Hip Osteoarthritis
Original Editor - Eric Robertson, Kim Presiaux
Top Contributors - Kim Presiaux, Dorien De Strijcker, Lucinda hampton, Davy Duverger, Leana Louw, Kim Jackson, Admin, Rachael Lowe, Laura Ritchie, Johnathan Fahrner, Van Horebeek Erika, Scott Buxton, Vidya Acharya, Eric Robertson, Kai A. Sigel, Areeba Raja, 127.0.0.1, Bram Van Roost, Shaimaa Eldib, Lauren Lopez, Loïc Byl, Marius De Bruyn and Kevin Vandebroucq
Definition/Description[edit | edit source]
Osteoarthritis is a condition that causes degeneration of a joint. Hip osteoarthritis mainly affects the articular cartilage, as well as causing changes to the subcondral bone, synovium, ligaments and capsules.[1] This degeneration lead to loss of joint space, which can potentially be symptomatic.[1] It is one of the top 15 contributors of global disability.[2] Hip osteoarthritis is prevalent in 10% of people above 65, where 50% of these cases are symptomatic.[3]
Risk factors[3][4][edit | edit source]
- Previous hip trauma (causing injury or fracture)
- Primary inflammatory arthritis (e.g. rheumatoid arthritis, ankylosing spondylitis)
- Genetics
- Congenital and developmental hip disease (e.g. congenital hip dislocation, Perthe's disease, slipped upper femoral epiphysis)
- Subchondral bone defects
- Obesity
- Occupation causing excessive strain on hips (e.g. manual labor causing repeated loading)
- Increase in age
- Gender (female > male)
- Sport (higher impact sport at a younger age can cause increase in articular cartilage strength, where low impact sport do no change the composition of the cartilage)
- Menopause
- Metabolic diseases and acromegaly
- Sedentary lifestyle
- Femoroacetabular impingement
- Avascular necrosis
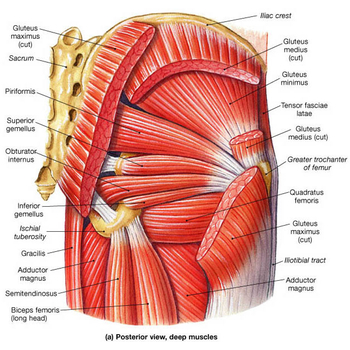
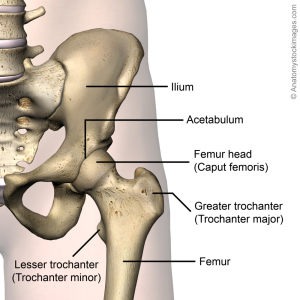
Clinically Relevant Anatomy[edit | edit source]
Epidemiology/etiology[edit | edit source]
Osteoarthritis is the most common disease causing joint complaints. Not only in women but also in men. It’s a disease that strikes many people worldwide, especially old persons. Research tells us that hip osteoarthritis has a prevalence of 11.5 percent in men and 11.6 percent in women. This is almost equal but when we look at knee osteoarthritis, we see that this is more prevalent in women.[5] Then we have some information about the incidence of hip OA.[6] The incidence rate for female was found 2.4/1000 a year and for males 1.7/1000 a year.
You have the personal level risk factors, described above, but you also have some joint level risk factors.[7] There are several causes for hip osteoarthritis:
1. Direct damage by trauma, arthritis, ...
2. Cartilage damage by metabolic process disorders (when there is a disrupt in homeostasis in the joint, more degradation of the cartilage matrix than synthesis)
3. The genetic factor (studies report the genetics are 60% of the risk)
4. Cartilage damage by repeated intra-articular bleedings
5. Congenital hip dislocation
6. Abnormality in stance of the joint (This will lead to a pathological loading pattern resulting in shear stresses)
7. Overload of the cartilage caused by obesity, prolonged overload, sensibility impediment
Additional to 6. :There is also more and more evidence these days that femoroacetabular impingement is an important factor causing hip osteoarthritis. This is what happens if the head of the femur scratches against the labrum what will lead to damage of the labrum and cartilage underneath. With the aid of time, this will result in degeneration of the joint.
A comparable problem is called developmental dysplasia of the hip. This is when the acetabulum doesn’t cover the femoral head enough and lead to instability of the femoral head. The result is shear forces onto the acetabular rim what also will lead to damage and degeneration of the hip joint.
Characteristics/Clinical Presentation[edit | edit source]
The most important characteristic of hip osteoarthritis is that there’s damage to or loss of the articular cartilage.[8] Another typical characteristic is pain, especially pain that starts when the patient starts moving. This pain decreases when the patient keeps on moving or increases when they load the joint for too long or the wrong way. Later on, they will typically complain of a continuous pain and night pain.[8]
Differential Diagnosis[edit | edit source]
A thorough patient history and physical examination should aid the clinican in his/her differential diagnosis. Pain location is often a good indicator of intraarticular versus extraarticular disorders.[9] The clinician should differentiate between a multitude of conditions such as: contusions, strains, athletic pubalgia, piriformis syndrome, hamstring syndrome, inflammatory disorders, snapping hip syndrome, bursitis, arthritis, septic arthritis, osteonecrosis, labral tears, fractures and dislocations and tumors.
Patients with OA complain about joint pain, stiffness, reduced movement and local inflammation. Further on in the development of this disorder, people can be confronted with joint contractures, muscle atrophy and limb deformity. Early in the development of OA, the pain comes in episodes, as it progresses, the pain becomes more constant, also with episodes of sharp pain. Morning stiffness and pain at night can also be a symptom of advanced hip osteoarthritis.[10]
The hip is stiff and rigid, there is an unpleasant tension and a higher resistance while moving. This is something that does not last long, after moving a little bit around the stiffness goes away. The range of motion decreases, this is because of the pain and the stiffness of the hip.When you start moving it will be better, but not as good as in the beginning. There can also be a crispy noise if the hip is moving.[11] [12]
Differential diagnosis[edit | edit source]
A thorough patient history and physical examination should aid a therapist in making his differential diagnosis. Patients will often come to the physiotherapist, complaining they have some pain issues. Pain location often gives a good indication whether it’s an intra-articular or extra-articular disorder.
Possible intra-articular hip disorders are: FAI ( Femoroacetabular impingement), Osteoarthritis, avascular necrosis, fractures (fig.3), dislocations, Septic arthritis, labral tear, chondral defect and an injury of ligamentum teres.
Possible extra-articular hip disorders are: abductor and gluteus muscle injuries, sciatica, obturator and LFC nerve irritation, piriformis syndrome, snapping hip, bursa, trochanteric bursitis, an inguinal ligament strain and a disorder of the joint capsule.[13]
Patients who probably have hip osteoarthritis have a constant pain and stiffness in the groin
region. This pain can be related to many causes, and doesn’t mean that every patient has arthritis. But the combination of groin pain and the limited movement and pain with internal rotation identifies people with this disorder. To make the diagnosis, radiography is usually done. If patients with osteoarthritis don’t have radiographic evidence, they often don’t receive a diagnosis of OA and don’t get the
treatment herefore.[10]
Diagnostic Procedures[edit | edit source]
Hip osteoarthritis can also be seen on radiographs. The visible findings of this disorder are joint space narrowing, marginal osteophytes, subchondral sclerosis, and bone cysts. Magnetic resonance imaging is more effective in detecting early change in the bone
structure, such as focal cartilage defects and bone marrow lesions in the subchondral bone.[5]
Outcome Measures[edit | edit source]
The first test was the hip disability and osteoarthritis outcome score (HOOS). This is a questionnaire which is used to gain the patients' history about their hip and associated problems, as well to evaluate symptoms and functional limitations related to the hip
during a therapeutic process. There are other questionnaires that can be used to get the patients opinion like Western Ontario and McMaster universities osteoarthritis index (WOMAC), the algofunctional index (AFI), the intermittent and constant osteoarthritis pain index (ICOAP), lequesne index, 6-minute walk test,timed up and go test and the patients specific complaints list (PSC).
The HOOS test judges functions and anatomical qualities combined with activities and participation. This is recommended when you are talking of hip disability with or without osteoarthritis. This test is meant to be used over short and long term intervals to view changes induced by treatment. It looks at the changes over a year time or at post traumatic osteoarthritis changes.
The HOOS questionnaire is a very simple test, which is user friendly and only takes 7-10
minutes to complete. The score consists of 40 items assessing 5 subscales: 5 separate patient-relevant dimensions: Pain (P), Symptoms (S), Activity limitations daily living (ADL), Function in sport and recreation (SP) and hip related quality of life (QOL). To interpret the score, the outcome measure is transformed in a worst to best scale from 0 to 100, with 100 indicating no symptoms and 0 indicating extreme symptoms. To calculate the total HOOS score the subscales need to be summed up, using following formula for all dimension: 100 – [(patient's score of the subscale x 100)/(total score of the subscale)]
This test has a high reliability , a good validity except for the floor and ceiling effects, a high responsiveness thanks to the addition of two subscales(SP and QOL).[35]
Medical management[edit | edit source]
Osteoarthritis is a common joint disorder, and the prevalence only increases with the aging of the population. This goes hand in hand with the increase of THR. THR, total hip replacement, is a successful orthopaedic procedure in the treatment of hip osteoarthritis, when the conservative therapy has failed. The number of total hip replacements per year increases by 73% overall. For those between 45 and 64 years, the total number of THR increases with 123% and 54% for people between 65 and 84 years old.
In THR, prosthetic substitutes replace the original hip joint partly or fully with the purpose to repair the hip joint. There is no age or weight limit in undergoing a total hip replacement, they have been performed successfully at all ages. But a hip replacement at higher age can result in a worse functional outcome, major technical difficulties and higher operative risks.
A good choice of implant and the right surgical technique are essential for a successful result.
A good focus on the patient is also very important, so all the elements that can have a bad impact on the result can be deleted.[14]
There are several techniques for implanting a prosthesis. In a study of Rosenlund et al, they investigated the difference in outcome in the two most commonly approaches of hip replacement: the lateral and posterior approach.[15] The lateral approach is set to have a reduced outcome in pain and physical function, and also in a decrease of strength of the adductor muscles. In a case-control study of Nilsdotter et al, the authors investigated the relevant outcomes of a patient after a total hip replacement, they were followed 3,6 years after the surgery.[16] 57% reported a WOMAC score less than 40 preoperatively, only 5,4% did this at the final follow-up. There was a significant increase in this score between the preoperatively measurement and the final one. 31% had an increased WOMAC score of less than 10 after 3,6 years for pain or function or function and pain. 40 patients reported a increase in WOMAC score of less than 20. The experimental group had a worse score than the reference group.
Examination[edit | edit source]
The beginning of OA is characterized by limited abduction and rotation in the hip joint. Later on flexion, extension, and adduction become more difficult.
Physiotherapeutic examination [18]
1) Palpation of M. gluteus medius.
Position: patient lies on his side. Upper leg in adduction and flexion
OA: Zone of greater Trochanter is sensitive and painful.
2)Flexion and forced flexion
Position: patient lies on his back. The physiotherapist lifted one leg to flexion. The knee is
in flexion so there is not too much muscle tension. The pelvis has to be at the same place.
OA: Flexion is limited for the final degrees.[19]
3) Extension
Position: 1. Patient stands in prone. Physiotherapist stabilizes the pelvis and raises the
leg. or 2. patient lies on his chest and lift the leg with flexion in the knee. You need a
flexion in the knee for a lower tension from the muscles
OA: Amplitude is limited.
4) Abduction
Position: Patient lies on his back. Physiotherapist stabilizes the pelvis and
performs abduction.
OA: abduction is limited and painful when the physiotherapist goes to the final degrees.
5) Adduction
Position: Patient lies on his back. The physiotherapist lift one leg and performs an
adduction with the other leg. The leg has to be in a normal position, no rotations.
OA: Keeps normal amplitude.[20][21]
Hip osteoarthritis can be diagnosed by a combination of the findings from a history and physical examination, so we don’t need to expose the patient to unnecessary radiation in an X-ray. The most used criteria in the diagnosis of hip osteoarthritis are those from the
American College of Rheumatology, which includes two sets of clinical features.[5]
Clinical Set A:
- Age: 50+
- Hip pain
- Hip internal rotation ≥ 15 degrees
- Pain with hip internal rotation
- Morning stiffness of the hip less than 60min
Clinical Set B:
- Age: 50+
- Hip pain
- Hip internal rotation < 15 degrees
Hip flexion ≤ 115 degrees
Later on, Sutlive et al. published a list of variables for detecting hip osteoarthritis in patients with unilateral hip pain. If there are 3 present variables out of the list of 5 variables, the chance of having OA is 68%. With 4 or 5 variables that are noticed, the
chance increases to 91%. The variables are positive when there’s pain or a limited range of motion in the tests.[12]
The five variables are:
- Flexion
- Internal rotation
- Scour test: external and internal rotation in abduction and adduction of the hip.
- Patrick’s or FABER test: flexion,abduction and external rotation of the hip.
- Hip flexion test
Physical Therapy Management[edit | edit source]
A systematic review by Bennel (2013) found that treatment goals should be made in cooperation between therapist and patient.[5] The therapy must be centered and applied around the patient. This way it suggests that the patients experience less anxiety to handle with the symptoms even though the condition may not always improve. The review states that patients using a self-management strategy have no difference in pain or function.[5]
Exercise Therapy[edit | edit source]
Currently the amount of research on exercise therapy for patients with hip osteoarthritis is limited and the effect of treatment is rather low. However, Bennel states that multiple trials and reviews suggest that exercise therapy might be an effective treatment strategy for hip osteoarthrosis.[5]
Below you can see a link to a summarised table with relevant studies using exercise therapy on land or in water (aquatherapy) and what they researched.
Table (from Bennell, K., “Physiotherapy management of hip osteoarthritis Journal of Physiotherapy”, Volume 59, Issue 3, September 2013, Pages 145–157.)
Exercises could be done in water as well, in order to facilitate recovery of the motorfuntion. In this situation, gravity is greatly reduced thus the burdensome weight and tension at the height of the effected joint will be reduced as well. Advice and education is important in treatment, tell the patient about their condition. Why does it occur? What's the treatment? What's the importance of exercise? This will make the patient have a clear understanding in his condition and will improve the healing process.However, it is unclear if aquatic exercises are more effective than exercises on land. There is also no clear evidence on balneotherapy. Currently, there doesn’t exist evidence that balneotherapy might be a beneficial therapy approach.[5][22][23][24]
Ultrasound therapy has been used across the globe in clinical practice, but as there is little evidence surrounding its use in the management of hip osteoarthritis, it is not recommended to use.[5]
Manual Therapy[edit | edit source]
A range of manual therapies is used as manual therapy treatment. These therapies are:[5]
- soft tissue techniques and stretches
- mobilisation of accessory and physiological movements
- manipulation/ mobilisation
The immediate effect of a mobilization intervention on elderly patients with osteoarthritis has been researched by Beselga et al (2016), they found that after an intervention pain decreased and that the range of motion in the hip joint improved. The study suggests that mobilization might reduce pain, might ‘provide a stretching effect on the joint capsules and muscles, thus restoring normal arthrokinematics or may induce pain inhibition and improved motor control’ and might reduce kinesiophobia.[24] However, these effects are currently not proven as studies regarding long-term effects are lacking. Further research for these effects is needed.[24]
“While there have been no reports of serious adverse events associated with the use of manual therapy in patients with hip osteoarthritis, therapists should advise patients about the possibility of self-limiting posttreatment soreness.”[5]
Resources[edit | edit source]
http://www.guidelines.gov/content.aspx?id=36893
https://www.ncbi.nlm.nih.gov/pubmed?otool=vublib
http://apps.webofknowledge.com.ezproxy.vub.ac.be:2048/WOS_GeneralSearch_input.do?product=WOS&search_mode=GeneralSearch&SID=U2HYlXJGBQdVzdFFDhX&preferencesSave d=
https://scholar.google.be/?inst=vub.ac.be
Clinical Bottom Line[edit | edit source]
Depending on the severity of the condition, managment will vary from patient to patient. It is important that the clinician individualizes treatment to each of their patients in order to ensure optimal outcomes.
References[edit | edit source]
- ↑ 1.0 1.1 Cooper C, Javaid MK, Arden N. Epidemiology of osteoarthritis. In: Atlas of Osteoarthritis. Tarporley: Springer Healthcare, 2014. p22.
- ↑ Cross M, Smith E, Hoy, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, Laslett LL, Jones G, Cicuttini F, Osborne R, Vos T, Buchbinder R, Woolf A, March L. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Annals of the Rheumatic Diseases 2014;73:1323-1330.
- ↑ 3.0 3.1 Nüesch E, Dieppe P, Reichenbach S, Williams S, Iff S, Jüni P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. Bmj 2011;342:1165.
- ↑ Reginister J-Y, Pelletier J-P, Martel-Pelletier J, Henrotin Y, editors. Osteoarthritis: Clinical and Experimental Aspects. Berlin: Springer, 1999.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Bennell K. Physiotherapy management of hip osteoarthritis. J Physiother. 2013; 59(3):145–157.
- ↑ Prieto-Alhambra D, Judge A, Javaid MK, Cooper C, Diez-Perez A, Arden NK. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: influences of age, gender and osteoarthritis affecting other joints. Annals of the rheumatic diseases. 2014;73(9):1659-1664.
- ↑ Murphy NJ, Eyles JP, Hunter DJ. Hip Osteoarthritis: Etiopathogenesis and Implications for Management. Advances in Therapy. 33.11 (2016): 1921–1946.
- ↑ 8.0 8.1 Book: CRIELAARD J.M., DEQUEKER J., FAMAEY J.P., FRANCHIMONG P., GRITTEN Ch., HUAUX J.P. et al. ‘Osteoartrose’. Brussel, België: drukkerij Lichtert; maart 1985.
- ↑ DeAngelis NA, Busconi BD. Assessment and differential diagnosis of the painful hip. Clinical Orthopaedics. 2003;406:11-18.
- ↑ 10.0 10.1 Kim C, Nevitt MC, Niu J, Clancy MM, Lane NE, Link TM et al. Association of Hip Pain with Radiographic Evidence of Hip Osteoarthritis: Diagnostic Test Study. BMJ. 2015 Dec 2;351:h5983.
- ↑ DeAngelis NA, Busconi BD. Assessment and differential diagnosis of the painful hip. Clinical Orthopaedics. 2003;406:11-18.
- ↑ 12.0 12.1 Sutlive TG, Lopez HP, Schnitker DE, Yawn SE, Halle RJ, Mansfield LT et al. Development of a Clinical Prediction Rule for Diagnosing Hip Osteoarthritis in Individuals With Unilateral Hip Pain. J Orthop Sports Phys Ther. 2008;38(9):542-50.
- ↑ Fernandez M, Wall P, O’Donnell J, Griffin D. Hip pain in young adults. Aust Fam Physician. 2014;43(4):205–9.
- ↑ Bottai V, Dell'Osso G, Celli F, Bugelli G, Cazzella N, Cei E et al. Total hip replacement in osteoarthritis: the role of bone metabolism and its complications. Clin Cases Miner Bone Metab. 2015 Sep-Dec;12(3):247-50.
- ↑ Rosenlund S, Broeng L, Jensen C, Holsgaard-Larsen A, Overgaard S. The effect of posterior and lateral approach on patient-reported outcome measures and physical function in patients with osteoarthritis, undergoing total hip replacement: a randomised controlled trial protocol. BMC Musculoskelet Disord. 2014;15:354.
- ↑ Nilsdotter AK, Petersson IF, Roos EM, Lohmander LS. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study. Ann Rheum Dis. 2003;62(10):923-30.
- ↑ Physiotutors. Cluster of Sutlive | Hip Osteoarthritis Diagnostic Cluster. Available from: https://www.youtube.com/watch?v=8xrDWgIUMO4
- ↑ CRIELAND, e.a., Osteoartrose, Lichtert, Brussel, 1985
- ↑ Bennell KL, Egerton T, Pua YH, Abbott JH, Sims K, Metcalf B et al. Efficacy of a multimodal physiotherapy treatment program for hip osteoarthritis: a randomised placebo-controlled trial protocol. BMC Musculoskelet Disord. 2010;11:238.
- ↑ Pisters MF, Veenhof C, Schellevis FG, De Bakker DH, Dekker J. Long-term effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a randomized controlled trial comparing two different physical therapy interventions. Osteoarthritis Cartilage. 2010;18(8):1019-26.
- ↑ Veenhof C, Köke AJ, Dekker J, Oostendorp RA, Bijlsma JW, van Tulder MW et al. Effectiveness of behavioral graded activity in patients with osteoarthritis of the hip and/or knee: A randomized clinical trial. Arthritis Rheum. 2006;55(6):925-34.
- ↑ Wright A, O'Hearn MA. Differential diagnosis and early management of rapidly progressing hip pain in a 59-year-old male. J Man Manip Ther. 2012;20(2):96-101.
- ↑ Verhagen AP, Cardoso JR, Bierma-Zeinstra SM. Aquatic exercise & balneotherapy in musculoskeletal conditions. Best Pract Res Clin Rheumatol. 2012;26(3):335-43.
- ↑ 24.0 24.1 24.2 Beselga C, Neto F, Alburquerque-Sendín F, Hall T, Oliveira-Campelo N. Immediate effects of hip mobilization with movement in patients with hip osteoarthritis: A randomised controlled trial. Man Ther. 2016;22:80-5.