Hip Osteoarthritis
Original Editors - Eric Robertson, Kim Presiaux
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.Search Strategy[edit | edit source]
Database: Pubmed
Keywords: Treatment OA, Exercise OA, OA
Database: Website Library VUB
Keywords: Treatment OA, Exercise OA, OA
Definition/Description[edit | edit source]
Hip osteoarthritis is a common type of osteoarthritis. Since the hip is a weight-bearing joint, osteoarthritis can cause significant problems.
Hip osteoarthritis is caused by deterioration of articular cartilage of the hip joint.
There are several reasons this can develop:
• Previous hip injury
• Previous fracture, which changes hip alignment
• Genetics
• Congenital and developmental hip disease
• subchondral bone that is too soft or too hard[1]
Clinically Relevant Anatomy[edit | edit source]
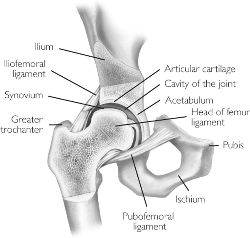
The hip joint is a synovial ball and socket joint, with the convex femoral head articulating with the concave acetabulum. Stability of the joint is achieved through a combination of muscle action and several ligaments forming a loose, but strong joint capsule, the iliofemoral ligament, the ischialfemoral ligament and the pubofemoral ligament. Another ligament, the ligamentum teres, does not provide stability to the hip but offers a portion of blood supply to the femoral head in some individuals.
The femoral head and acetablum are covered by smooth hyaline cartilage, and the acetabulum contains a labrum, which functions to facilitate movement and support the forces passed through the joint.
The hip, despite the requirement to support the weight of the body, has the second largest exursion of motion of any joint in the body.
External Link: [Hip Anatomy Video]
<== Epidemiology /Etiology ==>
add text here
Characteristics/Clinical Presentation[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
add text here
Diagnostic Procedures[edit | edit source]
Altman et al have established guidelines by which clinical diagnosis of hip osteoarthritis can be made. The guidelines, established in 1991, present a 3 pronged approach to diagnosis of hip osteoarthritis including clinical, radiological, and laboratory findings. According to these guidlelines, a patient was considered to have osteoarthritis if they presented with:
- Hip Pain and...
- Hip Internal Rotation < 15 degrees and Hip Flexion less than or equal to 115 degrees
or, hip pain in combination with:
- Hip Rotation < 15 degrees or...
- Pain with Hip Internal Rotation or...
- Hip stiffness in the AM less than 60 minutes or...
- Age > 50 years
More recently, Sutlive et al have proposed a clinical prediction rule to identify individuals with hip osteoarthritis presenting with unilateral hip pain.
add text here related to medical diagnostic procedures
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
The beginning of OA is characterized by limited
abduction and rotation in the hip joint. Later on flexion, extension, adduction,.. will become more difficult.
Physiotherapeutic examination [2]
1) Palpation of M. gluteus medius.
Position: patient lies on his side. Upper leg in adduction and flexion
OA: Zone of greater Trochanter is sensitive and painful.
2)Flexion and forced flexion
Position: patient lies on his back.
OA: Flexion is limited.
3) Extension Position: Patient in prone. Physiotherapist stabilizes the pelvis and raises the leg.
OA: Amplitude is limited.
4) Abduction and adduction
Position: Patient lies on his back. Physiotherapist stabilizes the pelvis and performs abduction and adduction.
OA: abduction is limited, adduction keeps normal amplitude.
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
Treatment goals: improve strength, coordination, mobility, balance, stand, stability, flexibility. Reduce pain.
USUAL CARE
Passive exercises
- Position patient: supine, hip in 15-30° flexion, 15-30° AB, slight ER
Physiotherapist: perform 3-6 thrusts at the beginning of the first set then perform oscillations.
- Positions patient: supine with hip flexed
Physiotherapist: oscillatory passive mobilizations, applied caudally or laterally to the proximal thigh
- Position patient: Prone with knee flexed.
Physiotherapist: IR until contralateral pelvis rises, apply oscillatory force downwards to contralateral pelvis.
- Firm effleurage stroke, deep frictions or sustained pressure trigger point release with the muscle on stretch.
- Position patient: Prone. The hip is in 10-15 ° AB.
Physiotherapist: Perform caudally directed oscillations. May perform 3-6 thrusts at the beginning of the first set.
- Position patient: Supine with hip in flexion and adduction.
Physiotherapist: Use body weight to impart passive oscillations to the postero-lateral hip capsule through the long axis of the femur. Add more flexion, adduction, &/or internal rotation to progress.
- Massage of quads, hamstrings, psoas, adductors, abductors, gluteus-muscles
Active exercises
- Knee to chest exercise (strengthens the abdominal muscles and improves
the flexibility of the hip, back and neck) Patient lies on the floor with left leg straight and right foot flat on the floor. Grabs his knee and bring it toward to his chest, holds for 30seconds and switches legs.
- Bridging exercise ( strengthens buttock abdominal and hamstrings
muscles) Patient lies on his back with knees bent and feet flat on the floor. While tightening abdominal muscles he lifts his pelvis slightly upwards. Hold for 15-20 seconds. Repeat 8-12 times.
- Balance exercises
( Standing weight shifting forwards/ lateral, Standing in double leg stance on foam, Shuttle walking, Stairs)
- Endurance exercises
Walk, cycle, swim
Advice and education
In the treatment it is very important to tell the patient about his condition. Why does it occur? What's the treatment? What's the importance of exercise?
This will make the patient have a clear understanding in his condition and will improve the healing.
It’s also very important to tell the patient what he can and can not do.
BGA
Behavioral graded activities is an kind of treatment that contains normal exercise therapy comprising booster sessions.
The long term effectiveness have been showed, but it is never proved that this treatment has a better efficacy than usual care.
BGA intervention consists of 3 phases:
1) Starting phase: The physiotherapist will educate the patient about his condition.
And there will be made a list of treatment goals and problematic activities.
2) Treatment phase: increasingly difficult exercises.
3) Integration phase: The physiotherapist will support and integrate behavioral change.
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
References[edit | edit source]
see adding references tutorial.
</div>