Hip Osteoarthritis: Difference between revisions
No edit summary |
No edit summary |
||
| (175 intermediate revisions by 22 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original | '''Original Editor '''- [[User:Eric Robertson|Eric Robertson]], [[User:Kim Presiaux|Kim Presiaux]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
== Introduction == | |||
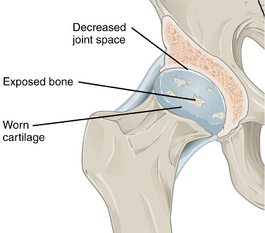
[[File:Hip OA diagram.png|thumb|265x265px|Hip OA diagram|alt=]] | |||
Osteoarthritis is a common disabling condition that causes joint pain and stiffness caused by the gradual erosion of cartilage. Hip osteoarthritis is a common form of osteoarthritis that causes restricted locomotor activity and functional disability, and may progress to the point where joint replacement is needed. Hip osteoarthritis is a major global public-health burden. <ref name=":2" /> | |||
* For people with hip arthritis, physiotherapy may assist in conditioning and obtaining endurance of the surrounding muscles that support the joint. | |||
* A long term approach to the management of a hip OA should include some type of regular physical therapy or conditioning program. | |||
== Epidemiology == | |||
Globally, from 1990 to 2019, the age-standardized incidence rate of hip osteoarthritis increased from 17.02 per 100,000 persons to 18.70 per 100,000 persons. The burden of hip osteoarthritis has increased in almost all countries over the past 30 years, this increasing trend is expected to continue, due to the rapid aging of the world’s population. | |||
* Osteoarthritis is the most common cause of hip pain in older adults (older than 50 years of age). | |||
</ | * Prevalence rates for adult hip OA range from 0.4% to 27%. | ||
< | * The reported prevalence of hip OA shows great variability, with men showing higher prevalence of radiographic hip OA.<ref name=":2">Fu M, Zhou H, Li Y, Jin H, Liu X. Global, regional, and national burdens of hip osteoarthritis from 1990 to 2019: estimates from the 2019 Global Burden of Disease Study. Arthritis research & therapy. 2022 Dec;24(1):1-1.Available;https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-021-02705-6#Sec9 (accessed 15.11.2022)</ref><ref name=":3">Cibulka MT, Bloom NJ, Enseki KR, MacDonald CW, Woehrle J, McDonough CM. Hip pain and mobility deficits—hip osteoarthritis: revision 2017: clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy. 2017 Jun;47(6):A1-37.Available:https://www.jospt.org/doi/10.2519/jospt.2017.0301 (accessed 15.11.2022)</ref> | ||
* Lifetime risk for symptomatic hip OA is 18.5% for men and 28.6% for women<ref name=":8">Lespasio MJ, Sultan AA, Piuzzi NS, Khlopas A, Husni ME, Muschler GF, Mont MA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5760056/ Hip osteoarthritis: a primer.] The Permanente Journal. 2018;22. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5760056/ (last accessed 19.11.2019)</ref>. | |||
* Research suggest that there are a 25% risk of developing hip osteoarthritis for people who live to the age of 85,<ref name=":0">Murphy NJ, Eyles JP, Hunter DJ. [https://link.springer.com/article/10.1007/s12325-016-0409-3 Hip osteoarthritis: Etiopathogenesis and implications for management.] Advances in therapy 2016;33(11):1921-46.</ref> | |||
== Pathology == | |||
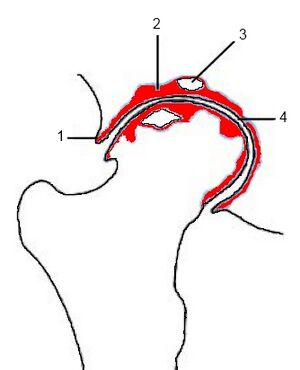
[[File:Hip OA schematic.jpeg|thumb|Severe OA 1. osteophytes 2. subchondral thickening 3. cyst 4. jt space narrowing|alt=]]Osteoarthritis is distinguished by an active progressive alteration of the whole synovial joint, being due to a combination of mechanical, inflammatory and metabolic factors. It is caused by an imbalance between the destruction and repair of the affected tissues. The disease affects the | |||
* Hyaline cartilage: loses its structural integrity due to composition changes. | |||
* Subchondral bone | |||
* Joint capsule | |||
* Synovium | |||
* Ligaments and the periarticular muscles. | |||
== Risk Factors == | |||
Risk factors that increase the likelihood of developing osteoarthritis of the hip are | |||
* [[Older People - An Introduction|Older age]] | |||
</ | * [[Obesity]] | ||
* [[Genetics and Health|Genetics]] | |||
* Repetitive stress and mechanical overload | |||
* Farmers, construction workers | |||
* High impact sports eg football, handball, hockey, wrestling, weight-lifting, and long-distance running | |||
* [[Hip Dysplasia|Acetabular dysplasia]] | |||
* [[Femoroacetabular Impingement|Femoroacetabular impingement]] | |||
* [[Slipped Capital Femoral Epiphysis|Slipped capital femoral epiphysis]] | |||
* [[Legg-Calve-Perthes Disease|Perthes disease]] | |||
* Trauma, e.g. [[Hip Dislocation|hip dislocation]] or [[Femoral Neck Hip Fracture|hip fracture]]<ref>Radiopedia Hip OA Available:https://radiopaedia.org/articles/osteoarthritis-of-the-hip (accessed 15.11.2022)</ref> | |||
== | == Diagnosis == | ||
[[File:Hip OA.jpg|250x250px|alt=|thumb|Advanced OA of a hip. ]]The following criteria should be used to classify adults over the age of 50 with hip OA: | |||
# Moderate anterior or lateral hip pain during weight-bearing activities | |||
# Morning stiffness less than 1 hour in duration after wakening | |||
# Hip internal rotation range of motion less than 24° or internal rotation and hip flexion 15° less than the nonpainful side, and/or increased hip pain associated with passive hip internal rotation.<ref name=":3" /> | |||
= | Radiographic evidence: joint space narrowing, marginal osteophytes, subchondral sclerosis, and bone cysts.<ref>Brandt CD. Diagnosis and non-surgical management of osteoarthritis. USA: Professional Communications, Inc. 2010.</ref><ref name=":7">Katz JN, Arant KR, Loeser RF. [https://jamanetwork.com/journals/jama/article-abstract/2776205 Diagnosis and treatment of hip and knee osteoarthritis: a review.] Jama. 2021 Feb 9;325(6):568-78. Available: https://jamanetwork.com/journals/jama/article-abstract/2776205<nowiki/>(accessed 23.1.2022)</ref>. | ||
[[ | == Clinical Presentation == | ||
[[File:Walking stick.jpeg|thumb|Hip OA - Elderly lady]]Pain characteristics: | |||
* Slowly progressive [[Hip Pain and Mobility Deficits|hip pain]], or hip-related groin pain radiating into the thigh, buttocks or knee. | |||
* The [[Pain Behaviours|pain]] can be worse at night, at rest or with strenuous activity, reducing the [[Range of Motion|range of motion]] and limiting walking distance. It can be associated with stiffness particular in the morning or after rest. | |||
Other symptoms include locking, grinding and joint instability, fatigue and pain-related psychological [[Stress and Health|stress]].<ref name=":6">Radiopedia OA of the hip Available: https://radiopaedia.org/articles/osteoarthritis-of-the-hip?lang=us<nowiki/>(accessed 23.1.2022)</ref> | |||
=== Physical Examination === | |||
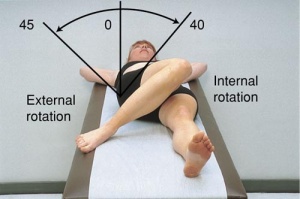
[[File:Hip rotation rom.jpeg|thumb|Measuring ROM hip]] | |||
A physical examination includes (Also also [[Hip Examination|hip examination]]) | |||
* Observation | |||
* Subjective interview: | |||
** Complaints of pain, deformity, stiffness and/or limp | |||
** Previous history linked to hip pain (congenital or childhood problems, previous trauma) | |||
* Physical examination in Standing and Supine (look for [[Leg Length Discrepancy|leg length discrepancy]], [[Gait: Antalgic|antalgic gait]] and [[Trendelenburg Test|Trendelenberg gait)]] | |||
* Objective observation (posture, deformities, muscle atrophy) | |||
* Palpation: | |||
** Tenderness at the hip | |||
** Pain and sensitivity over greater trochanter | |||
* Range of motion: | |||
** Early signs of hip osteoarthritis is limited abduction and rotation. As the disease progresses, flexion, extension and adduction becomes more difficult. | |||
** Normally painful at end of available range of motion | |||
* Crepitis with movement<ref name=":9">American Academy of Orthopaedic Surgeons. Diseases and conditions: Osteoarthritis of the hip.https://orthoinfo.aaos.org/en/diseases--conditions/osteoarthritis-of-the-hip (accessed 14/07/2018).</ref><ref name=":5">Crielaard JM, Dequeker J, Famaey JP, Franchimong P, Gritten CH., Huaux JP. Osteoartrose. Brussels: Drukkerij Lichtert, 1985.</ref><ref name=":10">Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.</ref> | |||
Five variables for detecting hip osteoarthritis are: | |||
# Self-reported squatting as an aggravating factor | |||
# Active hip flexion causing lateral hip pain | |||
# [[Hip Quadrant Test|Hip Quadrant test]] with adduction causing lateral hip or groin pain | |||
# Active hip extension causing pain | |||
# Passive internal rotation of less than or equal to 25° | |||
If there are 3/5 variables present, the chance of having OA is 68%. With 4-5/5 the chance increases to 91%. The variables are positive when there’s pain or a limited range of motion in the tests.<ref>Sutlive TG, Lopez HP, Schnitker DE, Yawn SE, Halle RJ, Mansfield LT et al. [https://www.jospt.org/doi/pdfplus/10.2519/jospt.2008.2753 Development of a clinical prediction rule for diagnosing hip osteoarthritis in individuals with unilateral hip pain.] J Orthop Sports Phys Ther. 2008;38(9):542-50.</ref> | |||
== Management == | |||
A [[Biopsychosocial Model|biopsychosocial approach]] offers the best outcome.<ref name=":1" /> A multidisciplinary team may be involved including: doctors, physiotherapists, dietitians, and occupational therapists. | |||
Management of hip osteoarthritis varies according to the severity of the condition. A combination of pharmaceutical and non-pharmaceutical modalities is recommended for the optimal management of the condition. Physiotherapy plays an important role in customized exercise programmes for patients living with hip osteoarthritis. | |||
== | # OA management includes patient education combined with exercise and/or manual therapy. Education should include teaching activity modification, exercise <ref>Dalmas I, Agius TP, Sciriha A. Core muscle strengthening exercises in the management of hip osteoarthritis: outcomes of a 12-week programme. European Journal of Physiotherapy. 2023 Mar 27:1-8.</ref>, supporting weight reduction when overweight (see below), and methods of unloading the arthritic joints. | ||
# Management includes providing impairment-based functional, gait, and balance training, including the proper use of assistive devices (canes, crutches, walkers), to patients with hip osteoarthritis and activity limitations, balance impairment, and/or gait limitations when associated problems are observed.<ref name=":3" /> | |||
# Offer topical or oral [[NSAIDs|nonsteroidal anti-inflammatory drugs]] in those without contraindications. | |||
# Intra-articular steroid injections provide short-term pain relief and duloxetine has demonstrated efficacy. Opiates should be avoided.<ref name=":7" /> | |||
= | '''Weight management''' – Hip OA<ref name=":12">2018 RACGP [https://www.racgp.org.au/download/Documents/Guidelines/Musculoskeletal/guideline-for-the-management-of-knee-and-hip-oa-2nd-edition.pdf Guidelines for hip and knee arthritis] Available from: https://www.racgp.org.au/download/Documents/Guidelines/Musculoskeletal/guideline-for-the-management-of-knee-and-hip-oa-2nd-edition.pdf (last accessed 19.11.2019)</ref>(RACPG 2018 guidelines): We strongly recommend weight management for people with hip OA. For those who are overweight ([[Body Mass Index|body mass index]] [BMI] ≥25 kg/m2 ) or obese (BMI ≥30 kg/m2 ), a minimum weight loss target of 5–7.5% of body weight is recommended. It is beneficial to achieve a greater amount of weight loss given that a relationship exists between the amount of weight loss and symptomatic benefits. Weight loss should be combined with exercise for greater benefits. For people of healthy body weight, education about the importance of maintaining healthy body weight is essential. | ||
'''Surgical interventions:''' [[Total Hip Replacement|Total hip replacement]] - The option in patients with symptomatic and radiographic osteoarthritis characterized by refractory pain and disability; [[Osteotomy]] and hip resurfacing - Should be considered in younger patients with symptomatic secondary osteoarthritis due to acetabular dysplasia, femoroacetabular impingement, varus or valgus deformity<ref name=":6" />. | |||
== Physiotherapy Management == | |||
Physiotherapy plays in major role in the management of patients with hip osteoarthritis. The goal is to improve strength, mobility and increase range of motion. Physiotherapy also helps relieve pain and restores normal movement in the hip and legs and also addresses pain management and functional adaptions. Patient-specific exercise programmes has shown to decrease pain and improve function in hip osteoarthritis.<ref name=":0" /><ref name=":1">Bennell K. [https://pubmed.ncbi.nlm.nih.gov/23896330/ Physiotherapy management of hip osteoarthritis]. J Physiother. 2013; 59(3):145–157.</ref> | |||
'''Education''' | |||
* Role of physiotherapy and expected outcomes of physiotherapy interventions | |||
* Importance of weight reduction (combination of diet and exercise) | |||
* Self-management of pain: Use of modalities such as heat and ice; Relaxation techniques; Coping strategies; Exercise<ref name=":0" /><ref name=":9" /><ref name=":11">Zhang W, Doherty M, Arden N, Bannwarth B, Bijlsma J, Gunther KP, Hauselmann HJ, Herrero-Beaumont G, Jordan K, Kaklamanis P, Leeb B. [https://ard.bmj.com/content/annrheumdis/64/5/669.full.pdf EULAR evidence based recommendations for the management of hip osteoarthritis: Report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT).] Annals of the rheumatic diseases 2005;64(5):669-81.</ref> | |||
'''Assistive devices''' | |||
* [[Walking Aids|Mobility assistive devices]] like [[Walking stick|walking sticks]]/[[canes]], [[crutches]], or [[Walkers|walking frames]] can improve mobility and independence of the patient. Occupational therapy also plays a role here, as they often also assists the patients with functional assistive devices like a long-handled reacher to pick up low-lying things, which will helps to avoid movements that may cause pain. | |||
= | * '''The RACPG 20188 guidelines''' '''Assistive walking device – Hip OA'''<ref name=":12" /> It may be appropriate to offer an assistive walking device (eg cane) for some people with knee and/or hip OA, depending on a person’s preference and capability. | ||
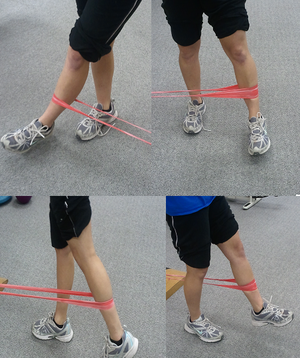
'''Exercise therapy'''[[File:Hip Theraband.png|right|frameless]] | |||
Exercise therapy is an effective treatment modality for hip osteo-arthrosis.<ref name=":1" /> Specific exercises can increase range of motion and flexibility, as well as strengthen the muscles of the hip and leg. Physiotherapists work together with the patient to develop an individualized, customized exercise program that meets the needs and lifestyle of the patient.<ref name=":1" /><ref name=":11" /> The benefits of exercise can assist the patients in their self-management of hip osteoarthritis. | |||
== | * Hydrotherapy is effective in the management of hip osteoarthritis. The combination of buoyancy and the reduction of gravity greatly assists patients that are struggling to weight-bear as a result of the pain from the hip osteoarthritis.<ref name=":11" /> | ||
* A 2016 study of 210 people with hip OA found that those who participated in a 12-week exercise program had less pain and more mobility than the placebo or no-treatment groups.<ref>Arthritis Foundation [https://www.arthritis.org/about-arthritis/types/osteoarthritis/articles/hip-oa-exercises.php Exercise Benefits for Hip Osteoarthritis] Available from: https://www.arthritis.org/about-arthritis/types/osteoarthritis/articles/hip-oa-exercises.php (last accessed 19.11.2019)</ref> | |||
* A study on a 6 week education and exercise programme has shown significant and sustained improvements in pain and disability on patients wait-listed for joint replacement surgery. Further positive results included improvements in function, knowledge and psycho-social aspects.<ref>Saw MM. [https://open.uct.ac.za/bitstream/handle/11427/15719/thesis_hsf_2015_saw_melissa_michelle.pdf?sequence=1&isAllowed=y <nowiki>The effects of a six-week physiotherapist-led exercise and education intervention in patients with osteoarthritis, awaiting an arthroplasty in the South Africa [dissertation]</nowiki>]. Cape Town: University of Cape Town. 2015.</ref> Clinical trials further suggest that it can postpone the need of total hip replacement surgery.<ref name=":11" /> | |||
[[File:Hip exercise 3.png|thumb|Hip abduction exercise]] | |||
'''The RACPG 20188 guidelines recommend as per below''' | |||
1.Land-based exercise – Hip OA <ref name=":12" /> | |||
* We strongly recommend offering land-based exercise for all people with hip OA to improve pain and function, regardless of their age, structural disease severity, functional status or pain levels. Exercise has also been found to be beneficial for other comorbidities and overall health. However, we are unable to specifically recommend either for or against different types of land-based exercise at this stage. Clinicians should prescribe an individualised progressive exercise [[File:Hydrotherapy Pool Exercises.jpg|thumb|Hydrotherapy Pool Exercises]]program, taking into account the person’s preference, capability and the availability of local facilities. Realistic goals should be set. Dosage should be progressed with full consideration given to the frequency, duration and intensity of exercise sessions, number of sessions, and the period over which sessions should occur. The clinician should monitor the person’s response to the exercise program and could try a different form of land-based exercise if improvements are not evident. Attention should be paid to strategies to optimise adherence. Strong for recommendation (when combining all studies of land-based exercise) Conditional (neutral) for recommending one type of land-based exercise over another (eg walking, muscle strengthening, stationary cycling, Tai Chi, Hatha yoga) Moderate (land-based) Very low (walking, muscle strengthening, stationary cycling, Tai Chi, Hatha yoga) | |||
< | 2. Aquatic exercise/ hydrotherapy – Hip OA<ref name=":12" /> | ||
* It may be appropriate to offer aquatic exercise/hydrotherapy for some people with knee and/or hip OA. This will depend upon personal preference and the availability of local facilities. | |||
'''Manual therapy''' | |||
</ | [[File:Prone Hip Posterior to Anterior Glide.JPG|thumb|Hip Posterior to Anterior Glide]] | ||
A range of manual therapies is used in the treatment of hip osteoarthritis:<ref name=":1" /> | |||
* Soft tissue techniques and stretches | |||
* Mobilization of accessory and physiological movements | |||
* Manipulation | |||
< | Research is inconclusive on the effect of manual therapy in the treatment of hip osteoarthritis.<ref name=":0" /> The immediate effect of a manual therapy, specifically joint mobilization decrease pain and improve hip range of motion, especially in the elderly population. Joint mobilization might reduce pain, might ''‘provide a stretching effect on the joint capsules and muscles, thus restoring normal arthrokinematics or may induce pain inhibition and improved motor control’'' and might reduce kinesiophobia.<ref name=":4">Beselga C, Neto F, Alburquerque-Sendín F, Hall T, Oliveira-Campelo N. [https://espace.curtin.edu.au/bitstream/handle/20.500.11937/34768/239353_239353.pdf?sequence=2 Immediate effects of hip mobilization with movement in patients with hip osteoarthritis: A randomised controlled trial.] Man Ther. 2016;22:80-5. | ||
</ref> | |||
< | '''The RACPG 20188 guidelines''' '''Massage''' '''and Manual''' '''therapy –''' '''Hip OA'''<ref name=":12" /> | ||
* It may be appropriate to offer a short course of massage therapy for some people with hip osteoarthritis (OA). This should be considered only as an adjunctive treatment to enable engagement with active management strategies, and only for short term, cognisant of issues related to cost and access. | |||
* Manual therapy (stretching, soft tissue and/or joint mobilisation and/ or manipulation) It may be appropriate to offer a short course of manual therapy (stretching, soft tissue and/or joint mobilisation and/ or manipulation) for some people with hip OA. This should be considered only as an adjunctive treatment to enable engagement with active management strategies and only for short term, cognisant of issues related to cost and access. | |||
== | == Outcome Measures == | ||
* [[Visual Analogue Scale|Visual analogue scale]] (VAS) | |||
* Hip disability and osteoarthritis outcome score ([[Hip Disability and Osteoarthritis Outcome Score|HOOS]]) | |||
* Western Ontario and McMaster universities osteoarthritis index ([[WOMAC Osteoarthritis Index|WOMAC]]) | |||
* [[Harris Hip Score|Harris hip score]] | |||
* Oxford hip score ([http://www.orthopaedicscore.com/scorepages/oxford_hip_score.html/ OHS]) | |||
* [[Six Minute Walk Test / 6 Minute Walk Test|6 Minute Walking Test]] | |||
* [[Timed Up and Go Test (TUG)|Timed up and go test]] | |||
* [[International Hip Outcome Tool (iHOT)|International Hip Outcome Tool]] | |||
* [[Ibadan Knee/Hip Osteoarthritis Outcome Measure (IKHOAM)|Ibadan Knee/Hip Osteoarthritis Outcome Measure]] | |||
=== The Future === | |||
'''<u></u><u></u>'''<u></u>Highly prevalent among the elderly, Hip osteoarthritis (OA) is highly prevalent among the elderly and carries a heavy burden of disease. Guidelines for the management of hip OA are often extrapolated from knee OA research, despite clear differences in the etiopathogenesis and response to treatments of OA at these sites. True inroads in reducing the burden of hip OA are most likely to be seen with an increased focus on risk factor modification prior to or in the early stages of the condition’s pathogenesis. Risk calculators such as those that currently exist for heart disease could be developed, incorporating imaging and even genetic biomarkers to enable stratification of people into varying risk levels for appropriate monitoring and management. With improved understanding of the etiopathogenesis of hip OA, intervention prior to or early in the disease course in a disease-modifying manner is likely to become feasible in the future. The management of hip OA has the potential to be an area of medicine undergoing substantial advancement in the decades to come.<ref>Murphy NJ, Eyles JP, Hunter DJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5083776/ Hip osteoarthritis: etiopathogenesis and implications for management.] Advances in therapy. 2016 Nov 1;33(11):1921-46. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5083776/ (last accessed 19.11.2019)</ref> | |||
== Resources == | |||
* [https://open.uct.ac.za/bitstream/handle/11427/12697/Living%20with%20Osteoarthritis_2018.pdf?sequence=18 Patient workbook] on "living with osteoarthritis" | |||
* [https://new-learning.bmj.com/course/10052313 The health benefits of physical activity: osteoarthritis and low back pain] | |||
* [http://www.fyss.se/wp-content/uploads/2018/01/37.-Osteoarthritis.pdf Physical activity in the prevention and treatment of the disease- Osteoarthritis] | |||
* [https://oaaction.unc.edu/health-care/ Physical activity implementation guide for osteoarthritis] | |||
== | === References === | ||
<references /> | |||
[[Category:Older People/Geriatrics]] | |||
[[Category:Osteoarthritis]] | |||
< | [[Category:Anatomy]] | ||
[[Category:Older People/Geriatrics - Conditions]] | |||
[[Category:Hip - Conditions]] | |||
[[Category:Rheumatology]] | |||
[[Category: | |||
Latest revision as of 03:29, 3 September 2023
Original Editor - Eric Robertson, Kim Presiaux
Top Contributors - Kim Presiaux, Dorien De Strijcker, Lucinda hampton, Davy Duverger, Leana Louw, Kim Jackson, Admin, Rachael Lowe, Laura Ritchie, Johnathan Fahrner, Van Horebeek Erika, Scott Buxton, Vidya Acharya, Kai A. Sigel, Eric Robertson, Areeba Raja, 127.0.0.1, Bram Van Roost, Shaimaa Eldib, Lauren Lopez, Loïc Byl, Marius De Bruyn and Kevin Vandebroucq
Introduction[edit | edit source]
Osteoarthritis is a common disabling condition that causes joint pain and stiffness caused by the gradual erosion of cartilage. Hip osteoarthritis is a common form of osteoarthritis that causes restricted locomotor activity and functional disability, and may progress to the point where joint replacement is needed. Hip osteoarthritis is a major global public-health burden. [1]
- For people with hip arthritis, physiotherapy may assist in conditioning and obtaining endurance of the surrounding muscles that support the joint.
- A long term approach to the management of a hip OA should include some type of regular physical therapy or conditioning program.
Epidemiology[edit | edit source]
Globally, from 1990 to 2019, the age-standardized incidence rate of hip osteoarthritis increased from 17.02 per 100,000 persons to 18.70 per 100,000 persons. The burden of hip osteoarthritis has increased in almost all countries over the past 30 years, this increasing trend is expected to continue, due to the rapid aging of the world’s population.
- Osteoarthritis is the most common cause of hip pain in older adults (older than 50 years of age).
- Prevalence rates for adult hip OA range from 0.4% to 27%.
- The reported prevalence of hip OA shows great variability, with men showing higher prevalence of radiographic hip OA.[1][2]
- Lifetime risk for symptomatic hip OA is 18.5% for men and 28.6% for women[3].
- Research suggest that there are a 25% risk of developing hip osteoarthritis for people who live to the age of 85,[4]
Pathology[edit | edit source]
Osteoarthritis is distinguished by an active progressive alteration of the whole synovial joint, being due to a combination of mechanical, inflammatory and metabolic factors. It is caused by an imbalance between the destruction and repair of the affected tissues. The disease affects the
- Hyaline cartilage: loses its structural integrity due to composition changes.
- Subchondral bone
- Joint capsule
- Synovium
- Ligaments and the periarticular muscles.
Risk Factors[edit | edit source]
Risk factors that increase the likelihood of developing osteoarthritis of the hip are
- Older age
- Obesity
- Genetics
- Repetitive stress and mechanical overload
- Farmers, construction workers
- High impact sports eg football, handball, hockey, wrestling, weight-lifting, and long-distance running
- Acetabular dysplasia
- Femoroacetabular impingement
- Slipped capital femoral epiphysis
- Perthes disease
- Trauma, e.g. hip dislocation or hip fracture[5]
Diagnosis[edit | edit source]
The following criteria should be used to classify adults over the age of 50 with hip OA:
- Moderate anterior or lateral hip pain during weight-bearing activities
- Morning stiffness less than 1 hour in duration after wakening
- Hip internal rotation range of motion less than 24° or internal rotation and hip flexion 15° less than the nonpainful side, and/or increased hip pain associated with passive hip internal rotation.[2]
Radiographic evidence: joint space narrowing, marginal osteophytes, subchondral sclerosis, and bone cysts.[6][7].
Clinical Presentation[edit | edit source]
Pain characteristics:
- Slowly progressive hip pain, or hip-related groin pain radiating into the thigh, buttocks or knee.
- The pain can be worse at night, at rest or with strenuous activity, reducing the range of motion and limiting walking distance. It can be associated with stiffness particular in the morning or after rest.
Other symptoms include locking, grinding and joint instability, fatigue and pain-related psychological stress.[8]
Physical Examination[edit | edit source]
A physical examination includes (Also also hip examination)
- Observation
- Subjective interview:
- Complaints of pain, deformity, stiffness and/or limp
- Previous history linked to hip pain (congenital or childhood problems, previous trauma)
- Physical examination in Standing and Supine (look for leg length discrepancy, antalgic gait and Trendelenberg gait)
- Objective observation (posture, deformities, muscle atrophy)
- Palpation:
- Tenderness at the hip
- Pain and sensitivity over greater trochanter
- Range of motion:
- Early signs of hip osteoarthritis is limited abduction and rotation. As the disease progresses, flexion, extension and adduction becomes more difficult.
- Normally painful at end of available range of motion
- Crepitis with movement[9][10][11]
Five variables for detecting hip osteoarthritis are:
- Self-reported squatting as an aggravating factor
- Active hip flexion causing lateral hip pain
- Hip Quadrant test with adduction causing lateral hip or groin pain
- Active hip extension causing pain
- Passive internal rotation of less than or equal to 25°
If there are 3/5 variables present, the chance of having OA is 68%. With 4-5/5 the chance increases to 91%. The variables are positive when there’s pain or a limited range of motion in the tests.[12]
Management[edit | edit source]
A biopsychosocial approach offers the best outcome.[13] A multidisciplinary team may be involved including: doctors, physiotherapists, dietitians, and occupational therapists.
Management of hip osteoarthritis varies according to the severity of the condition. A combination of pharmaceutical and non-pharmaceutical modalities is recommended for the optimal management of the condition. Physiotherapy plays an important role in customized exercise programmes for patients living with hip osteoarthritis.
- OA management includes patient education combined with exercise and/or manual therapy. Education should include teaching activity modification, exercise [14], supporting weight reduction when overweight (see below), and methods of unloading the arthritic joints.
- Management includes providing impairment-based functional, gait, and balance training, including the proper use of assistive devices (canes, crutches, walkers), to patients with hip osteoarthritis and activity limitations, balance impairment, and/or gait limitations when associated problems are observed.[2]
- Offer topical or oral nonsteroidal anti-inflammatory drugs in those without contraindications.
- Intra-articular steroid injections provide short-term pain relief and duloxetine has demonstrated efficacy. Opiates should be avoided.[7]
Weight management – Hip OA[15](RACPG 2018 guidelines): We strongly recommend weight management for people with hip OA. For those who are overweight (body mass index [BMI] ≥25 kg/m2 ) or obese (BMI ≥30 kg/m2 ), a minimum weight loss target of 5–7.5% of body weight is recommended. It is beneficial to achieve a greater amount of weight loss given that a relationship exists between the amount of weight loss and symptomatic benefits. Weight loss should be combined with exercise for greater benefits. For people of healthy body weight, education about the importance of maintaining healthy body weight is essential.
Surgical interventions: Total hip replacement - The option in patients with symptomatic and radiographic osteoarthritis characterized by refractory pain and disability; Osteotomy and hip resurfacing - Should be considered in younger patients with symptomatic secondary osteoarthritis due to acetabular dysplasia, femoroacetabular impingement, varus or valgus deformity[8].
Physiotherapy Management[edit | edit source]
Physiotherapy plays in major role in the management of patients with hip osteoarthritis. The goal is to improve strength, mobility and increase range of motion. Physiotherapy also helps relieve pain and restores normal movement in the hip and legs and also addresses pain management and functional adaptions. Patient-specific exercise programmes has shown to decrease pain and improve function in hip osteoarthritis.[4][13]
Education
- Role of physiotherapy and expected outcomes of physiotherapy interventions
- Importance of weight reduction (combination of diet and exercise)
- Self-management of pain: Use of modalities such as heat and ice; Relaxation techniques; Coping strategies; Exercise[4][9][16]
Assistive devices
- Mobility assistive devices like walking sticks/canes, crutches, or walking frames can improve mobility and independence of the patient. Occupational therapy also plays a role here, as they often also assists the patients with functional assistive devices like a long-handled reacher to pick up low-lying things, which will helps to avoid movements that may cause pain.
- The RACPG 20188 guidelines Assistive walking device – Hip OA[15] It may be appropriate to offer an assistive walking device (eg cane) for some people with knee and/or hip OA, depending on a person’s preference and capability.
Exercise therapy
Exercise therapy is an effective treatment modality for hip osteo-arthrosis.[13] Specific exercises can increase range of motion and flexibility, as well as strengthen the muscles of the hip and leg. Physiotherapists work together with the patient to develop an individualized, customized exercise program that meets the needs and lifestyle of the patient.[13][16] The benefits of exercise can assist the patients in their self-management of hip osteoarthritis.
- Hydrotherapy is effective in the management of hip osteoarthritis. The combination of buoyancy and the reduction of gravity greatly assists patients that are struggling to weight-bear as a result of the pain from the hip osteoarthritis.[16]
- A 2016 study of 210 people with hip OA found that those who participated in a 12-week exercise program had less pain and more mobility than the placebo or no-treatment groups.[17]
- A study on a 6 week education and exercise programme has shown significant and sustained improvements in pain and disability on patients wait-listed for joint replacement surgery. Further positive results included improvements in function, knowledge and psycho-social aspects.[18] Clinical trials further suggest that it can postpone the need of total hip replacement surgery.[16]
The RACPG 20188 guidelines recommend as per below
1.Land-based exercise – Hip OA [15]
- We strongly recommend offering land-based exercise for all people with hip OA to improve pain and function, regardless of their age, structural disease severity, functional status or pain levels. Exercise has also been found to be beneficial for other comorbidities and overall health. However, we are unable to specifically recommend either for or against different types of land-based exercise at this stage. Clinicians should prescribe an individualised progressive exercise program, taking into account the person’s preference, capability and the availability of local facilities. Realistic goals should be set. Dosage should be progressed with full consideration given to the frequency, duration and intensity of exercise sessions, number of sessions, and the period over which sessions should occur. The clinician should monitor the person’s response to the exercise program and could try a different form of land-based exercise if improvements are not evident. Attention should be paid to strategies to optimise adherence. Strong for recommendation (when combining all studies of land-based exercise) Conditional (neutral) for recommending one type of land-based exercise over another (eg walking, muscle strengthening, stationary cycling, Tai Chi, Hatha yoga) Moderate (land-based) Very low (walking, muscle strengthening, stationary cycling, Tai Chi, Hatha yoga)
2. Aquatic exercise/ hydrotherapy – Hip OA[15]
- It may be appropriate to offer aquatic exercise/hydrotherapy for some people with knee and/or hip OA. This will depend upon personal preference and the availability of local facilities.
Manual therapy
A range of manual therapies is used in the treatment of hip osteoarthritis:[13]
- Soft tissue techniques and stretches
- Mobilization of accessory and physiological movements
- Manipulation
Research is inconclusive on the effect of manual therapy in the treatment of hip osteoarthritis.[4] The immediate effect of a manual therapy, specifically joint mobilization decrease pain and improve hip range of motion, especially in the elderly population. Joint mobilization might reduce pain, might ‘provide a stretching effect on the joint capsules and muscles, thus restoring normal arthrokinematics or may induce pain inhibition and improved motor control’ and might reduce kinesiophobia.[19]
The RACPG 20188 guidelines Massage and Manual therapy – Hip OA[15]
- It may be appropriate to offer a short course of massage therapy for some people with hip osteoarthritis (OA). This should be considered only as an adjunctive treatment to enable engagement with active management strategies, and only for short term, cognisant of issues related to cost and access.
- Manual therapy (stretching, soft tissue and/or joint mobilisation and/ or manipulation) It may be appropriate to offer a short course of manual therapy (stretching, soft tissue and/or joint mobilisation and/ or manipulation) for some people with hip OA. This should be considered only as an adjunctive treatment to enable engagement with active management strategies and only for short term, cognisant of issues related to cost and access.
Outcome Measures[edit | edit source]
- Visual analogue scale (VAS)
- Hip disability and osteoarthritis outcome score (HOOS)
- Western Ontario and McMaster universities osteoarthritis index (WOMAC)
- Harris hip score
- Oxford hip score (OHS)
- 6 Minute Walking Test
- Timed up and go test
- International Hip Outcome Tool
- Ibadan Knee/Hip Osteoarthritis Outcome Measure
The Future[edit | edit source]
Highly prevalent among the elderly, Hip osteoarthritis (OA) is highly prevalent among the elderly and carries a heavy burden of disease. Guidelines for the management of hip OA are often extrapolated from knee OA research, despite clear differences in the etiopathogenesis and response to treatments of OA at these sites. True inroads in reducing the burden of hip OA are most likely to be seen with an increased focus on risk factor modification prior to or in the early stages of the condition’s pathogenesis. Risk calculators such as those that currently exist for heart disease could be developed, incorporating imaging and even genetic biomarkers to enable stratification of people into varying risk levels for appropriate monitoring and management. With improved understanding of the etiopathogenesis of hip OA, intervention prior to or early in the disease course in a disease-modifying manner is likely to become feasible in the future. The management of hip OA has the potential to be an area of medicine undergoing substantial advancement in the decades to come.[20]
Resources[edit | edit source]
- Patient workbook on "living with osteoarthritis"
- The health benefits of physical activity: osteoarthritis and low back pain
- Physical activity in the prevention and treatment of the disease- Osteoarthritis
- Physical activity implementation guide for osteoarthritis
References[edit | edit source]
- ↑ 1.0 1.1 Fu M, Zhou H, Li Y, Jin H, Liu X. Global, regional, and national burdens of hip osteoarthritis from 1990 to 2019: estimates from the 2019 Global Burden of Disease Study. Arthritis research & therapy. 2022 Dec;24(1):1-1.Available;https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-021-02705-6#Sec9 (accessed 15.11.2022)
- ↑ 2.0 2.1 2.2 Cibulka MT, Bloom NJ, Enseki KR, MacDonald CW, Woehrle J, McDonough CM. Hip pain and mobility deficits—hip osteoarthritis: revision 2017: clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy. 2017 Jun;47(6):A1-37.Available:https://www.jospt.org/doi/10.2519/jospt.2017.0301 (accessed 15.11.2022)
- ↑ Lespasio MJ, Sultan AA, Piuzzi NS, Khlopas A, Husni ME, Muschler GF, Mont MA. Hip osteoarthritis: a primer. The Permanente Journal. 2018;22. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5760056/ (last accessed 19.11.2019)
- ↑ 4.0 4.1 4.2 4.3 Murphy NJ, Eyles JP, Hunter DJ. Hip osteoarthritis: Etiopathogenesis and implications for management. Advances in therapy 2016;33(11):1921-46.
- ↑ Radiopedia Hip OA Available:https://radiopaedia.org/articles/osteoarthritis-of-the-hip (accessed 15.11.2022)
- ↑ Brandt CD. Diagnosis and non-surgical management of osteoarthritis. USA: Professional Communications, Inc. 2010.
- ↑ 7.0 7.1 Katz JN, Arant KR, Loeser RF. Diagnosis and treatment of hip and knee osteoarthritis: a review. Jama. 2021 Feb 9;325(6):568-78. Available: https://jamanetwork.com/journals/jama/article-abstract/2776205(accessed 23.1.2022)
- ↑ 8.0 8.1 Radiopedia OA of the hip Available: https://radiopaedia.org/articles/osteoarthritis-of-the-hip?lang=us(accessed 23.1.2022)
- ↑ 9.0 9.1 American Academy of Orthopaedic Surgeons. Diseases and conditions: Osteoarthritis of the hip.https://orthoinfo.aaos.org/en/diseases--conditions/osteoarthritis-of-the-hip (accessed 14/07/2018).
- ↑ Crielaard JM, Dequeker J, Famaey JP, Franchimong P, Gritten CH., Huaux JP. Osteoartrose. Brussels: Drukkerij Lichtert, 1985.
- ↑ Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.
- ↑ Sutlive TG, Lopez HP, Schnitker DE, Yawn SE, Halle RJ, Mansfield LT et al. Development of a clinical prediction rule for diagnosing hip osteoarthritis in individuals with unilateral hip pain. J Orthop Sports Phys Ther. 2008;38(9):542-50.
- ↑ 13.0 13.1 13.2 13.3 13.4 Bennell K. Physiotherapy management of hip osteoarthritis. J Physiother. 2013; 59(3):145–157.
- ↑ Dalmas I, Agius TP, Sciriha A. Core muscle strengthening exercises in the management of hip osteoarthritis: outcomes of a 12-week programme. European Journal of Physiotherapy. 2023 Mar 27:1-8.
- ↑ 15.0 15.1 15.2 15.3 15.4 2018 RACGP Guidelines for hip and knee arthritis Available from: https://www.racgp.org.au/download/Documents/Guidelines/Musculoskeletal/guideline-for-the-management-of-knee-and-hip-oa-2nd-edition.pdf (last accessed 19.11.2019)
- ↑ 16.0 16.1 16.2 16.3 Zhang W, Doherty M, Arden N, Bannwarth B, Bijlsma J, Gunther KP, Hauselmann HJ, Herrero-Beaumont G, Jordan K, Kaklamanis P, Leeb B. EULAR evidence based recommendations for the management of hip osteoarthritis: Report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Annals of the rheumatic diseases 2005;64(5):669-81.
- ↑ Arthritis Foundation Exercise Benefits for Hip Osteoarthritis Available from: https://www.arthritis.org/about-arthritis/types/osteoarthritis/articles/hip-oa-exercises.php (last accessed 19.11.2019)
- ↑ Saw MM. The effects of a six-week physiotherapist-led exercise and education intervention in patients with osteoarthritis, awaiting an arthroplasty in the South Africa [dissertation]. Cape Town: University of Cape Town. 2015.
- ↑ Beselga C, Neto F, Alburquerque-Sendín F, Hall T, Oliveira-Campelo N. Immediate effects of hip mobilization with movement in patients with hip osteoarthritis: A randomised controlled trial. Man Ther. 2016;22:80-5.
- ↑ Murphy NJ, Eyles JP, Hunter DJ. Hip osteoarthritis: etiopathogenesis and implications for management. Advances in therapy. 2016 Nov 1;33(11):1921-46. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5083776/ (last accessed 19.11.2019)