Dyspareunia
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (11/09/2023)
Definition[edit | edit source]
Dyspareunia is defined as persistent genital pain that occurs during sexual intercourse.[1] It can be classified into two types based on the location of the pain – entry or deep dyspareunia. While entry dyspareunia is associated with pain upon an attempt at vaginal penetration at the introitus, deep dyspareunia is pain perceived upon vaginal penetration and causes include adenomyosis, endometriosis, vaginal scarring, interstitial cystitis, and pelvic adhesions. [2]
Prevalence[edit | edit source]
The prevalence of dyspareunia varies from 8% to 21.1% globally, as reported by the World Health Organization in 2006. [3]
A recent systematic review concluded the prevalence of dyspareunia as 42% at 2 months, 43% at 2–6 months, and 22% at 6–12 months postpartum. Given these high prevalence as well as impact on a woman's life, the study highlighted to give special attention to the dyspareunia during the postpartum period. [4]
Clinically Relevant Anatomy[edit | edit source]
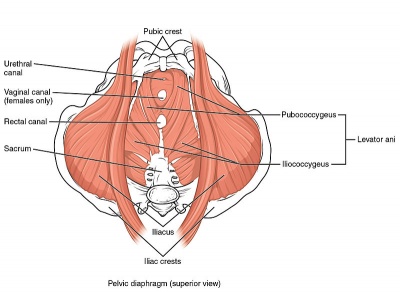
Weakness in deep pelvic floor muscles (levator ani muscle group and coccygeus) can cause deep dyspareunia. [5][6][7]
The pudendal nerve (composed of somatic branches from the sacral plexus, specifically S2 to S4 [8] [9] [10][11]) is one of most important nerves associated with dyspareunia or pelvic pain. Due to its location in the pelvis, it is susceptible to injury during pelvic surgeries and parturition. [8][10]
Entry dyspareunia usually involves the vulva and its surrounding structures [7]
Deep dyspareunia is characterized by pain experienced during deep vaginal penetration and might involve the inner pelvic structures such as the urinary bladder and cervix. [7][6]
Please see the page "Pelvic Floor Anatomy" for further details regarding anatomy.
Aetiology[edit | edit source]
Dyspareunia could be a symptom stemming from one or more of the following:
- skin irritation (i.e. eczema or other skin problems in the genital region)[1]
- endometriosis[12]
- vestibulodynia
- vulvodynia[13]
- vaginismus[12]
- interstitial cystitis[13]
- fibromyalgia[13]
- irritable bowel syndrome[13]
- pelvic inflammatory disease[14]
- depression and/or anxiety[14]
- post-menopause[14]
- postpartum dyspareunia [2]
- inadequate vaginal lubrication or arousal [2]
- anogenital causes such as hemorrhoids and anal fissures [2]
- Bartholin gland infection [2]
- vulvovaginitis [2]
- vaginal atrophy [2]
- adenomyosis [2]
- vaginal scarring [2]
- pelvic adhesions [2]
Clinical Presentation[edit | edit source]
Individuals may present with pain that occurs at entry during penetration, with deep penetration or pain post-penetration. The patient may also describe pain associated with the insertion of a tampon or during a Pap exam. Words used to describe pain may be (but are not limited to): "throbbing" "burning" or "aching." [15]
Diagnostic Procedures[edit | edit source]
History Taking[edit | edit source]
A recent study [2] summarised important findings related to the history taking:
- Accurate clinical diagnosis requires detailed information about the location, onset, duration, severity, nature of pain, precipitating factors, and positions associated with the pain. [7][6]
- It is particularly helpful to know the specific location of the pain, especially if it is localized to the vulva, vagina introitus, or inside of the vagina, as this can help narrow down the possible causes.
- In his article on the clinical approach to dyspareunia, Graziottin provides a comprehensive guide to the necessary questions for a thorough history and physical examination. [16]
Another study [3] listed the important elements to discuss during clinical evaluation of female sexual pain as below:
- Pain characteristics: Timing, duration, quality, location, provoked, or unprovoked
- Musculoskeletal history: Pelvic floor surgery, trauma, obstetrics
- Bowel and bladder history: Constipation, diarrhea, urgency, frequency
- Sexual history: Frequency, desire, arousal, satisfaction, relationship
- Psychological history: Mood disorder, anxiety, depression
- History of abuse: Sexual, physical, neglect.
Physical Examination[edit | edit source]
The gold standard to assess the pelvic floor muscles is through an internal exam, performed by a trained medical professional with the informed consent of the patient. This exam allows for the assessment of the health of the tissue, the tonicity of the pelvic floor muscles, the ability to contract and relax these muscles and to assess for vulvodynia and/or vestibulodynia.
Outcome Measures[edit | edit source]
When quantifying the pain, validated self-report questionnaires such as the Female Sexual Function Index, the McGill Pain Questionnaire, or the Patient Reported Outcomes Measurement Information System (PROMIS) vulvar discomfort scale may be more helpful instead of asking a patient to rate their pain on one to 10. [17]
The Female Sexual Destress Scale-Revised (FSDS-R): A single item from this scale may be a useful tool in quickly screening for sexual distress in middle-aged women.[18]
Management / Interventions[edit | edit source]
Multidisciplinary Approach[edit | edit source]
The use of a multidisciplinary approach with the inclusion of a gynaecologist, urologist, psychiatrist, pain management expert, physical therapist, sexual therapist, and mental health professionals with a specialization in chronic pain is advantageous to address all the aspects of pain (physical, emotional, and behavioural). [19]
The first step towards treating a patient's pain is for the physician to acknowledge that the patient is experiencing it. The physician should counsel the patient that pain management might take time and that it may not completely go away even after treatment. The patient should be informed about all the available treatment options and should be helped in selecting the best possible option. The initial step should be a conservative, nonsurgical approach. Treatment options depend on the aetiology of the patient's complaint and can include: [20]
- Oral tricyclic antidepressants
- Oral or topical hormonal replacement
- Oral NSAIDs, and botox injections: Botulinum toxin injection is effective in treating dyspareunia caused by pelvic floor myalgia and contracture. [21][22]
- Cognitive-behavioural therapy, and other brain-based therapies: Cognitive-behavioral therapy is the most commonly used behavioural intervention and is strongly recommended. It is an effective behavioural intervention in reducing anxiety and fear associated with dyspareunia. [23]
- Systemic and topical hormone replacement therapy, selective estrogen receptor modulator therapy, and the use of vaginal dehydroepiandrosterone: For the patients with dyspareunia due to post-menopausal vaginal atrophy. [24]
- Appropriate antibiotic, antifungal, or antiviral therapy based upon culture results: For dyspareunia due to infectious causes.
- Vaginal lubricants, scar tissue massage: Post-partum dyspareunia can respond to these options.
- Pelvic floor rehabilitation: According to the result of a recent randomised control study [25], pelvic floor rehabilitation is an important part of a multidisciplinary treatment approach to dyspareunia. It can serve as an adjuvant treatment option in most cases of dyspareunia. It relaxes the pelvic floor muscles and re-educates the pain receptors. [26]
- Surgical treatment: Only adopted as a last option when all conservative treatment options have failed. It is usually useful in identifying and/or treating pelvic adhesions, endometriosis, and pelvic organ prolapse. [27]
Physiotherapy Management[edit | edit source]
Physiotherapists can address factors contributing to dyspareunia with the following tools and techniques.
| Contributing factor | Tool/Technique |
|---|---|
| Lack of awareness of pelvic floor muscles | Assess the patient's ability to connect with their pelvic floor muscles through their ability to correctly contract and relax their pelvic floor muscles. If the patient is unable to correctly recruit these muscles, whether it be due to lack of strength or neuromotor connection, this should be addressed. |
| Hypertonic pelvic floor muscles | Teaching relaxation techniques for the pelvic floor muscles:
The use of inserts can be beneficial along with these techniques. Teach the patient to move the dilator or insert past the entrance of the vaginal canal in conjunction with relaxing the pelvic floor muscles. |
| Pain centralization | If this has been a chronic issue, addressing principles of centralized pain and explaining this to the patient can be helpful and informative. Additionally, pain at the entrance or through the vaginal canal can elicit a spasm or hypertonic response by the pelvic floor muscles. |
Additional Considerations[edit | edit source]
- The use of a multidisciplinary approach with the inclusion of a physician and a counselling therapist could be beneficial, depending on the reason for experiencing dyspareunia.
- Issues such as fatigue, depression/anxiety, stress or history of abuse can contribute to the tension of the pelvic floor muscles, and this may be addressed through counselling.
- Ensure that the patient has been screened by a physician to rule out any differential diagnoses or address co-existing diagnoses that are out of the physiotherapy scope of practice.
Resources[edit | edit source]
- To see the recommended measurement tools prepared by the Pelvic Floor Disorders Consortium: "Measuring Pelvic Floor Disorder Symptoms Using Patient-Reported Instruments"
- A webinar by "Jean Hailes for Women’s Health" ( a national not-for-profit organisation) on dyspareunia and the physiotherapist's perspective:
- A presentation was created by Carolyn Vandyken, a physiotherapist who specializes in the treatment of male and female pelvic dysfunction. She also provides education and mentorship to physiotherapists who are similarly interested in treating these dysfunctions. In the presentation, Carolyn reviews pelvic anatomy, the history of Kegel exercises and what the evidence tells us about when Kegels are and aren't appropriate for our patients.
References[edit | edit source]
- ↑ 1.0 1.1 Mayo Clinic. Painful intercourse. Available from:https://www.mayoclinic.org/diseases-conditions/painful-intercourse/symptoms-causes/syc-20375967 (accessed 13 Feb 2019).
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Alimi Y, Iwanaga JO, Oskouian RJ, Loukas M, Tubbs RS. The clinical anatomy of dyspareunia: A review. Clinical Anatomy. 2018 Oct;31(7):1013-7.
- ↑ 3.0 3.1 Sorensen J, Bautista KE, Lamvu G, Feranec J. Evaluation and treatment of female sexual pain: a clinical review. Cureus. 2018 Mar 27;10(3).
- ↑ Banaei M, Kariman N, Ozgoli G, Nasiri M, Ghasemi V, Khiabani A, Dashti S, Mohamadkhani Shahri L. Prevalence of postpartum dyspareunia: a systematic review and meta‐analysis. International Journal of Gynecology & Obstetrics. 2021 Apr;153(1):14-24.
- ↑ Edwards L. Vulvodynia. Clinical obstetrics and gynecology. 2015 Mar 1;58(1):143-52.
- ↑ 6.0 6.1 6.2 Seehusen DA, Baird DC, Bode DV. Dyspareunia in women. American family physician. 2014 Oct 1;90(7):465-70.
- ↑ 7.0 7.1 7.2 7.3 Howard FM, editor. Pelvic pain: diagnosis and management. Lippincott Williams & Wilkins; 2000.
- ↑ 8.0 8.1 Prather H, Dugan S, Fitzgerald C, Hunt D. Review of anatomy, evaluation, and treatment of musculoskeletal pelvic floor pain in women. PM&R. 2009 Apr 1;1(4):346-58.
- ↑ Standring S. Gray’s Anatomy 41st Edition: Churchill Livingstone.
- ↑ 10.0 10.1 Woodman PJ, Graney DO. Anatomy and physiology of the female perineal body with relevance to obstetrical injury and repair. Clinical Anatomy: The Official Journal of the American Association of Clinical Anatomists and the British Association of Clinical Anatomists. 2002 Aug;15(5):321-34.
- ↑ Ventolini G. Vulvar pain: anatomic and recent pathophysiologic considerations. Clinical Anatomy. 2013 Jan;26(1):130-3.
- ↑ 12.0 12.1 The American College of Obstetricians and Gynecologists. When sex is painful. Available from:https://www.acog.org/Patients/FAQs/When-Sex-Is-Painful (accessed 21 Feb 2019).
- ↑ 13.0 13.1 13.2 13.3 Reed BD, Harlow SD, Sen A, Edwards RM, Chen D, Haefner HK. Relationship between vulvodynia and chronic comorbid pain conditions. Obstetrics and gynecology. 2012;120(1):145.
- ↑ 14.0 14.1 14.2 Latthe P, Mignini L, Gray R, et al. Factors predisposing women to chronic pelvic pain: systematic review. BMJ. 2006;332:749. Latthe P, Mignini L, Gray R, Hills R, Khan K. Factors predisposing women to chronic pelvic pain: systematic review. BMJ. 2006;332(7544):749-55.
- ↑ Morris C, Briggs C, Navani M. Dyspareunia. InnovAiT. 2021 Oct;14(10):607-14.
- ↑ Graziottin A. Clinical approach to dyspareunia. Journal of Sex & Marital Therapy. 2001 Oct 1;27(5):489-501.
- ↑ Goldstein AT, Pukall CF, Brown C, Bergeron S, Stein A, Kellogg-Spadt S. Vulvodynia: assessment and treatment. The journal of sexual medicine. 2016 Apr;13(4):572-90.
- ↑ Carpenter JS, Reed SD, Guthrie KA, Larson JC, Newton KM, Lau RJ, Learman LA, Shifren JL. Using an FSDS‐R Item to Screen for Sexually Related Distress: A MsFLASH Analysis. Sexual medicine. 2015 Mar;3(1):7-13.
- ↑ American College of Obstetricians and Gynecologists. Committee Opinion No 673-Persistent vulvar pain. Obstet Gynecol. 2016;128(3):e78-84.
- ↑ Tayyeb M, Gupta V. Dyspareunia.
- ↑ Park AJ, Paraiso MF. Successful use of botulinum toxin type a in the treatment of refractory postoperative dyspareunia. Obstetrics & Gynecology. 2009 Aug 1;114(2 Part 2):484-7.
- ↑ Pelletier F, Girardin M, Humbert P, Puyraveau M, Aubin F, Parratte B. Long‐term assessment of effectiveness and quality of life of OnabotulinumtoxinA injections in provoked vestibulodynia. Journal of the European Academy of Dermatology and Venereology. 2016 Jan;30(1):106-11.
- ↑ Engman M, Wijma K, Wijma B. Long-term coital behaviour in women treated with cognitive behaviour therapy for superficial coital pain and vaginismus. Cognitive behaviour therapy. 2010 Sep 1;39(3):193-202.
- ↑ Naumova I, Castelo-Branco C. Current treatment options for postmenopausal vaginal atrophy. International journal of women's health. 2018 Jul 31:387-95.
- ↑ Ghaderi F, Bastani P, Hajebrahimi S, Jafarabadi MA, Berghmans B. Pelvic floor rehabilitation in the treatment of women with dyspareunia: a randomized controlled clinical trial. International urogynecology journal. 2019 Nov;30:1849-55.
- ↑ Rosenbaum TY. Physiotherapy treatment of sexual pain disorders. Journal of sex & marital therapy. 2005 Jul 1;31(4):329-40.
- ↑ Kliethermes CJ, Shah M, Hoffstetter S, Gavard JA, Steele A. Effect of vestibulectomy for intractable vulvodynia. Journal of Minimally Invasive Gynecology. 2016 Nov 1;23(7):1152-7.
- ↑ Jean Hailes. Webinar: Dyspareunia - The physiotherapist's perspective. Available from: https://www.youtube.com/watch?v=rpIi_1SVTeg
- ↑ Physiopedia. Pelvic Physiotherapy - to Kegel or Not?. Available from: https://www.youtube.com/watch?v=w08iCzxnQBU