Physical Activity in Adolescents with Haemophilia
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Caitlin MacRae, Hazel Burt, Alex Leishman, Chloe Allan, Kim Jackson, Steven flett, Rucha Gadgil, 127.0.0.1, Admin, Jane Hislop, Michelle Lee and Tarina van der Stockt
Introduction[edit | edit source]
Welcome to this online wiki resource which will focus on ‘The Role of a Physiotherapist in Promotion and Management of Physical Activity in Adolescents with Haemophilia.’ This wiki has been designed as learning resource for final year physiotherapy students and newly qualified physiotherapists. It is an online self-study module and should take approximately 10 hours to complete.
There are various treatments and concerns associated with paediatric haemophilia, the background will include a brief introduction to haemophilia and its medical management. As this resource will focus solely on the physiotherapists role in physical activity, aspects not directly related to the scope of this wiki may not be fully explained in detail. Therefore, any red hyperlinks will offer further information, should the reader require, when clicked on. Additionally, the learner will be orientated to further reading, should they wish to do so, throughout the module.
The Physiotherapists role in treating and managing adolescents with haemophilia is extremely important, and recent developments within the profession have increased its value (Buzzard and Beeton 2008). One of the key interventions involved in its treatment is promotion of physical activity (REF).
Definition of PE and how it is important in general pop as well as PWH
Although various studies have described the benefits of engaging in physical activity for PWH, results from research conducted in the USA among adolescent haemophilia patients have demonstrated a lack of knowledge concerning the role of physical activity in managing their condition (Nazzaro et al. 2006). This suggests that more work must be done to promote physical activity and emphasize its positive role in enhancing the lives of haemophilia sufferers (Negrier et al. 2013).
Physical activity promotion for health exists worldwide (Heath et al. 2012). The benefits of such in the general population are widely known, providing health improvements along with the potential for enhancing disease outcomes (WHO 2015). Although many studies have reported the benefits of participation in physical activity for PWH, researchers in the USA have identified a lack of knowledge among
young haemophilia patients (aged 13–18 years) as to the role of exercise in the management of their condition.
The promotion of exercise in children with haemophilia (CwH) is of particular importance due to recent advances in care over the past 40 years (Manco-Johnson et al. 2003). This has seen changes in exercise prescription; as is it now believed to be a crucial modality and understood it will not attribute to bleeds, as previously believed (REF).
As physiotherapists, we have an obligation and responsibility to actively promote physical activity in this population, as well as educating the individuals correctly in self-management of their life-long conditions, the intention being to maximize quality of life (REF).
The wiki is organised under three main sections, ‘Background of Haemophilia’, ‘Physiotherapist’s Role’ and ‘Benefits of Physical Activity’
Useful advice to be considered whilst undertaking the wiki: ensure you take regular screen breaks, complete all tasks, use further reading to expand knowledge and understanding, be aware of posture. (Insert pic of ideal posture)
Aims and Objectives[edit | edit source]
The aims of this wiki are as follows:
• To present a learning resource for final year physiotherapy students and newly qualified graduates which aims to develop their knowledge and understanding of the management of adolescents with haemophilia.
• To introduce final year physiotherapy students and newly qualified graduates to the skills, competencies and resources which can be utilised within their clinical practice in order to offer more effective and comprehensive management of adolescents with haemophilia.
Throughout this learning resource various tasks and activities have been encouraged to engage the learner. These have been developed considering different learning styles (VARK xxxx)
Learning Outcomes:
The following learning outcomes have been constructed using the levels determined by Bloom’s Taxonomy to facilitate learning development (Bloom et al. 1956).
Through completion of this learning module and related tasks, final year physiotherapy students and newly qualified physiotherapy graduates will be able to:
• Summarise the characteristics and underlying pathophysiology of haemophilia including explanation of different types.
• Critically reflect on the challenges and considerations associated with treating an adolescent with haemophilia.
• Using the biopsychosocial model, evaluate the physical, spiritual and emotional needs which must be considered when treating an adolescent with haemophilia.
• Critically appraise the evidence base surrounding physical activity in an adolescent with haemophilia.
Blooms Taxonomy, shown to the right, demonstrates a hierarchy of learning of which this wiki aims to encompass various levels of throughout. The identified learning aims have been constructed to suit this learning theory. (Insert pic of blooms taxonomy)
Background[edit | edit source]
Welcome to the background section of this wiki. This chapter will offer a brief understanding of haemophilia including pathophysiology, incidence and prevalence and medical management. The role of the MDT in treating an adolescent with this condition will also be briefly discussed. This chapter should take approximately __ to complete.
The learning outcomes to be addressed in this section are:
1. Summarise the characteristics and underlying pathophysiology of haemophilia including explanation of different types.
Definitions[edit | edit source]
Haemophilia is a rare inherited blood disorder where blood in the body has an inability to produce sufficient clotting factor, a protein in the blood which controls bleeding (NHS Choices 2015). This lack of clotting factor can lead to severe and prolonged bleeds within the joints which may cause permanent damage to both the joint and surrounding tissues (World Federation of Haemophilia 2015). The condition mainly affects boys and is carried genetically through a gene which is passed to child from parent through the X chromosome (Great Ormond Street Hospital 2015)
Symptoms of a bleed may include swollen and hot joints, described as a ‘funny feeling’ surrounding the joints, pain in the area and stiffness when mobilising the joint. This disorder mainly affects boys and it can affect any age group (The World Federation of Haemophilia 2015).
There are four main types of Haemophilia. These include:
• Haemophilia A
• Haemophilia B
• Haemophilia C
• Acquired Haemophilia
Haemophilia A is the most common type of Haemophilia. This is where someone either has low levels of clotting factor eight or is completely missing factor eight. This type of Haemophilia affects around 80% of the Haemophilia population (The Haemophilia Society 2015).
Haemophilia B is much less common and this is where clotting factor nine is either very low or is missing from the blood. This type of Haemophilia was first diagnosed in 1952. Around 20% off people with Haemophilia have Haemophilia B (The Haemophilia Society 2015).
Haemophilia C is ten times rarer than type A. AWH C will either have low levels of clotting factor eleven or this will be completed absent. Haemophilia C deficiency is different to A and B as it can present in both males and females. This is extremely uncommon and can only happen when the mother and father are both carriers of the gene (Haemophilia Information 2013). Haemophilia C does not cause joint bleeds but can lead to nose bleeds, bleeding in the mouth, heavy bleeding during periods for girls and prolonged external bleeding following injury (IHTC 2012).
Acquired Haemophilia is extremely rare. This type of Haemophilia is not inherited as it is an auto immune disorder. This is where the immune system attacks the clotting factors. This condition can affect males and females. (Grethlein 2014).
The most common type is haemophilia A which is a shortage of clotting factor 8. Haemophilia B is less common and the only difference is they lack in clotting factor 9.
The figure below shows how Haemophilia is passed on genetically:
GENETIC PICTURES
As shown above, when the female is the carrier of haemophilia and the father is unaffected, the son will possess a 50% chance of inheriting the condition. There is a 50% chance the daughter will be a carrier of the gene but will not inherit the condition (HFA 2015).
When the male suffers from haemophilia and the mother is unaffected, none of the sons will inherit the condition, all daughters will carry the gene but not be affected (HFA 2015).
If the father has haemophilia and the mother is a carrier, there will be a 25% chance that the daughter and son may have haemophilia. This is the only time where the girl can inherit the condition however this is extremely rare (Haemophilia information 2013).
Incidence and Prevalence[edit | edit source]
There are an estimated 6,000 people living in the United Kingdom with Haemophilia (NHS Choices 2015), most of which are male due to the way the condition is inherited.
Worldwide estimations suggest Haemophilia A is five times more prevalent than Haemophilia B; with statistics demonstrating of 1 in 10,000 boys will be diagnosed with Haemophilia A whereas out of 50,000 only one will suffer with Haemophilia B. (The Haemophilia Society 2015). Acquired Haemophilia affects 1-2 people in one million (Grethlein 2014).
Classifications and Severities[edit | edit source]
The table below catagorises the severities of haemophilia into mild, moderate and severe, detailing the percentage of sufferers in each category (Preston et al. 2004).
CLASSIFICATIONS TABLE
• When the father has haemophilia and the mother does not, none of the sons will have Haemophilia but all of the daughters will carry the Haemophilia gene
• When the mother is the carrier of Haemophilia but the father is not affected, there is a 50% chance the son will have Haemophilia and a 50% chance that a daughter will be a carrier.
• The only scenario that woman can be affected by Haemophilia is if their father has and their mother is a carrier however this is extremely uncommon.
Like other disorders, haemophilia can affect people to varying degrees. The symptoms can be mild, moderate or severe, depending on the level of clotting factor present (NHS Choices 2015).
For mild Haemophilia the individual will have between 4% - 49% of the factor level in their blood. Around 43-70% of the haemophilia population are considered mildly affected (Haemophilia Information 2013). Symptoms for mild haemophilia sufferers can be non-existent, although may include prolonged bleeding following serious injury, trauma or surgery. In many cases, haemophilia will not be discovered until there is excessive bleeding following injury or if they are undergoing surgery. In some cases it may not even be discovered until adulthood.
Moderate haemophilia sufferers have between 1% and 5% of factor level in their blood. Between 15-26% of AWH are considered moderate (Haemophilia Information 2013). Moderate sufferers are likely to suffer prolonged bleeding following injury and may have occasional spontaneous bleeding episodes.
Severe Haemophilia will affect an individual to a greater extent. Those with severe haemophilia will have a factor level between 0% and 1%. This accounts for the other 15-31% of the haemophilia population (National Haemophilia Foundation 2016).They will experience excessive bleeding after slight injuries and surgery and are also highly likely to have spontaneous bleeding episodes. They may also experience joint bleeding and prolonged bleeding into the muscles (Haemophilia Information 2013). This internal bleeding is particularly dangerous as suffers may be unaware it is occurring. If untreated it may lead to permanent joint deterioration and arthritis in years to come.
Medical Managment
[edit | edit source]
The medical management of Haemophilia typically involves two treatment methods, ‘on demand’ or prophylactic. Haemophilia Care (2014) explains how treatment involves replacing the deficient clotting factor (VIII for haemophilia A and IX for haemophilia B) through intravenous injection.
On demand treatment is administered immediately following a bleed and is most commonly used in mild or moderate cases. It provides the advantage of not having to infuse regularly, however if there is a delay in ‘on demand’ treatment following a bleed then there is potential for damage to occur.
Prophylactic is administered regularly as a method of preventative management and is most commonly used in those who suffer with severe haemophilia. The ultimate goal of prophylaxis treatment is to reduce the deficiency of factor VII or factor IX (Berntorp and Shapario 2012) therefore reducing the chance of spontaneous bleeds. It also aims to reduce the severity of the condition (Nilsson et al. 1976). Khoriaty et al. (2005) explains how clotting factors are infused by the patient themselves on a constant basis around three times a week in the case of severe haemophilia A (factor VIII), and twice a week in the case of severe haemophilia B (factor IX). The World Health Organisation recognises prophylaxis treatment as the optimal treatment for patients with severe haemophilia.
MDT Involvement
[edit | edit source]
Despite recent development in management of the condition, haemophilia sufferers still require comprehensive multidisciplinary care through all stages of their life (Breakey et al. 2010). A multidisciplinary team involves a range of professionals who collaborate together to structure a treatment plan for an individual, aiming to achieve high quality patient-centered care (Department of Health 2015). Physiotherapists have an extremely important role as a member of this team when treating AWH (REF). They will assist in ensuring there is a low risk of joint damage, work with parents, encourage light exercise, provide splints if necessary and introduce strengthening exercises (Great Ormond Street hospital, 2015). This includes taking a holistic approach considering the individual’s physical, social, emotional, cultural and spiritual needs (CSP 2015). The transition from childhood into adulthood causes additional stress for those with chronic disorders, which can be eased with a strong supporting team (Breakey et al. 2010). This may mean referring the patient to another team member to allow high quality treatment, specific to the patients needs. Professionals such as, GP’s, Occupational therapists and social workers all play an important role in a collaborative care team for adolescents with haemophilia.
Q&A[edit | edit source]
The Role of The Physiotherapist[edit | edit source]
Assessment[edit | edit source]
Management[edit | edit source]
Education[edit | edit source]
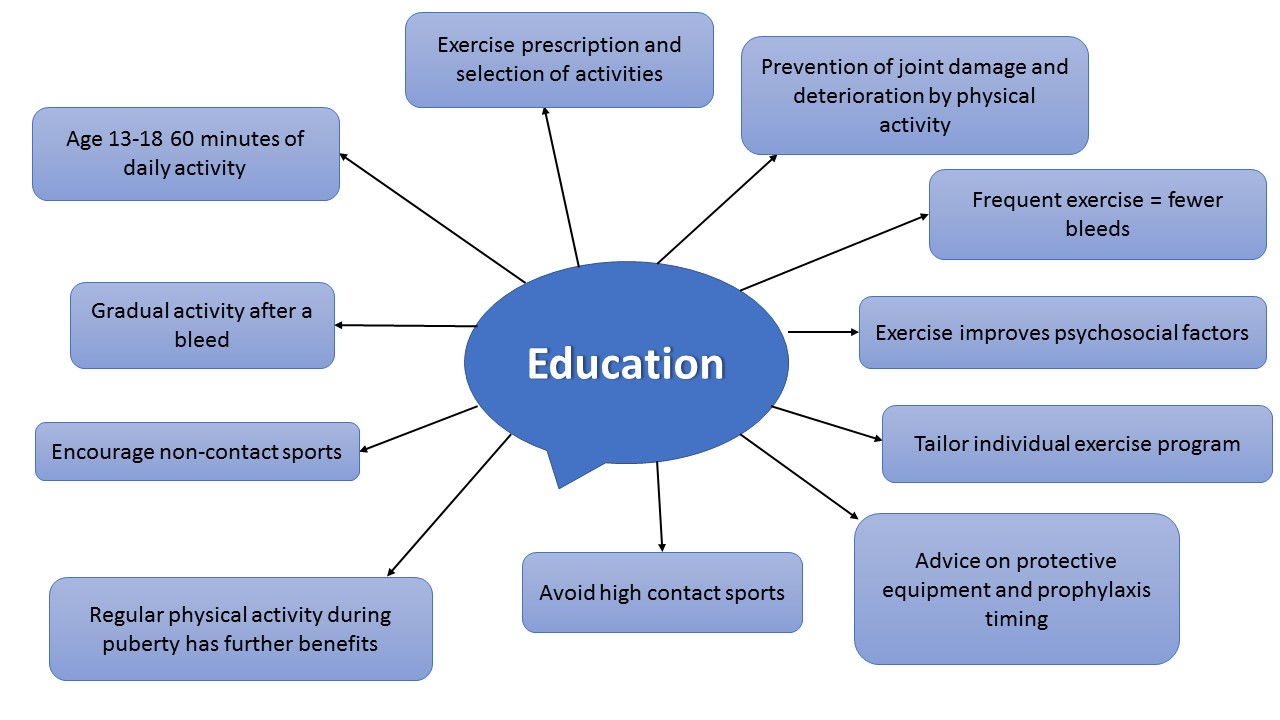
Below is a mind map which explains the advice that should be given to patients regarding physical activity. More detail on each is presented in the bullet points below.
The physiotherapist has a crucial role in educating patients regarding physical activity, exercise prescription and selecting particular activities (Heijnen 1993).
It is important to inform patients/relatives/peers that the benefits derived from physical activity can actually help to prevent joint damage and functional impairment (Buzzard 1997).
Individuals who exercise frequently actually exhibit fewer bleeds (Tinktinsky et al 2002).
You should inform patients that just as with healthy individuals, exercise also improves psychosocial factors (Negrier et al. 2008).
The physiotherapist should assist and advise patients on developing an individually tailored physical activity programme (Wittmeier and Mulder 2007).
You must educate the patients regarding protective equipment and timing of prophylaxis administration that is appropriate to their chosen sport or activity (McGee et al 2015; The World Federation of Hemophilia 2015).
The encouragement of the use of protective equipment (e.g. splints, braces) during activity especially if the patients has a target joint, or no clotting factor given prior to activity (Philpott et al. 2010).
Depending on the patients severity of their condition high contact and collision sports such as football, hockey, rugby, boxing, and wrestling are usually best avoided (The World Federation of Haemophilia 2015).
It is important to address the added benefits of physical activity during puberty in adolescents. Regular physical activity participation during puberty, enhances lean tissue mass, fitness and strength and decreases fat mass (Ara et al. 2004).
Physiotherapists should try to encourage non-contact sports such as swimming, walking, cycling, golf, archery, badminton, rowing and sailing (The World Federation of Haemophilia 2015).
It is paramount for physiotherapists to advise patients on the importance of gradually re-introducing activity after a bleed to minimise the chance of a re-ocurring bleed (The World Federation of Haemophilia 2015).
Give advice on appropriate forms of physical activity specific to that patient and their individual preferences, interests and needs (The World Federation of Hemophilia 2015).
Advice on amount of physical activity is no different to national guidelines for healthy individuals. Young people between the ages of 13-18 should participate in a minimum of 60 minutes of daily activity (Department of Health 2011).
It is advised that school personnel should be educated regarding suitable activities for the child, immediate care in case of a bleed, and modifications in activities that may be needed after bleeds (The World Federation of Hemophilia 2015).�
Physical Activity Promotion[edit | edit source]
Managing Risks and Considerations[edit | edit source]
PPE[edit | edit source]
How to Approach Conversations Regarding PA[edit | edit source]
Benefits of Physical Activity[edit | edit source]
Obesity[edit | edit source]
Childhood Development[edit | edit source]
Quality of Life[edit | edit source]
Policies and Guidelines[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.