ACL Rehabilitation: Rehabilitation Planning
Original Editor - Mariam Hashem
Top Contributors - Mariam Hashem, Kim Jackson, Tony Lowe, Tarina van der Stockt, Simisola Ajeyalemi, Jess Bell, Chelsea Mclene, Robin Tacchetti, Leana Louw, Wanda van Niekerk, Abbey Wright, Olajumoke Ogunleye and Rachael Lowe
Considerations Before Setting up a Plan[edit | edit source]
Following the first 6 weeks of acute management after ACL reconstruction, creating a log-term rehabilitation plan can be challenging for physiotherapists. It is important to set specific goals and milestones for your athlets and build time frames accordingly. These goals should be priotorized depending on athletic needs.
In the acute management phase, there are some considerations to protect the surgical repair and allow scar heeling without compromising ROM.
Protection and Restrictions:[edit | edit source]
1-ROM: patient can move freely either actively or passively throughout the available ROM within pain tolerance.
2-Bracing: This is an area of great controversy in the literature and in clinical practice. While bracing may not be beneficial on the long run, some clinicians prefer placing the knee in a mobilizer then replace it with a c-hinge functional knee brace once femoral nerve block wears off following the surgery. However, the main purpose of bracing is to prevent re-injury in the acute stage. This is depenable on the environmental exposure, for example, bracing is essential to prevent re-injury if the patient is in risk for slipping due to snow. A different environment may not require bracing.
3-Weight-Bearing: while full weight-bearing may be tolerated in the first few weeks, partial weight bearing is preferred to protect scar, allow healing and restore joint homeostasis as soon as possible.
4- Stationary bike: introduced on day 10 or once 110° of knee ROM is achived. However, you may use a small range of rocking back and forth as a way of facilitating ROM if the whole range is still restricted.
5-Resistance weight-bearing strength training: delayed until 6 weeks after surgery to avoid scar hypertrophy and stiffness.
The evidence is rich in ACL-rehabilitation protocols. There is no specific program that is superior to the others, however, there are mutual goals considered in all rehabilitation progrmas.
The intermediate rehabilitation phase goals:
- Knee flexion within 10° of the contralateral side
- Quadriceps index greater than 60%[1].
Quadriceps Index is :''the ratio of involved-side quadriceps strength to uninvolved-side quadriceps strength"[1]
Quadriceps strength can be easily quantified using a handheld dynamometer to identify strength deficits and differences between the two sides[2].
Late rehabilitation phase goals:
- Quadriceps index greater than 80%
- Normal gait pattern
- Full knee ROM
- Knee joint effusion equal to a grade of trace or less[1]. Assessed using the modified stroke test.
Knee Symmetry[edit | edit source]
Comparing the injured knee to the other side and trying to reach as much as possible symmetry is essential for recovery and return to funciton. It could be described as a vicious cycle of abnormal loading pattern leading to loss of strength, resulting in more abnormal loading patterns.
Symmetry means equal ROM and equal strength. Loss of as little as 2° of extension and 5° flexion, compared to the other knee, were associated with lower subjective scores[3].
Researchers consider ROM symmetry to be the most important factors in successful rehabilitaiton and long-term patient satisfaction.
Achieving symmetry depends on many factors such as surgical approach; graft type, donor site, proper graft placement, knee hyperextension after graft placement, pre-operative rehab, post-operative, rehab periodic evaluations and follow-ups up to 10 years after surgery[4].
A problem may arise when the surgical graft is obtained from the contralteral leg. Regaining full ROM for both knees should be aimed during rehabilitaiton. Regardless of the donor site, both knees should be incorporated throughout the rehabilitation process[4].
Creating a Plan[edit | edit source]
As a physiotherapist, you have a role in guiding your patient through a long-term rehabilitation plan. Setting up milestones and goals depends on your patient's needs and aspired funciton. Predicting outcomes and time-frames, using your clinical exprinece and clinical reasoning skills, for each goal is also part of your role.
The ACL rehabilitation plan has 9 Phases:
1-ROM: Aiming to maintian available range and facilitate regaining of full ROM. At this phase you should also manage effusion and inflammation and achieve knee terminal extension. This stage starts immediately after surgery and lasts up to the 6th week. Full ROM is identified as the primary factor for successful outcomes[5]. In addition, early restoration of ROM reduces the risk of arthrofibrosis[6]. Achieving full knee extension in the early stage of rehabilitation doesn't affect the stability of the graft[7].
2-Increase Weight Bearing tolerance gradually. Depending on the complxity of the injury:
- A single ACL injury requires 2 weeks of partial weight bearing, then the patient is allowed full weight bearing. Despite being able to tolerate full weight bearing, partial weight bearing is required to allow scar healing. Thus, we could allow immediate transition from parital to full weight bearing without gradual building of tolerance.
- ACL injury combined with meniscus and/or chondral injury would take up to 6 weeks to full weight bearing. In this case, we need to increase the tolereance gradually.
3- Building muscular endurance: this also depends on the joint pathology and may take up to 8 weeks. So this goal is expected to be achieved between the 10-18th week of rehabilitation.
4- Developing strength: research shows weakness in hip, knee and ankle muscles following ACL injury with knee flexor and extensor weaakness persisting for longer peroiod after surgery[8]. Expected regaining of strength between 19-26th week.
5-Muscular power: time frame around 27-32th week.
6- Building running tolerance: not all sports demand the same volume of running.Depending on the athletic's needs, start a designed running program on the 27th week over a 4-6 weeks period.
7-Speed and agility trianing: at week 32, introduce uni-directional drill training for a week then progress to multi-directional training.
8- Return to training: expected around week 35.
9-Return to play: around week 38.
Time frames vary among different sports.The previous are suggetions to build a road map for you and your patient. Rushing rehabilitation may lead to adverse complications such as increased inflammation and loss of ROM[5].
Weekly Plan[edit | edit source]
When setting a weekly plan, consider the priorites for your athlete and the required levels of different physiological characteristics.
The following is a suggested weekly plan for an athlete requires strong lower body as the top priority, cardiovascular fitness, core stability and upper body strength:
Accordingly, the plan includes 4 lower body strengthning sessions, 2 cardio sessions, 2 pool sessions, 2 core sessions, 2 upper body strengthning sessions.
| Monday | Lower body strengthning + cardio |
| Tuseday | Lower body + upper body strengthning |
| Wednesday | Low load recovery (core stability + pool exercise) |
| Thursday | Same as Monday |
| Friday | Same as Tuseday |
| Saturday | Same as Wednesday. |
| Sunday | Off |
Selecting Proper Exercises and Parameters[edit | edit source]
Endurance is the ability to exert work for prolonged time and resist fatigue. Exercises should be light intensity (<50% of 1-RM) high repeitions (15-20) for 3 or more sets with less than 60 seconds of rest, 2-3 times weekly with 48 hours rest between sessions to target type 1 atrophied muscle fibers, due to arthrogenic inhibition[9].
Moving from endurance to strength training can start when the athlete shows[9]:
- Ability to walk on treadmill or cycle with resistance for 20 minutes.
- Similar active ROM to the opposite side
- Back leg squat/Leg press for 10 rep at >70% of the predicted 10 RM.
- 15 reps single leg squat from a 10 inch step/box
- Anterior reach on the Y-Balance test within 8 cm difference from the opposite leg
- Quadrieps index > 80%
Strength is the ability to exert force/torque at a specific speed. It requires heavy to moderate loads (60-67% of 1-RM), with frequent increase of resistance, either by external weight or single leg posture. Depending on the previous level of strength, 1-12 reps for 1-3 sets with 2 minutes rest between sets. Every two weeks, a week of de-loading is recommended to allow recovery[9].
Selecting specific strengthning exercises depends on what muscles you want to emphasis. For example, building a 30-40 minutes lower body workout would look like
| Muscle | Example | |
|---|---|---|
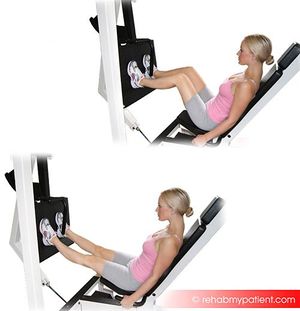
| Quadriceps Dominant | Leg Press | |
| Glutes Dominant | Single Leg Bridge | |
| Hamstrings Dominant | Romanian Deadlift | |
| Quadriceps Dominant | Tuck Squat | |
| Quadriceps Dominant | Single Leg Squat | |
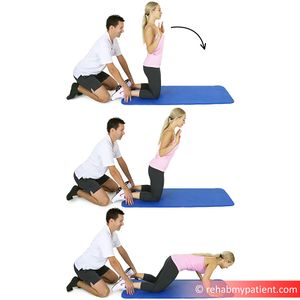
| Hamstrings Dominant | Hamstrings Lean/Nordic Hamstrings Curl |
Further examples and more on the progression of exercises are found in table 6 in this article.
Starting power training should begin when the athlete shows the following criteria:
- Ability to run for 20 minutes
- Back squat/Leg press at 80% of the predicted 10 RM
- Anterior reach distance within 4 cm difference from the opposite leg on the Y-Balance test
- Quad girth within 1 cm compared to the contralateral side
- Quad index at 90%
- Hamstrings/Quad ratio 60%, using a handheld dynamomter
- Passing single leg drop test
A different characteristic of muscular strength is power which is a combination of force and velocity. Training for high load activities requires 85-100% of 1 RM, 1-3 sets with 3 minutes rest. Developing velocity requires lower resistance, about 30% 1 RM for 6 reps, 1-3 sets with 3 minutes rest.
You can implenment a running program when the athlete achives 90% quadriceps index to make sure the running mechanics will be as close to normal[12]. The Vail sports test will give you an idea how your patient loads his/her injured knee which will reflect on running[9]. Increasing running tolerance should be gradual and slow for up to 4 weeks. Alter-G treadmill or pool running is helpful when you want to start with partial weight-bearing, progressing 5% each session till full weigh-bearing. You may begin with 4 minutes of walking to a minute of running repeated 4 times over 20 minutes, 2-3 times per week. Progress each week by increasing a minute of running and decrease a minute of walking, till the athlete is able to run for a progressive 20 minutes. If any signs of overload was present, return to the previous stage of running progression.
| [13] | [14] |
Speed and Agility are important for re-conditioning and return to sport. Build a specific drills program depending on your patient's sport-specific needs.
By the end of this phase your patient must be able to[9]:
- Pass the modified T-test
- Pass single leg hop series with >90% from the opposite side
- Complete 10 rep squat / 10 rep leg press with >90% of the predicted 1RM.
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Adams D, Logerstedt D, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. journal of orthopaedic & sports physical therapy. 2012 Jul;42(7):601-14.
- ↑ Sinacore JA, Evans AM, Lynch BN, Joreitz RE, Irrgang JJ, Lynch AD. Diagnostic accuracy of handheld dynamometry and 1-repetition-maximum tests for identifying meaningful quadriceps strength asymmetries. journal of orthopaedic & sports physical therapy. 2017 Feb;47(2):97-107.
- ↑ Shelbourne KD, Klotz C. What I have learned about the ACL: utilizing a progressive rehabilitation scheme to achieve total knee symmetry after anterior cruciate ligament reconstruction. Journal of Orthopaedic Science. 2006 May 1;11(3):318.
- ↑ 4.0 4.1 Biggs A, Jenkins WL, Urch SE, Shelbourne KD. Rehabilitation for patients following ACL reconstruction: a knee symmetry model. North American journal of sports physical therapy: NAJSPT. 2009 Feb;4(1):2.
- ↑ 5.0 5.1 Biggs A, Jenkins WL, Urch SE, Shelbourne KD. Rehabilitation for patients following ACL reconstruction: a knee symmetry model. North American journal of sports physical therapy: NAJSPT. 2009 Feb;4(1):2.
- ↑ Mayr HO, Weig TG, Plitz W. Arthrofibrosis following ACL reconstruction—reasons and outcome. Archives of orthopaedic and trauma surgery. 2004 Oct 1;124(8):518-22.
- ↑ Saka T. Principles of postoperative anterior cruciate ligament rehabilitation. World journal of orthopedics. 2014 Sep 18;5(4):450.
- ↑ Thomas AC, Villwock M, Wojtys EM, Palmieri-Smith RM. Lower extremity muscle strength after anterior cruciate ligament injury and reconstruction. Journal of athletic training. 2013 Oct;48(5):610-20.
- ↑ 9.0 9.1 9.2 9.3 9.4 Bousquet BA, O'Brien L, Singleton S, Beggs M. POST-OPERATIVE CRITERION BASED REHABILITATION OF ACL REPAIRS: A CLINICAL COMMENTARY. International Journal of Sports Physical Therapy. 2018 Apr 1;13(2).
- ↑ Y Balance Test Explained. Available from: https://www.youtube.com/watch?v=1gfGkxWlx4o
- ↑ Single Leg Drop Jump | OSU Sports Medicine. Available from:https://www.youtube.com/watch?v=yy7GWyMat4Y
- ↑ Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clinical biomechanics. 2002 Jan 1;17(1):56-63.
- ↑ Logan Hutsko - Vail Sport Test. Available from:https://www.youtube.com/watch?v=njfP29KabO4
- ↑ Demonstration of Anti-Gravity Treadmill at Michigan Medicine. Available from:https://www.youtube.com/watch?v=u0o-8MmKArg
- ↑ Agility T-Test. Available from: https://www.youtube.com/watch?v=XkPsoV6-HJw
- ↑ Monday Academic Session - Luke O'Brien - Rehabilitation. Available from: https://www.youtube.com/watch?v=wMc9G7Kzj0w