Osteogenesis Imperfecta
Genetic_DisordersOriginal Editors - Barrett Mattingly from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Barrett Mattingly, Lucinda hampton, Jess Bell, Admin, Uchechukwu Chukwuemeka, Robin Tacchetti, Kim Jackson, Kirenga Bamurange Liliane, Dave Pariser, WikiSysop, Anna Fuhrmann, 127.0.0.1, Heidi Johnson Eigsti, Elaine Lonnemann, Wendy Walker and Meaghan Rieke
Introduction[edit | edit source]
Osteogenesis imperfecta (OI) is a "heterogeneous group of congenital, non-sex-linked, genetic disorders".[1] It affects the production or processing of type 1 collagen, and therefore, impacts connective tissue and bone.[1][2]
It is also referred to as "brittle bone disease". Individuals with OI are susceptible to fractures and reduced bone density.[2] They may present with osteoporosis and blue sclera (i.e. the white part of the eye), and their teeth and hearing can be affected.[1] It can also impact mobility and an individual's ability to perform activities of daily living.
OI can also have a negative effect on the social and emotional well-being of young people with this condition and their families. Adopting a coordinated, multidisciplinary team approach helps to ensure that children with OI can "fulfill their potential, maximizing function, independence, and well-being."[3]
Types of OI[edit | edit source]
There are at least eight different types of OI, but three types are said to be easily distinguished.[1]
- Type I:[4]
- The most common and mildest type of OI
- Around 50% of children with OI have Type 1 OI
- Individuals have few fractures / deformities
- Type II:[4][2]
- The most severe type of OI - it is a lethal condition, usually within weeks of birth
- Causes severe disruption of "qualitative function" of the collagen molecule[2]
- Infants with Type II OI present with very short arms and legs, small chest and they have delayed ossification of the skull (so it is softer)
- There may be fractures at birth, low birth weight, under-developed lungs
- May also have a low birth weight and lungs that are not well developed
- Type III:[4]
- Children who have severe clinical signs tend to have Type III OI
- Tend to present with moderate to severe fragility of bones, coxa vera, they may have slightly shorter arms and legs, and have arm, leg, and rib fractures
- Infants may have a larger head, a triangular-shaped face, changes in their chest and spine (scoliosis), difficulties with breathing and swallowing
- May also have frontal bossing (i.e. prominent forehead), basilar invagination, short stature
- Symptoms vary in each infant[4]
- Types IV to VIII are not common and vary in terms of their severity.[1]
Epidemiology[edit | edit source]
OI is a rare condition. The estimated incidence is approximately 1 in every 15,000 to 20,000 births.[2] It affects males and females equally, and there are no differences in differences in terms of race / ethnic group.[1]
Aetiology[edit | edit source]
OI usually occurs secondary to mutations in the COL1A1 and COL1A2 genes, but there have been diverse mutations related to OI identified more recently.[2]
Pathology[edit | edit source]
In OI, the synthesis of type I collagen is affected. Type I collagen forms the main protein of the extracellular matrix of many of our tissues, including our skin, bones, tendons, skin and sclerae.[1][2]
Clinical presentation[edit | edit source]
The clinical presentation of osteogenesis imperfecta is highly variable, ranging from a mild form with no deformity, normal stature and few fractures to a form that is lethal during the perinatal period.
In general, four major clinical features characterise osteogenesis imperfecta:
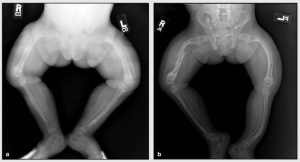
- Osteoporosis with abnormal bone fragility Image 4: X-ray OI
- Easily broken bones
- Bone deformities
- bowing of the legs
- barrel-shaped chest
- curved spine
- triangle-shaped face[4]
- Discoloration of the sclera (white of the eye)
- may be blue or gray in color
- Dentinogenesis imperfecta, a disorder of tooth development
- causes the teeth to be discolored (most often a blue-gray or yellow-brown color) and translucent.
- teeth are also weaker than normal, making them prone to rapid wear, breakage, and loss.
- can affect both primary (baby) teeth and permanent teeth[5].
- Hearing impairment
Other features include ligamentous laxity and hypermobility of joints, short stature and easy bruising.[1]
Diagnosis[edit | edit source]
The baby's healthcare provider or the specialists may recommend the following diagnostic tests:
- X-rays. These may show many changes such as weak or deformed bones and fractures.
- Lab tests. Blood, saliva, and skin may be checked. The tests may include gene testing.
- Dual Energy X-ray Absorptiometry scan (DXA or DEXA scan). To check for softening.
- Bone biopsy. A sample of the hipbone is checked[4].
Treatment[edit | edit source]
The main goal of treatment is to prevent deformities and fractures. As they age, the goal is to allow him or her to function as independently as possible.
Management options include:
- Surgical correction of deformities and the prevention of fractures
- Intramedullary rods with osteotomy are used to correct severe bowing of the long bones
- Intramedullary rods are also recommended for children who repeatedly fracture long bones
- Different types of rods (surgical nails) are available to address issues related to surgery, bone size, and the prospect for growth; the two major categories of rods are telescopic and non-telescopic.
- Care of fractures. The lightest possible materials are used to cast fractured bones. To prevent further problems, it is recommended that a child begin moving or using the affected area as soon as possible.
- Bisphosphonates
- Growth hormone therapy[1]
- Dental procedures: Treatments including capping teeth, braces, and surgery may be needed.
- Physical and occupational therapy are both very important in babies and children with OI.
- Assistive devices. Wheelchairs and other custom-made equipment may be needed as babies get older[4].
Prognosis[edit | edit source]
Varied across the diverse spectrum of the disease.
- Age of onset of long bone fractures has been demonstrated as an important prognostic indicator for ambulatory ability.
- Survival: The most significant indicators include the location of fractures, the severity of fractures and general radiographic appearance of the skeleton.
- Engelbert et al. demonstrated that: children who achieved independent sitting or standing or both by 12 years of age, were finally able to ambulate; children who could achieve independent sitting or standing, or both, by the age of 12 months were likely to be able to walk[2]
Complications[edit | edit source]
Complications may affect most body systems in a baby or child with OI. The risk of developing complications depends on the type and severity of your baby's OI. Complications may include the following:
- Respiratory infections eg. COVID 19, pneumonia
- Heart problems eg. poor cardiac valve defects
- Kidney stones
- Joint problems
- Hearing loss
- Eye conditions and vision loss
Team Approach[edit | edit source]
Physical and occupational therapy are part of an interdisciplinary approach to treatment. The medical team may also include a primary care physician, orthopedist, geneticist, nutritionist, social worker, and psychologist. Children and adults with OI, especially those with spine curves which may affect pulmonary status, may regularly see a pulmonologist. Ideally planning ahead for rehabilitation is included in the preparation for surgery. [6]
Physiotherapy[edit | edit source]
When working with individuals and families living with OI, therapists should keep these principles in mind:
- Listen: It is essential to listen to individuals with OI and their families and respect their input.
- Set Goals: Make goals incremental, realistic and achievable.
- Fear of Fractures is another serious constraint to movement: Establishing safe movement procedures, encouraging self-confidence and optimizing strength are strategies that can help resolve this issue. Passive range of motion is not recommended with new clients.
- Expect Success. With the proper environment and equipment, the majority of children and adults with OI can function well in many or most areas of daily life including but not limited to self-care, school and work.
Maximizing a person’s strength and function not only improves overall health and wellbeing, but also improves bone health, as mechanical stresses and muscle tension on bone help increase bone density. eg, deformities such as a flattened skull, a lordotic back, or tight hip flexor muscles can be prevented or minimized through therapy.
Approaches include:
- Exercise including weight bearing activities (braces may be needed), and recreational activities low-impact activities such as swimming, once precautions are defined.
- Encouraging different body positions and postures during the day and safe handling to strengthen muscle groups and prevent deformities.
- Adaptive equipment. Depending on the environment, a variety of mobility aides may be needed (cane, walker, manual or power wheelchair).
- Environmental adaptations in the home, school or workplace.[6]
Circumstances requiring intermittent or long-term physical therapy:
- When a child with OI has delays or weakness in motor skills
- When a child or adult with OI is recovering from a fracture, surgery or injury
- When a person with OI experiences fear of movement and trying new skills and activities.
- When a person with OI reaches a transition point in life, they must adapt to a new environment or require ADL training.[6]
Key Principles of Therapeutic Strategies
Patience and task analysis are both necessary to develop a successful therapy program. Developmental concepts and specific skills need to be analyzed closely, so that many small improvements can lead to achieving a particular therapy goal.
Key therapeutic strategies include the following:
1. Skill Progression - gross motor skills may be delayed or difficult for those with moderate to severe OI; In order to learn person care skills, basic gross motor skills need to be developed (reaching, sitting, etc.)
2. Preventive positioning, protective handling and active movement with gradual progression facilitate safe development of motor skills
3. Water therapy - allows for reduced gravity environment and a great starting place in the face of fear of movement; Adults often use water therapy to maintain or relearn motor skills.
4. Equipment - various equipment from wheelchairs to pillows can contribute to achieving personal and motor goals
5. Encouraging healthy living and participation in recreational activities to promote general health and prevent obesity [6]
Children of Glass[edit | edit source]
Excerpts from the Discovery Health documentary on the genetic brittle bone disorder "Osteogenesis Imperfecta", courtesy of Youtube.com.
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Osteogenesisi Imperfecta. Available from: https://radiopaedia.org/articles/osteogenesis-imperfecta-1 (Accessed, 15/10/ 2021).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Subramanian S. StatPearls Publishing LLC.; Treasure Island, FL, USA: 2021. Osteogenesis Imperfecta.
- ↑ Marr C, Seasman A, Bishop N. Managing the patient with osteogenesis imperfecta: a multidisciplinary approach. Journal of multidisciplinary healthcare. 2017; 10:145.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Osteogenesis Imperfecta. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/osteogenesis-imperfecta (Accessed, 15/10/2021).
- ↑ Dentiogenesis Imperfecta. Available from: https://medlineplus.gov/genetics/condition/dentinogenesis-imperfecta/ (Accessed, 15/10/2021).
- ↑ 6.0 6.1 6.2 6.3 OI foundation Physical and Occupational Therapists Guide to Treating Osteogenesis Imperfecta Available:https://oif.org/wp-content/uploads/2019/08/PT_guide_final.pdf (accessed 15.10.2021)
- ↑ Bublitz Videos. Children of Glass - (Part 1 of 4). Available from: http://www.youtube.com/watch?v=TpAMTOud3bw [last accessed 27/8/2020]
- ↑ Bublitz Videos. Children of Glass - (Part 2 of 4). Available from: http://www.youtube.com/watch?v=GTpSxlPzC8k [last accessed 37/8/2020]
- ↑ Bublitz Videos. Children of Glass - (Part 3 of 4). Available from: http://www.youtube.com/watch?v=L2f8fz6vzoI [last accessed 27/8/2020]
- ↑ Bublitz Videos. Children of Glass - (Part 4 of 4). Available from: http://www.youtube.com/watch?v=QvbY7XqyMz8 [last accessed 27/8/2020]