumatology, Arthroscopy. 2008;16:859‐864.
- ↑ Wijesekera N, Chew N, Lee J, Mitchell A, et al. US‐guided treatment for chronic Achilles tendinopathy: an update and current status. Skeletal Radiology. 2010;39:425‐434.
- ↑ van Sterkenburg M, Jonge M. Less promising results with sclerosing ethoxysclerol (polidocanol) injections for mid‐portion Achilles tendinopathy. Am J Sports Med. 2010;38(11):2226‐2232.
- ↑ Ryan M, Wong A, Taunton J. Favorable outcomes after US‐guided intertendinous injection of hyerosmolar dextrose for chronic insertional and mid‐portion Achilles tendinitis. (Original research). Am J Roengentoloty. 2010;194:1047‐1053.
- ↑ 19.0 19.1 Wijesekera N, Chew N, Lee J, Mitchell A, et al. US‐guided treatment for chronic Achilles tendinopathy: an update and current status. Skeletal Radiology. 2010;39:425‐434.
- ↑ Yelland, M. J., Sweeting, K. R., Lyftogt, J. A., Ng, S. K., Scuffham, P. A., & Evans, K. A. (2011). Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: a randomised trial. Br J Sports Med, 45(5), 421-428. doi: 10.1136/bjsm.2009.057968
- ↑ De Vos R, Weir A, et al. PRP injection for chronic Achilles tendinopathy. Journal of the American Medical Association. 2010;303(3):144‐149.
- ↑ Engebretsen L, Steffen K, et al. IOC consensus paper on use of PRP in sports medicine. British Journal of Sports Medicine. 2010;44(15):1072‐1081.
- ↑ De Jonge S, de Vos R, Weir A, et al. 1‐year follow‐up of PRP treatment in chronic Achilles tendinopathy: a double‐blind random placebo‐controlled trial. American Journal of Sports Medicine. 2011;39(8):1623‐1629.
- ↑ Bell, K. J., Fulcher, M. L., Rowlands, D. S., & Kerse, N. (2013). Impact of autologous blood injections in treatment of mid-portion Achilles tendinopathy: double blind randomised controlled trial (Vol. 346).
- ↑ Chan O, O’Dowd D, Padhiar N, et al. High volume image guided injections in chronic Achilles tendinopathy. Disability and Rehabilitation. 2008;30:1697‐1708.
- ↑ Maffulli, N., Spiezia, F., Longo, U. G., Denaro, V., & Maffulli, G. D. (2013). High volume image guided injections for the management of chronic tendinopathy of the main body of the Achilles tendon. Physical Therapy in Sport, 14(3), 163-167. doi: http://dx.doi.org/10.1016/j.ptsp.2012.07.002
- ↑ Boesen, A., Boesen, M., Hansen, R., Malliaras, P., Chan, O., & Langberg, H. (2014). 61 High Volume Injection, Platelet Rich Plasma And Placebo In Chronic Achilles Tendinopathy–A Double Blind Prospective Study. British Journal of Sports Medicine, 48(Suppl 2), A39-A40.
- ↑ Housner J, Jacobsen J, Misko R. Sonographically guided percutaneous needle tenotomy for treatment of chronic tendinosis. Journal of Ultrasound Medicine. 2009;28(8):1187‐1192.
- ↑ Testa V, Capasso G, Benazzo F, Muffulli N. Management of Achilles tendinopathy by US‐guided percutaneous tenotomy. Medicine and Science in Sports and Exercise. 2002;34(4):573‐580.
- ↑ Maffulli, N., Oliva, F., Testa, V., Capasso, G., & Del Buono, A. (2013). Multiple Percutaneous Longitudinal Tenotomies for Chronic Achilles Tendinopathy in Runners A Long-Term Study. The American journal of sports medicine, 41(9), 2151-2157.
- ↑ Tallon C, Coleman B, Khan K, Maffulli N. Outcomes of surgery of chronic Achilles tendinopathy. Am J Sports Med. 2001;29(3):315‐320.
- ↑ Maffulli, N., Del Buono, A., Testa, V., Capasso, G., Oliva, F., & Denaro, V. (2011). Safety and outcome of surgical debridement of insertional Achilles tendinopathy using a transverse (Cincinnati) incision. Journal of Bone & Joint Surgery, British Volume, 93(11), 1503-1507.
- ↑ Longo UG, Ramamurthy C, Denaro V, Maffulli N. Minimally invasive stripping for chronic Achilles tendinopathy. Disabil Rehabil. 2008;30(20‐22):1709‐13.
Acknowledgements[edit | edit source]
Developed by Michael Yates, PT. BC Physiotherapy Tendinopathy Task Force. April 2012.
Updated by Alexandra Kobza, Dr. Alex Scott. June 2015.