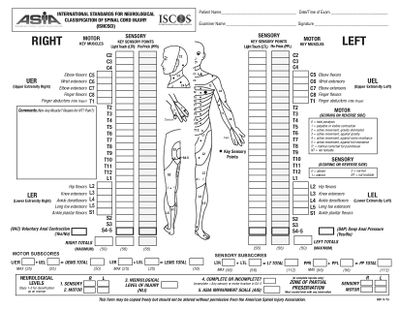
American Spinal Injury Association (ASIA) Impairment Scale
Original Editor - Daphne Jackson.
Top Contributors - Naomi O'Reilly, Arnold Fredrick D'Souza, Stacy Schiurring, Kim Jackson, Jess Bell, Admin, Abbey Wright, Tarina van der Stockt, Rucha Gadgil and Olajumoke Ogunleye
Overview[edit | edit source]
Conduction of Sensory and Motor signals and the autonomic nervous system is affected by spinal cord injury. By systematically examining the dermatomes and myotomes, one can determine the cord segments affected by the spinal cord injury. The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI), commonly referred to as the ASIA Exam, was developed by the American Spinal Injury Association (ASIA) as a universal classification tool for Spinal Cord Injury based on a standardized sensory and motor assessment, with the most recent revised edition published in 2011. The impairment scale involves both a motor and sensory examination to determine the Sensory Level and Motor Level for each side of the body (Right and Left), the single Neurological Level of Injury (NLI) and completeness of the Injury i.e. whether the injury is complete or incomplete. [1]
Sensory Examination[edit | edit source]
Key Sensory Points, readily located in relation to bony anatomical landmarks in each of the 28 Dermatomes C2 - S5, are tested bilaterally using light touch and pin-prick (sharp-dull discrimination). Equipment common to clinical settings may be used, such as a cotton bud for light touch and a neurotip or safety pin for pin-prick. Appreciation of light touch and pin prick sensation at each of the key points is made in comparison to sensation on the patient’s cheek as a normal frame of reference. [1]
A three-point scale is used for scoring:
| 0 | = | Absent |
| 1 | = | Altered - Impaired or Partial Appreciation, including Hyperesthesia |
| 2 | = | Normal or Intact - Similar as on the Cheek |
| NT | = | Not Testable |
| Level | Description of Key Points for Sensory Testing |
|---|---|
| C2 | 1 cm lateral to Occipital Protuberance |
| C3 | Supraclavicular Fossa at Midclavicular Line |
| C4 | Over Acromioclavicular Joint |
| C5 | Lateral Side Antecubital Fossa just Proximal to Elbow Crease |
| C6 | Dorsal Surface of Proximal Phalanx of the Thumb |
| C7 | Dorsal Surface of Proximal Phalanx of the Middle Finger |
| C8 | Dorsal Surface of Proximal Phalanx of the Little Finger |
| T1 | Medial Side Antecubital Fossa, just Proximal to Medical Epicondyle of Humerus |
| T2 | Apex of Axilla |
| T3 | Midclavicular Line and 3rd Intercostal Space |
| T4 | Midclavicular Line and 4th Intercostal Space at Nipple Line |
| T5 | Midclavicular Line and 5th Intercostal Space Midway between T4 and T6 |
| T6 | Midclavicular Line and 6th Intercostal Space at the level of Xiphisternum |
| T7 | Midclavicular Line and 7th Intercostal Space Midway between T6 and T8 - Quarter the Distance between Level Xiphisternum and Umbilicus |
| T8 | Midclavicular Line and 8th Intercostal Space Midway between T6 and T10- Half the Distance between Level Xiphisternum and Umbilicus |
| T9 | Midclavicular Line and 9th Intercostal Space Midway between T8 and T10 - Three Quarters the Distance between Level Xiphisternum and Umbilicus |
| T10 | Midclavicular Line and 10th Intercostal Space at the Level of Umbilicus |
| T11 | Midclavicular Line and 11th Intercostal Space Midway between T10 and T12 - Midway between Level of Umbilicus and Inguinal Ligament |
| T12 | Midclavicular Line Over Midpoint Inguinal Ligament |
| L1 | Midway between Sensory Point at T12 and L1 |
| L2 | Anterior-Medial Thigh at the Midpoint drawn connecting the Midpoint of Inguinal Ligament and the Medial Femoral Condyle |
| L3 | Medial femoral Condyle above the Knee |
| L4 | Medial Malleolus |
| L5 | Dorsal Foot at 3rd Metatarsal Phalangeal Joint |
| S1 | Lateral Aspect Calcaneus |
| S2 | Midpoint Popliteal Fossa |
| S3 | Over Ischial Tuberosity or Infragluteal Fold |
| S4 - 5 | Perianal Area < 1cm Lateral to Mucocutaneous Junction |
| Deep Anal Pressure |
|---|
| A gentle pressure with the examiner’s finger is applied to the internal, anorectal wall, innervated by the somatosensory components of the pudendal nerve S4/5. Perceived pressure is graded as absent or present. Any reproducible pressure sensation felt in the anal area during this part of the exam signifies that the patient has a sensory incomplete lesion. [1] |
Sensory Level[edit | edit source]
Defined as the most caudal, intact dermatome for both light touch and pin prick (sharp/dull discrimination) sensation. The sensory level is determined, as above, by performing an examination of the key sensory points within each of the 28 dermatomes on each side of the body, and may be different for the right and left side .
Sensory Score[edit | edit source]
Sensory scores of each dermatome for pin-prick and light touch can be summed across dermatomes and sides of body, right and left, to generate two summary sensory scores: Pin-prick and Light Touch. The sensory score, provide a means of numerically documenting changes in sensory function, but cannot be calculated if any required key sensory point is Not Testable. [1]
Normal sensation for each modality is assigned a score of 2. A score of 2 for each of the 28 key sensory points for Light Touch on each side of the body would result in a maximum score of 56 for Light Touch. A score of 2 for each of the 28 key sensory points for Pin-Prick on each side of the body would result in a maximum score of 56 for Pin-Prick. Total Maximum Sensory Score of 112
Motor Examination[edit | edit source]
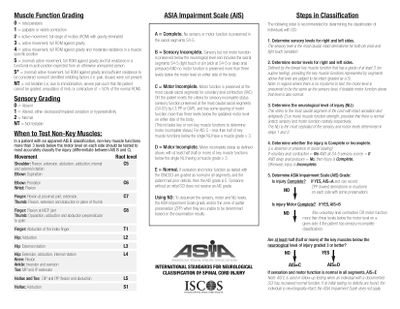
Key Motor Functions of the 10 Paired Myotomes C5 - T1 and L2 - S1 are tested bilaterally. Improper positioning and stabilization can lead to substitution by other muscles, and will not accurately reflect the muscle function being graded. [1] A six-point scale is used for scoring:
| 0 | = | Total Paralysis |
| 1 | = | Palpable or Visible Contraction |
| 2 | = | Active Movement, Full Range of Motion with Gravity Eliminated |
| 3 | = | Active Movement, Full Range of Motion Against Gravity |
| 4 | = | Active Movement, Full ROM Against Gravity and Moderate Resistance in a Muscle Specific Position |
| 5 | = | Normal Active Movement, Full Range of Motion Against Gravity and Full Resistance in a Muscle Specific Position expected from an Unimpaired Person |
| 5* | = | Normal Active Movement, Full Range of Motion Against Gravity and Sufficient Resistance to be considered normal if identified Inhibiting Factors
i.e., pain, disuse were not present |
| NT | = | Not Testable
i.e., due to Immobilization, Severe pain such that the patient cannot be graded, Amputation of Limb, or Contracture of >50% of the Range of Motion |
Voluntary Anal Contraction: The patient is asked to voluntarily contract the external anal sphincter around the examiner’s finger. [1] The contraction is scored as absent or present.
Motor Level[edit | edit source]
The Motor Level is defined by the lowest key muscle function that has a grade of at least 3 (on supine testing), providing the key muscle functions represented by segments above that level are judged to be intact (graded as a 5). The motor level is determined, as above, by examining the key muscle function within each of the 10 myotomes on each side of the body, and may be different for the right and left side. [1]
In regions where there is no myotome that are clinically testable i.e., C1 to C4, T2 to L1, and S2 to S5, the Motor Level is presumed to be the same as the Sensory Level, if testable motor function above that level is also normal. [1]
- Example 1: If the sensory level is C4, and there is no C5 motor function strength (or strength graded <3), the motor level is C4.
- Example 2: If the sensory level is C4, with C5 key muscle function strength graded as 4, the motor level would be C5 because the strength at C5 is at least 3 with the “muscle function” above considered normal: presumably if there was a C4 key muscle function it would be graded as normal since the sensation at C4 is intact.
Motor Score[edit | edit source]
Motor scores for each myotome can be summed across myotomes and sides of body, right and left, to generate a single motor score for each of the upper limbs and lower limbs. The Motor Score, provide a means of numerically documenting changes in motor function, but cannot be calculated if any required muscle function is Not Testable.
Normal strength is assigned a grade of 5 for each muscle function. A score of 5 for each of the five key muscle functions of the upper extremity would result in a maximum score of 25 for each extremity, totaling 50 for the upper limbs. A score of 5 for each of the five key muscle functions of the lower extremity would result in a maximum score of 25 for each extremity, totaling 50 for the lower limbs.
Determination of Neurological Level of Injury[edit | edit source]
The Neurological Level of Injury is determined by identifying the most caudal segment of the cord with intact sensation and antigravity (3 or more) muscle function strength on both sides of the body, provided that there is normal, intact sensory and motor function rostrally.
- Sensory Level refers to the most caudal, intact dermatome for both light touch and pin-prick sensation (Score=2).
- Motor Level refers to the most caudal myotome with a key muscle function of at least Grade 3 on MMT.
- If there is a discrepancy between the most caudal intact section between the four possible levels of Right-Sensory level, Left-Sensory level, Right-Motor level, or Left-Motor level, the Neurological Level of Injury is considered the most cephalad segment of these four levels. [1]
ASIA Impairment Scale (AIS)[edit | edit source]
Spinal Cord Injuries are classified in general terms of being neurologically “Complete” or “Incomplete” based upon Sacral Sparing, which refers to the presence of Sensory or Motor Function in the most Caudal Sacral Segments i.e. preservation of light touch or pin prick sensation at S4-5 Dermatome, Deep Anal Pressure or Voluntary Anal Sphincter Contraction..
Complete Injury is defined as the absence of Sacral Sparing i.e. no Sensory and Motor Function at S4-5
Incomplete Injury is defined as the presence of Sacral Sparing i.e. some preservation of Sensory and/or Motor Function at S4-5
| Grade | Type of Injury | Description of Injury |
|---|---|---|
| A | Complete | No Sensory or Motor Function is preserved in the Sacral Segments S4-S5 |
| B | Sensory Incomplete | Sensory but not Motor Function is preserved below the neurological level and includes the Sacral Segments S4-S5,
AND No Motor Function is preserved more than three levels below the Motor Level on either side of the body |
| C | Motor Incomplete | Motor Function is preserved below the Neurological Level
AND More than half of key muscle functions below the Neurological Level of Injury have a muscle grade less than 3 (Grades 0-2) |
| D | Motor Incomplete | Motor function is preserved below the neurological level
AND At least half (half or more) of key muscle functions below the NLI have a muscle grade ≥ 3 |
| E | Normal | If sensation and motor function as tested with the ISNCSCI are graded as normal in all segments
AND the patient had prior deficits Then the AIS Grade is E. |
| Someone without a Spinal Cord Injury does not receive an AIS Grade. | ||
Zone of Partial Preservation[edit | edit source]
The Zone of Partial Preservation is only used with Complete Injuries (AIS A), and refers to the dermatomes and myotomes caudal to the sensory or motor level that remains partially innervated. [1]
Evidence[edit | edit source]
Reliability[edit | edit source]
The ISNCSCI sensory and motor examinations are reliable when conducted by a trained examiner. [4] Formal training in the administration of the ISNCSCI Standards has been shown to improve the accuracy of the examiner’s classification. [5]
Validity[edit | edit source]
The ISNCSCI are validated for injury classification. [6] Construct validity of the ASIA Motor Score as a measure of recovery following spinal cord injury and as an outcome measure for clinical trials is greater when upper and lower extremity motor scales are scored independently and not summated together. [6]
Patient Explanation[edit | edit source]
Explaining the exam to your Patients- This test will help us determine where your spinal cord was injured
- It might be different than what was seen on the MRI or CT Scan
- This is the main test we use to determine what level your injury was, how severe it was, and a rough idea of what we could expect for recovery
Resources[edit | edit source]
ASIA E-Learning Centre InSTeP: International Standards
- To promote the teaching and competent use of the Standards, ASIA with contribution from the International Spinal Cord Society has developed the International Standards Training e-Learning Program or InSTeP.
ASIA E-Learning Centre ASTeP: Autonomic Anatomy & Function
- The goal of this training for the Autonomic Standards is to learn normal autonomic functions, understand the changes in autonomic functions following spinal cord injury (SCI) and use the Autonomic Assessment to document and classify remaining autonomic neurological function.
ASIA Impairment Scale: International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) Assessment Form
ASIA Impairment Scale: Autonomic Standards Assessment Form
ASIA Impairment Scale: Motor Exam Guide
ASIA Impairment Scale: Key Sensory Points
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Burns S, Biering-Sørensen F, Donovan W, Graves D, Jha A, Johansen M, Jones L, Krassioukov A, Kirshblum, Mulcahey MJ, Schmidt Read M, Waring W. International Standards for Neurological Classification of Spinal Cord Injury, Revised 2011. Top Spinal Cord Inj Rehabil 2012;18(1):85-99.
- ↑ Kaplan M. Kaplan - ASIA assessment. Available from: http://www.youtube.com/watch?v=IP_wunjn9Io[last accessed 30/10/18]
- ↑ SCIREWebVideo . Common Errors Made During the ISNCSCI Examination (ASIA Exam). Available from: https://www.youtube.com/watch?v=PpgGzIhCpuI[last accessed 30/10/18]
- ↑ Marino R, Jones L, Kirshblum S, Tal J, Dasgupta A. Reliability and repeatability of the motor and sensory examination of the international standards for neurological classification of spinal cord injury. J Spinal Cord Med 2008;31(2)166-170.
- ↑ Schuld C, Wiese J, Franz S, Putz C, Stierle I, Smoor I, Weidner N, EMSCI Study Group, Rupp RR. Effect of formal training in scaling, scoring and classification of the international standards for neurological classification of spinal cord injury. Spinal Cord 2013;51(4):282-8.
- ↑ 6.0 6.1 Graves D, Frankiewicz RG, Donovan WH. Construct validity and dimensional structure of the ASIA motor scale. J Spinal Cord Med 2006;29(1):39-45.