Parsonage-Turner Syndrome: Case Study: Difference between revisions
No edit summary |
No edit summary |
||
| Line 19: | Line 19: | ||
== Background == | == Background == | ||
A 13-year-old right-handed African-American reported injuring his right shoulder while doing a push up in gym class. At that time he had substantial pain and for a couple of days was unable to use his right upper extremity. When his parent observed he wasn't using his right upper extremity normally, she sought the services of the primary care physician. Based on the reported mechanism of injury and the amount of laxity, the patient was referred for an orthopaedic consult. He was referred | A 13-year-old right-handed African-American reported injuring his right shoulder while doing a push up in gym class. At that time he had substantial pain and for a couple of days was unable to use his right upper extremity. When his parent observed he wasn't using his right upper extremity normally, she sought the services of the primary care physician. Based on the reported mechanism of injury and the amount of laxity, the patient was referred for an orthopaedic consult. He was referred for physical therapy services due to right shoulder laxity. | ||
== Client Characteristics == | == Client Characteristics == | ||
| Line 25: | Line 25: | ||
== Examination Findings == | == Examination Findings == | ||
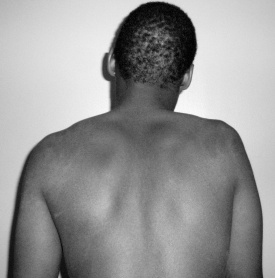
Upon palpating his shoulder, I immediately knew something was not normal. This patient's shoulder didn't feel as would be expected. I asked the patient to disrobe so I could better have a better understanding of what I was palpating. It seemed that my fingers could easily sink to the humerus on his involved side. After he disrobed, this is what I observed. | Upon palpating his shoulder, I immediately knew something was not normal. This patient's shoulder didn't feel as would be expected. I asked the patient to disrobe so I could better have a better understanding of what I was palpating. It seemed that my fingers could easily sink to the humerus on his involved side. After he disrobed, this is what I observed. He had substantial atrophy of his right shoulder muscles. | ||
[[File:2-6-2009 posterior.jpg|left|thumb|278x278px]] [[File:2-6-2009 Anterior.jpg|none|thumb|316x316px]] | [[File:2-6-2009 posterior.jpg|left|thumb|278x278px]] [[File:2-6-2009 Anterior.jpg|none|thumb|316x316px]] | ||
He demonstrated poor ability to elevate the right shoulder. Actively, he was only able to demonstrate approximately 140 degrees of flexion and 120 degrees of abduction. Measuring the active motion proved to be difficult due to compensatory patterns and fatigue. Multiple repetitions of assessment led to less elevation and more compensatory patterns. He reported no pain with active range of motion. | He demonstrated poor ability to elevate the right shoulder. Actively, he was only able to demonstrate approximately 140 degrees of flexion and 120 degrees of abduction on his first attempt. Measuring the active motion proved to be difficult due to compensatory patterns and fatigue. Multiple repetitions of assessment led to less elevation and more compensatory patterns. He reported no pain with active range of motion. | ||
Here is a video of what was observed when assessing active range of motion: | Here is a video of what was observed when assessing active range of motion: | ||
| Line 44: | Line 44: | ||
The patient was basically on hold with physical therapy services for 4 weeks as he progressed through the medical system due to the need for differential diagnosis. I was unsure how to proceed without a reasonable diagnosis that could help with determining physical therapy interventions and progressing the patient to have optimal outcomes. | The patient was basically on hold with physical therapy services for 4 weeks as he progressed through the medical system due to the need for differential diagnosis. I was unsure how to proceed without a reasonable diagnosis that could help with determining physical therapy interventions and progressing the patient to have optimal outcomes. | ||
== Resuming Physical Therapy Services == | |||
Parent contacted me 2 weeks after | |||
The patient returned for physical therapy services 4 weeks later with a more specific diagnosis. Electromyography indicated that the patient had neuralgic amytrophy (NA), also known as Parsonage-Turner Syndrome or brachial plexus neuropathy. The working diagnosis of NA seemed consistent with the initial presentation. Although he had not received any physical therapy services or advice during the 4 weeks, he showed improvement in his presentation. | |||
He continued to have atrophy but the right upper extremity muscles were beginning to have more definition. | |||
[[File:2-24-2009 posterior.jpg|left|thumb]] | |||
[[File:2-24-2009 Anterior.jpg|center|thumb]] | |||
Active range of motion of the right shoulder improved to 160 degrees of flexion and 180 degrees of abduction. He was actually able to perform 1 set of 6 repetitions of full abduction before he exhibited fatigue and compensatory movement. Right grip strength assessed by the hand dynamometer had improved to an average of 66.67 pounds. | |||
== Intervention == | == Intervention == | ||
Revision as of 18:28, 3 March 2018
Original Editor - Selena Horner
Top Contributors -
Introduction[edit | edit source]
This will be the first case report to highlight clinical thinking and rationale combined with the progression and results of physical therapy treatment for a 13 year old with Parsonage-Turner Syndrome.
A 13-year-old African-American male initiated physical therapy services after a referral from an orthopaedic surgeon due to right shoulder instability. Upon subsequent physical examination by a physical therapist, the combination of significant strength deficits, substantial atrophy and no pain complaints led to further questioning. The young patient reported severe right shoulder pain approximately 4 weeks prior to the visit and contributed the symptoms to attempting to perform a push up in gym class. Upon further questioning, his parent reported an upper respiratory infection and severe neck pain approximately 4 weeks prior to the push up incident. Neither the current presentation nor the reported history were consistent with typical shoulder instability. The physical therapist recommended a referral to a physiatrist for further diagnostic testing. Electromyography and nerve conduction studies indicated neuralgic amyotrophy.
Keywords: Neuralgic Amyotrophy, Brachial Plexus Neuropathy, Parsonage-Turner Syndrome
Neuralgic amytrophy (NA), also known as Parsonage-Turner Syndrome or brachial plexus neuropathy, is quite rare with an annual incidence rate from 1 to 3 cases per 100,000 population.1,2 Onset age is usually in the 2nd or 3rd decade, but can have a range from neonatal to the 7th decade.
Because of the typical presentation, most patients with NA are initially diagnosed with a shoulder type pathology or cervical radiculopathy. Patients with NA generally seek services from their primary care physician. Due to the initial presentation, it is highly likely patients with NA are then referred to physical therapists or at times to neurologists and/or orthopedic surgeons.3
Although patients with NA are referred to physical therapists, literature is substantially lacking in what physical therapy interventions are beneficial. The majority of literature focuses on diagnosis and etiology. [references] Lack of anticipated progression is found within current published literature. This will be the first case report to highlight clinical thinking and rationale combined with the progression and results of physical therapy treatment.
Background[edit | edit source]
A 13-year-old right-handed African-American reported injuring his right shoulder while doing a push up in gym class. At that time he had substantial pain and for a couple of days was unable to use his right upper extremity. When his parent observed he wasn't using his right upper extremity normally, she sought the services of the primary care physician. Based on the reported mechanism of injury and the amount of laxity, the patient was referred for an orthopaedic consult. He was referred for physical therapy services due to right shoulder laxity.
Client Characteristics[edit | edit source]
The adolescent denied pain and numbness or tingling. He reported a 50% deficit in function. The PF-10 score was 70/100.
Examination Findings[edit | edit source]
Upon palpating his shoulder, I immediately knew something was not normal. This patient's shoulder didn't feel as would be expected. I asked the patient to disrobe so I could better have a better understanding of what I was palpating. It seemed that my fingers could easily sink to the humerus on his involved side. After he disrobed, this is what I observed. He had substantial atrophy of his right shoulder muscles.
He demonstrated poor ability to elevate the right shoulder. Actively, he was only able to demonstrate approximately 140 degrees of flexion and 120 degrees of abduction on his first attempt. Measuring the active motion proved to be difficult due to compensatory patterns and fatigue. Multiple repetitions of assessment led to less elevation and more compensatory patterns. He reported no pain with active range of motion.
Here is a video of what was observed when assessing active range of motion:
Passively, in the supine position, he had normal, pain free range of motion of the involved shoulder (right). Grip strength assessed performing 3 trials with a hand dynamometer indicated a grip strength of an average of 79 pounds on the non-dominant non-involved side and 50 pounds on the dominant involved side.
Critical Thinking and Decision-Making Process[edit | edit source]
Based on the preliminary findings, the atypical presentation did not match what would be expected with joint laxity. I questioned the parent for additional information. The parent denied any recent immunization(s) or any recent antibiotics. The family had not been on vacation or out of the country. The parent confirmed that 4 weeks prior to the push up scenario her son had an episode of extreme neck pain, swollen lymph nodes and an upper respiratory infection. She said those symptoms seemed to resolve within a few days. Unfortunately, the familial history for the adolescent was unknown because he was adopted.
Because the patient was adopted, I had no familial history to help me determine if his presentation was the result of some type of progressive muscular type of disease process or a peripheral nerve injury.
I recommended the adolescent have a consult with a physiatrist. I needed further diagnostic testing to help determine if some type of peripheral nerve damage was due to a viral infection or if there was some genetic reason for the significant amount of muscle atrophy.
The patient was basically on hold with physical therapy services for 4 weeks as he progressed through the medical system due to the need for differential diagnosis. I was unsure how to proceed without a reasonable diagnosis that could help with determining physical therapy interventions and progressing the patient to have optimal outcomes.
Resuming Physical Therapy Services[edit | edit source]
Parent contacted me 2 weeks after
The patient returned for physical therapy services 4 weeks later with a more specific diagnosis. Electromyography indicated that the patient had neuralgic amytrophy (NA), also known as Parsonage-Turner Syndrome or brachial plexus neuropathy. The working diagnosis of NA seemed consistent with the initial presentation. Although he had not received any physical therapy services or advice during the 4 weeks, he showed improvement in his presentation.
He continued to have atrophy but the right upper extremity muscles were beginning to have more definition.
Active range of motion of the right shoulder improved to 160 degrees of flexion and 180 degrees of abduction. He was actually able to perform 1 set of 6 repetitions of full abduction before he exhibited fatigue and compensatory movement. Right grip strength assessed by the hand dynamometer had improved to an average of 66.67 pounds.