Ankle-Brachial Index: Difference between revisions
Chloe Waller (talk | contribs) (Update video, results and interpretation) |
Chloe Waller (talk | contribs) (Updated evidence) |
||
| Line 97: | Line 97: | ||
|} | |} | ||
== | == Evidence == | ||
* | * A 2019 meta-analysis found sparse evidence for the validity of the ABI for diagnosing PAD in people with leg pain on exercise that is alleviated by rest.<ref>Crawford F, Welch K, Andras A, Chappell FM. [https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010680.pub2/full Ankle brachial index for the diagnosis of lower limb peripheral arterial disease]. Cochrane Database of Systematic Reviews 2016, Issue 9.</ref> | ||
* A 2019 systematic review deemed the inter- and intra-tester reliability of the ABI as acceptable, however, the authors note the validity of the included studies is undetermined. <ref>Casey S, Lanting S, Oldmeadow C, Chuter V. [https://pubmed.ncbi.nlm.nih.gov/31388357/ The reliability of the ankle brachial index: a systematic review.] J Foot Ankle Res. 2019 Aug 2;12:39. </ref> | |||
* The ABI does not measure limb microvascular perfusion, which is believed to be a main cause of PAD symptoms and tissue injury.<ref>Davidson BP, Hodovan J, Mason OR, Moccetti F, Gupta A, Muller M, Belcik JT, Annex BH, Lindner JR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6732010/ Limb Perfusion During Exercise Assessed by Contrast Ultrasound Varies According to Symptom Severity in Patients with Peripheral Artery Disease]. J Am Soc Echocardiogr. 2019 Sep;32(9):1086-1094.e3.</ref> This study supports the use of contrast-enhanced ultrasound alongside the ABI. | |||
* One study of 201 patients found oscillometric ABI showed good accuracy of PAD diagnosis, however, the authors noted high incidence of oscillometric errors and difficulties with interpreting the readings.<ref>Hageman D, van den Houten MML, Pesser N, Gommans LNM, Scheltinga MRM, Teijink JAW. [https://pubmed.ncbi.nlm.nih.gov/32682067/ Diagnostic accuracy of automated oscillometric determination of the ankle-brachial index in peripheral artery disease.] J Vasc Surg. 2021 Feb;73(2):652-660.</ref> | |||
* | |||
== Resources == | == Resources == | ||
Revision as of 13:05, 13 September 2022
Original Editor - Khloud Shreif
Top Contributors - Khloud Shreif, Chloe Waller, Vidya Acharya and Lucinda hampton
Introduction[edit | edit source]
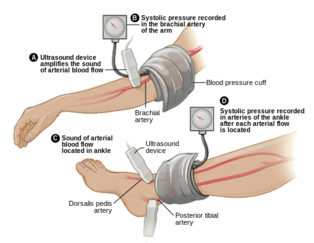
The ankle-brachial index (ABI) is a quick, non-invasive technique used to check vascular status and for peripheral arterial disease (PAD)[1][2]. It was first described by Winsor in 1950[3].
The ABI is the ratio between the systolic blood pressure of the lower limb (specifically at the ankle) and the upper limb, to assess for narrowing or blockages in the arteries in the legs[1][4].
Indications[edit | edit source]
Symptoms of peripheral artery disease:
- Intermittent claudication or cramping pain in the legs.[5]
- Wounds on the legs that are slow to heal.[6]
- Leg that feels colder than other parts of the body or is a different shade of color. [6]
Those with risk factors for PAD, such as:[4]
- History of tobacco use
- Restricted blood flow (atherosclerosis) in other parts of your body.
- History of stroke or transient ischemic attack.
- Family history of heart disease.
- Over 70 years of age. [5]
Contraindications[edit | edit source]
- Patients with confirmed or suspected DVT, because of the possibility of breaking of the thrombus.
- Severe leg pain.[5]
Procedures[edit | edit source]
Tools[5][edit | edit source]
- Doppler
- Blood pressure monitor.
- Pressure cuffs
Preparation[edit | edit source]
- Rest for 10-20 minutes prior to the test.
- Wear loose, comfortable clothing.
- Avoid nicotine/ smoking for 2 hours prior to the test.
- Supported, comfortable supine position.
Technique[7][edit | edit source]
- Place the cuff around the patient's arm, use the doppler and press against the skin at the level of the brachial artery in the arm. Inflate the cuff to about 20 mmHg above the last audible pulse. The Doppler signal should disappear. Then slowly deflate the cuff, approximately 1 mmHg/sec. When the Doppler signal re-appears, the pressure of the cuff is equal to the brachial systolic pressure. Record the brachial systolic pressure.
- Place the cuff around the lower leg and locate two arteries:
- Dorsalis pedis, which is a branch from the anterior tibial artery, it is located between the tibialis anterior and extensor hallucis longus
- Posterior tibial artery, that is behind the medial malleolus.
- Repeat the same technique as the arm to record the dorsalis pedis and posterior tibial arterty: using the doppler to locate the signal, inflating the cuff and then deflating until the signal re-appears.
- The ABI value is calculated by taking the higher pressure of the 2 arteries at the ankle, divided by the brachial arterial systolic pressure.
- Repeat the ankle measurement for the other leg in order to calculate its ABI.
Demonstration video:
Results and Interpretation[7][edit | edit source]
| ABI value | Interpretation | Recommendation |
|---|---|---|
| <0.5 | Severe arterial disease | Refer to vascular specialist |
| 0.5-0.8 | Moderate arterial disease | Refer to vascular specialist |
| 0.8-0.9 | Mild arterial disease | Treat risk factors |
| 0.9-1 | Acceptable | None |
| 1-1.4 | Normal range | None |
| >1.4 | Calcification of vessels | Refer to vascular specialist |
Evidence[edit | edit source]
- A 2019 meta-analysis found sparse evidence for the validity of the ABI for diagnosing PAD in people with leg pain on exercise that is alleviated by rest.[9]
- A 2019 systematic review deemed the inter- and intra-tester reliability of the ABI as acceptable, however, the authors note the validity of the included studies is undetermined. [10]
- The ABI does not measure limb microvascular perfusion, which is believed to be a main cause of PAD symptoms and tissue injury.[11] This study supports the use of contrast-enhanced ultrasound alongside the ABI.
- One study of 201 patients found oscillometric ABI showed good accuracy of PAD diagnosis, however, the authors noted high incidence of oscillometric errors and difficulties with interpreting the readings.[12]
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 McClary KN, Massey P. Ankle Brachial Index. 2022 Jan 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–
- ↑ Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, Fowkes FG, Hiatt WR, Jönsson B, Lacroix P, Marin B. Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation. 2012 Dec 11;126(24):2890-909.
- ↑ Winsor, T. Influence of arterial disease on the systolic blood pressure gradients of the extremity. Am J Med Sci. 1950 Aug;220(2):117-26.
- ↑ 4.0 4.1 Mayo Clinic.Ankle Brachial Index. Available from:https://www.mayoclinic.org/tests-procedures/ankle-brachial-index/about/pac-20392934 (Last accessed 12/09/2022)
- ↑ 5.0 5.1 5.2 5.3 Ankle Brachial Index: Quick Reference Guide for Clinicians. Journal of Wound, Ostomy and Continence Nursing: March/April 2012 - Volume 39 - Issue 2S - p S21-S29
- ↑ 6.0 6.1 Harvard Health Publishing. Ankle-brachial index. Available from: https://www.health.harvard.edu/newsletter_article/ankle-brachial-index (Last accessed 12/09/2022).
- ↑ 7.0 7.1 Stanford Medicine. Introduction to Measuring the Ankle Brachial Index. Availble from: https://stanfordmedicine25.stanford.edu/the25/ankle-brachial-index.html#:~:text=The%20ABI%20is%20performed%20by,or%2010%2DmHz%20Doppler%20instrument. (Last accessed 13/09/2022)
- ↑ St Michael's Hospital. How to perform an ankle brachial index. Available from https://www.youtube.com/watch?v=0_0VlLSTAAE (Last accessed 13/09/2022)
- ↑ Crawford F, Welch K, Andras A, Chappell FM. Ankle brachial index for the diagnosis of lower limb peripheral arterial disease. Cochrane Database of Systematic Reviews 2016, Issue 9.
- ↑ Casey S, Lanting S, Oldmeadow C, Chuter V. The reliability of the ankle brachial index: a systematic review. J Foot Ankle Res. 2019 Aug 2;12:39.
- ↑ Davidson BP, Hodovan J, Mason OR, Moccetti F, Gupta A, Muller M, Belcik JT, Annex BH, Lindner JR. Limb Perfusion During Exercise Assessed by Contrast Ultrasound Varies According to Symptom Severity in Patients with Peripheral Artery Disease. J Am Soc Echocardiogr. 2019 Sep;32(9):1086-1094.e3.
- ↑ Hageman D, van den Houten MML, Pesser N, Gommans LNM, Scheltinga MRM, Teijink JAW. Diagnostic accuracy of automated oscillometric determination of the ankle-brachial index in peripheral artery disease. J Vasc Surg. 2021 Feb;73(2):652-660.