Physical Activity in Adolescents with Haemophilia: Difference between revisions
No edit summary |
Rucha Gadgil (talk | contribs) No edit summary |
||
| (313 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class=" | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Caitlin MacRae|Caitlin MacRae]], [[User:Hazel Burt|Hazel Burt]], [[User: Steven Flett|Steven Flett]], [[User:Alex Leishman|Alex Leishman]] and [[User:Chloe Allan|Chloe Allan]] as part of the [[Current and Emerging Roles in Physiotherapy Practice|Queen Margaret University's Current and Emerging Roles in Physiotherapy Practice Project]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction== | ||
<br> | Physical activity and exercise, are often used synonymously, however, physical activity is defined as “as any bodily movement produced by skeletal muscles that require energy expenditure” <ref name="WHO 2016">World Health Organization. Physical Activity. http://www.who.int/topics/physical_activity/en/ (accessed 25 January 2016).</ref>, and exercise is a subsection of physical activity, involving planned or structured activity which aims to improve or maintain physical fitness <ref name="Caperson et al. 2016">Casperson SJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public health Rep 1985;100;(2):126–131. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1424733/ (accessed 25 January 2016).</ref>.<br><br>The physiotherapist's role in treating and managing adolescents with haemophilia (AWH) is extremely important, and recent developments within this profession have increased its value <ref name="Buzzard and Beeton 2008">Buzzard B, Beeton K. Physiotherapy Management of Haemophilia. Oxford: Wiley, 2008.</ref>. One of the key interventions involved in its treatment is the promotion of physical activity <ref name="WFH 2015">World Federation of Heamophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd 2012;2:6-73. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 October 2015).</ref>. | ||
== Definition == | |||
[[Hemophilia|Haemophilia]] is a rare inherited disorder where blood in the body has an inability to produce sufficient clotting factor, a protein which controls bleeding <ref name="NHS choices 2015">NHS Choices. Haemophilia. http://www.nhs.uk/conditions/haemophilia/Pages/Introduction.aspx (accessed 7 Jan 2016).</ref>. This lack of clotting factor can lead to severe and prolonged bleeds which may cause permanent damage to the site of haemorrhage and surrounding tissues<ref name="Severity">World Federation of Haemophilia. Severity of hemophilia. http://www.wfh.org/en/page.aspx?pid=643 (accessed 7 January 2016).</ref>. There are an estimated 6000 people living in the United Kingdom with the condition. It occurs mainly through a gene passed from parent to child on the X chromosome, i.e. it mainly affects males<ref name="Great Ormond Street 2015">Great Ormond Street Hospital. What causes Haemophilia? http://www.gosh.nhs.uk/medical-information/search-medical-conditions/haemophilia (accessed 10 Jan 2016).</ref>. <br>There are four main types of haemophilia. The table below shows the missing clotting factor and commonality for each type:[[Image:Types table.jpg|center|500px]] | |||
* Haemophilia A is the most common type affecting around 80% of the haemophilic population<ref name="Haem Society 2015 A">The Haemophilia Society. Haemophilia A.fckLRhttp://www.haemophilia.org.uk/bleeding_disorders/bleeding_disorders/haemophilia_a (accessed 9 November 2015).</ref><span style="line-height: 1.5em; font-size: 13.28px;">. </span>This is where the individual will either have low levels of clotting factor eight or it is completely missing<span style="line-height: 1.5em; font-size: 13.28px;">. </span> | |||
* Haemophilia B is less common. This is where clotting factor nine is either very low or is missing from the blood. Around 20% of PWH will have this type<ref name="Haem Society 2015 B">The Haemophilia Society. Haemophilia B. fckLRhttp://www.haemophilia.org.uk/bleeding_disorders/bleeding_disorders/haemophilia_fckLRb (accessed 9 November 2015).</ref>. | |||
* Haemophilia C is ten times rarer than type A and differs from both A and B as it can present in both genders. However, this is extremely rare and can only occur when the mother and father are both carriers of the gene <ref name="Haemophilia Information 2013">Haemophilia Information. Haemophilia Genetics. http://www.hemophilia-information.com/hemophilia-genetics.html (accessed 12 September 2015).</ref>. Individuals with type C will have low levels of clotting factor eleven, or this will be completed absent. | |||
* Acquired Haemophilia is extremely rare. This type is not inherited in the same way, as it is an auto-immune disorder. This is where the body's immune system attacks the clotting factors. This condition can also affect both males and females <ref name="Grethlein 2014">Grethlein SJ. Acquired Haemophilia. http://emedicine.medscape.com/article/211186-overview#a2fckLR (accessed 7 January 2016).</ref>. | |||
=== Classifications and Severities === | |||
=== | The table below categorises haemophilia into mild, moderate and severe, showing the percentage of sufferers in each category <ref name="Preston et al. 2004">Preston FE, Kitchen S, Jennings L, Woods TA, Mackris M. SSC/ISTH classification of hemophilia A: can hemophilia center laboratories achieve the new criteria? J Thromb Haemost 2004;(2):271-4. http://www.ncbi.nlm.nih.gov/pubmed/14995989 (accessed 10 January 2016).</ref>.[[Image:Severityhaem.jpg|center|600px]]<br>Like other disorders, haemophilia can affect individuals to varying degrees. The symptoms can be mild, moderate or severe, depending on the level of clotting factor present<ref name="nhs choices 2016">NHS Choices. Haemophilia symptoms. http://www.nhs.uk/Conditions/Haemophilia/Pages/Symptoms.aspx (accessed 10 Jan 2016).</ref>. | ||
=== Multidisciplinary Team Involvement === | |||
Despite recent development in the management of the condition, patients still require comprehensive multidisciplinary care throughout all stages of their life <ref name="Breakey et al. 2010" />. A multidisciplinary team involves a range of professionals who collaborate together to structure a treatment plan for an individual, aiming to achieve high quality patient-centered care <ref name="Department of Health 2015">Department of Health. Multidisciplinary teams (MDT’s). http://www.health.nt.gov.au/Cancer_Services/CanNET_NT/Multidisciplinary_Teams/index.aspx (accessed 7 Jan 2016).</ref>. | |||
The collaboration of all professionals allows a holistic approach to be considered which takes into account the individual’s physical, social, emotional, cultural and spiritual needs <ref name="CSP 2015">Chartered Society of Physiotherapy. Physiotherapy works for social care – Why Physiotherapy? http://www.csp.org.uk/physiotherapy-works-social-care (accessed 10 Jan 2016).</ref>. This is especially important during the transition from childhood into adulthood which can cause additional stress for those with chronic disorders. Therefore during this time they need for the MDT to work together is essential <ref name="Breakey et al. 2010">Breakey VR, Blanchette VS, Bolton-Maggs PHB. Towards comprehensive care in transition for young people with haemophilia. Haemophilia 2010;16(6):848-857. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2010.02249.x/abstract (accessed 18 Dec 2015).</ref>. This may mean referring the patient to another team member to allow high-quality treatment, specific to the patients needs. [[Image:Mdt altered.jpg|center|725px]] | |||
== The Role of the Physiotherapist == | |||
=== Assessment === | |||
[[Image:Joint swelling.jpg|250px|right]]When assessing a patients condition or evaluating the success of interventions it is often beneficial for the physiotherapist to use a standardised outcome measure. These offer an objective measure which can help to monitor change in a patients symptoms<ref>American Physical Therapy Association. Outcome Measures in Patient Care. http://www.apta.org/OutcomeMeasures/ (accessed 20 Jan 2016).</ref>.<br><br>Symptoms of a joint bleed may include swollen and hot joints, pain in the area and stiffness when mobilising. Many patients have described the overall feeling as an 'aura' surrounding the joint<ref name="Haem care">Haemophilia Care. How to recognise a bleed. http://www.haemophiliacare.co.uk/how-to-recognise-a-bleed.html (accessed 7 Jan 2016)</ref>, for example swelling in the knee during a joint bleed. | |||
=== Outcome Measures: === | |||
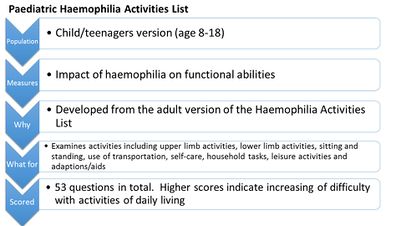
[[Image:Hjhs.jpg|414x414px|right]]'The Haemophilia Joint Health Score' <ref name="International Prophlaxis Study Group 2015">International Prophylaxis Study Group. HJHS. http://ipsg.ca/working-groups/physical-therapy/info/hjhs (accessed 15 Dec 2015).</ref> is designed for physiotherapists and recommended for use by professionals specialised in haemophilia treatment. The outcome measure takes approximately 45 – 60 minutes to complete and is designed specifically for children with haemophilia. It examines the condition of a joint affected by a bleed and can be used to demonstrate degeneration in a joint over time.[[File:Paediatric_Haemophilia_Activities_List_picture.jpg|right|401x401px]] | |||
The 'Paediatric Haemophilia Activities List’ is another outcome measure used for individuals with haemophilia. Adolescents will complete the child/teenager version explaining to what extent their haemophilia impacts upon their daily activities The questionnaire can then be used by healthcare professionals involved in their care<ref name="WFH ACTIVITES">World Federation of Haemophilia, Paediatric Haemophilia Activities List: http://www.wfh.org/en/page.aspx?pid=886 (accessed 20 Oct 2015).</ref>.<br> | |||
Although outcome measures exist for the assessment of children with haemophilia many of these have demonstrated poor validity and reliability<ref>Stephensen D, Drechsler WI, Scott OM. Outcome measures monitoring physical function in children with haemophilia: a systematic review. Haemophilia 2014;20:306-321. http://onlinelibrary.wiley.com/doi/10.1111/hae.12299/epdf (accessed 19 Jan 2016).</ref>. | |||
=== Management === | |||
The main role of the physiotherapist when treating an AWH involves the management of impairments from a musculoskeletal perspective, aiming to restore and improve function. Some of these include: haemarthoses, synovitis, joint contractures, haemotomas and haemophilic arthropathys<ref>Buzzard B, Beeton K. Physiotherapy Management of Haemophilia. Wiley-Blackwell, 2010.</ref>. | |||
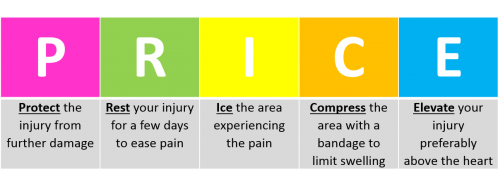
During the acute phase, the physiotherapist will attempt to minimise bleeding using the PRICE regime (protection, rest, ice, compression elevation)<ref name="HAEM CARE">Haemophilia Care. How is Physiotherapy used in Haemophilia care. http://www.haemophiliacare.co.uk/physiotherapy.html (accessed 10 Oct 2015).</ref>. This will also work in conjunction with factor replacement if necessary.[[Image:PRICE2.png|center|500px]]<br>Following the acute phase, the physiotherapy management will focus on regaining full range of movement, muscle strength and reducing pain<ref>Talking Joints. Let’s talk about physiotherapy for haemophilia patients. https://www.novonordisk.com/content/dam/Denmark/HQ/aboutus/documents/cpih-2015-talkingjoints-brochure-lets-talk-physiotherapy.pdf (accessed 10 Oct 2016).</ref>. As soon as the pain and swelling begin to decrease, the patient should be encouraged to gradually increase the joint range aiming to achieve complete extension. This should be done actively by the patient to encourage muscle contraction, however passive movements may initially be used. It is vital that early active muscle control occurs to prevent the loss of joint movement <ref name="Hermans et al. 2011">Hermans C, De Moerloose P, Fischer K, Holstein K, Klamroth R, Lambert T, Lavigne-Lissalde G, Perez R, Richards M, Dolan G. European Haemophilia Therapy Standardisation Board. Management of acute haemarthrosis in haemophilia A without inhibitors: literature review, European survey and recommendations. Haemophilia 2011;17(3):383-92. http://www.ncbi.nlm.nih.gov/pubmed/21323794 (accessed 30 Sept 2015).</ref>;<ref name="Gomis et al. 2009">Gomis M, Querol F, Gallach JE, Gonzalez LM, Aznar JA. Exercise and sport in the treatment of haemophilic patients: a systematic review. Haemophilia 2009;15(1):43-54. http://www.ncbi.nlm.nih.gov/pubmed/18721151 (accessed 10 Jan 2016).</ref>;<ref name="Mulder 2006">Mulder K. Exercises for people with haemophilia. Montreal: World Federation of Haemophilia. 2006. http://scholar.google.co.uk/scholar_url?url=http%3A%2F%2Fhaemophilia.ie%2FPDF%2FExercise_Guide_med.pdf(accessed 22 Jan 2016).</ref>. Rehabilitation involving active exercises and proprioceptive training must then be continued until full pre-bleed joint ROM and function is restored <ref name="Heijnen and Buzzard 2005">Heijnen L, Buzzard BB. The role of physical therapy and rehabilitation in the management of hemophilia in developing countries. Semin Thromb Hemost 2005;31(5):513-7. http://www.ncbi.nlm.nih.gov/pubmed/16276459 (accessed 25 Sept 2015).</ref>. | |||
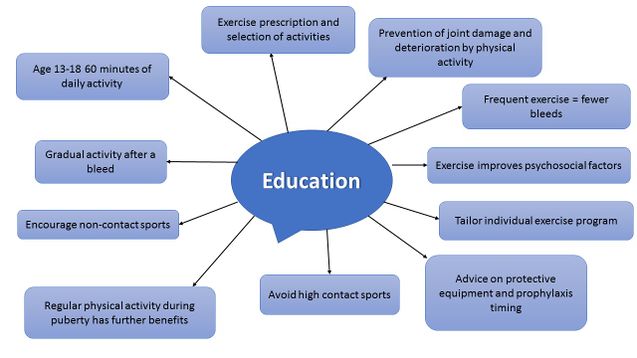
== | Another key role of the physiotherapist when treating an AWH is promotion of physical activity. Exercise is encouraged as it will improve the child’s fitness, reduce obesity levels, improve muscular strength, and reduce frequency of bleeding episodes and joint deterioration <ref name="Blamey 2010">Blamey G, Forsyth A, Zourikian N, Short L, Jankovic N, Kleijn PDE, Flannery T. Comprehensive elements of a physiotherapy exercise program in haemophilia – a global perspective. World Federation of Haemophilia 2010;16:136-145 http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2010.02312.x/abstract;jsessionid=BB3B137A0C21342D378A949A977850CA.f04t01fckLR(accessed 10 Oct 2015).</ref>. The World Federation of Haemophilia<ref>World Federation of Heamophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd 2012;2:6-73. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 Oct 2015).</ref> advise particular focus towards strengthening, co-ordination, achieving a healthy body weight and improving self-esteem. As well as the physical aspects concerned, a major aspect of physiotherapy management focuses on education and advice. | ||
==== Education ==== | |||
Below is a mind map which summarises key points regarding the advice that should be offered to patients around physical activity. <br> | |||
[[Image:Education picture.jpg|637x637px]] | |||
The physiotherapist plays a crucial role in: | |||
<br> | # Educating patients regarding physical activity, exercise prescription and selection of appropriate activities<ref name="Heijnen 1993">Heijnen L. Rehabilitation and the role of the physical therapist. Southeast Asian J Trop Med Public Health 1993;24(Suppl. 1):26–9. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3570911/ (accessed 25 Sept 2015).</ref>. | ||
# Ensuring patients, relatives and peers are made aware of the positive impact physical activity can have, helping to prevent joint damage and functional impairment<ref name="Buzzard 1997">Buzzard B. Physiotherapy for Prevention and Treatment of Chronic Haemophilic Synovitis. Clinical Orthopaedics and Related Research. Orthopaedics and Related Research 1997;343:42-46. http://www.ncbi.nlm.nih.gov/pubmed/9345204 (accessed 9 Jan 2016).</ref>. Individuals who regularly exercise will also experience fewer bleeds<ref name="Tiktinsky 2002">Tiktinsky R, Falk B, Heim M, Martinovitz U. The effect of resistance training on the frequency of bleeding in haemophilia patients: a pilot study. Haemophilia 2002;8:22–7. http://www.ncbi.nlm.nih.gov/pubmed/11886461 (accessed 15 Dec 2015).</ref>. | |||
# Informing patients that just as with healthy individuals, exercise has various benefits. Additional benefits such as enhanced lean tissue mass, improved fitness and strength and a decrease in body fat percentage are apparent during puberty in adolescents<ref>U.S. Department of Health and Human Services. Physical Activity Guidelines Advisory Committee report. http://health.gov/paguidelines/report/pdf/committeereport.pdf (accessed 17 Jan 2016).</ref><span style="line-height: 1.5em; font-size: 13.28px;">.</span> | |||
# Advising them to attempt non-contact sports such as swimming, walking, cycling, golf, archery, badminton, rowing and sailing in place of contact sports like rugby <ref name="WFH guidelines">World Federation of Hemophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd. 2012;2:6-73. 2012. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 Oct 2015).</ref>. | |||
# Working in conjunction with the medical team when advising timing of prophylaxis appropriate to their chosen sport or activity<ref name="McGee">McGee S et al. Organized sports participation and the association with injury in paediatric patients with haemophilia. Haemophilia 2015;21(4):538-542. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2786948/ (accessed 15 Nov 2015).</ref>;<ref name="WFH GUIDELINES">World Federation of Heamophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd 2012;2:6-73. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 Oct 2015).</ref>. | |||
# Educating on and encouraging the use of protective equipment e.g if patient has a target joint, or does not take prophylaxis prior to activity <ref name="Philpott et al. 2010">Philpott J, Houghton K, Luke A. Physical activity recommendations for children with specific chronic health conditions: Juvenile idiopathic arthritis, hemophilia, asthma and cystic fibrosis. Paediatrics Child Health 2010;15(4):213-218. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2866314/ fckLR(accessed 6 Oct 2015).</ref>. Protective equipment is discussed later in the module. | |||
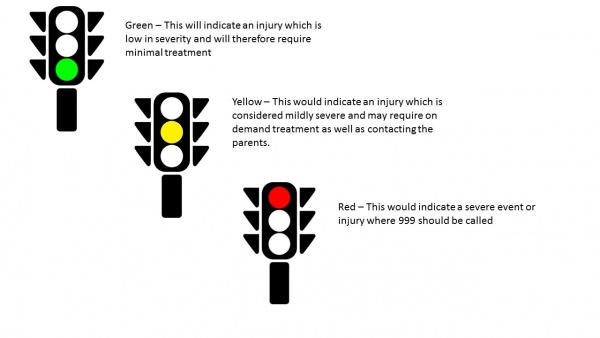
# Educating school personnel regarding suitable activities for the child, discussing immediate care in case of a bleed, and explaining modifications in activities that may be necessary following bleeds<ref name="WFH GUIDELINES" />. <br>Some parents have found a traffic light coding system beneficial to inform teachers at school of the appropriate actions to take in event of specific injuries or bleed. This is also alluded to in the “get fit and active” video later in the module.<br><br> | |||
Figure 10. Traffic light system | |||
<br> | [[Image:Traffic lights.jpg|center|600px]]<br> <br> | ||
=== Physical Activity Promotion === | |||
' | It is believed that physical activity in this population is reduced compared to healthy age-matched peers<ref name="Darby et al. 2007">Darby SC, Wan Kan S, Spooner RJ, Giangrande PLF, Hill FGH, Hay CRM, Lee CA, Ludlam CA, Williams M. Mortality rates, life expectancy, and causes of death in people with hemophilia A or B in the United Kingdom who were not infected with HIV. Blood 2007;110(3):815-825. :http://www.bloodjournal.org/content/110/3/815?sso-checked=true (accessed 2 Jan 2016).</ref>. The Kings Fund<ref name="The Kings Fund">The Kings Fund. Inequalities in life expectancy Changes over time and implications for policy. http://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/inequalities-in-life-expectancy-kings-fund-aug15.pdf (accessed 24 Nov 2015).</ref> acknowledge health behaviour patterns to impact an individual's overall health by as much as 40%, when compared to healthcare which contributes only 10%. Therefore, as Physiotherapists, our role in health and activity promotion is crucial in order to influence positive behavioural change to impact upon health<ref>Chartered Society of Physiotherapy. Physio 15: Physios can improve public health by influencing behaviour and promoting physical activity. http://www.csp.org.uk/news/2015/10/21/physio-15-physios-can-improve-public-health-influencing-behaviour-promoting-physical (accessed 27 Nov 2015).</ref>. | ||
< | Health promotion involves supporting people to gain control and responsibility over improving their own health. It extends beyond focusing on individual behaviour and includes a variety of social and environmental interventions<ref>World Health Organization. Health Promotion. http://www.who.int/topics/health_promotion/en/ (accessed 28 Dec 2015).</ref>. | ||
< | The Corporate Policy and Strategy Committee have introduced a Physical Activity for Health Pledge which the NHS is engaging with. This pledge involves ensuring primary care staff have the necessary skills and resources available to assess physical activity levels. It also ensures they offer education detailing recommended minimum requirements for physical activity, brief advice and intervention, along with increasing awareness of available community resources. Unpublished data from NHS Health Scotland reveals only 13% of primary care practitioners are presently aware of the recommended weekly activity levels <ref name="Corporate Policy and Strategy Committee 2015">Corporate Policy and Strategy Committee. Physical Activity for Health Pledge. 2-12 www.edinburgh.gov.uk (accessed 8 Oct 2015).</ref>. It can therefore be assumed this is not currently being promoted effectively. | ||
The following video [https://www.youtube.com/watch?v=aUaInS6HIGo "23 and a 1/2 hours"] strongly promotes physical activity for at least 30 minutes of your day. Although not specific to the haemophilic population, the take home message can be followed for AWH. | |||
< | Although various studies have described the benefits of engaging in physical activity for people with haemophilia (PWH), results from research conducted in the USA among adolescent haemophilia patients have demonstrated a lack of knowledge concerning the role of physical activity in managing their condition<ref>Nazzaro AM, Owens S, Hoots WK, Larson KL. Knowledge, attitudes, and behaviors of youths in the US hemophilia population: results of a national survey. American Journal of Public Health 2006;96(9):1618-1622. http://www.ncbi.nlm.nih.gov/pubmed/16873741 (accessed 3 Jan 2016).</ref>. Whilst it is recognised this information is important, this study has not been conducted in the UK so results must be generalised with caution. However, this suggests more work must be done to promote physical activity and emphasise its positive role in enhancing the lives of PWH <ref name="Negrier et al. 2013">Negrier C, Seuser A, Forsyth A, Lobet S, Llinas A, Roas M, Heijnen L. The benefits of exercise for patients with haemophilia and recommendations for safe and effective physical activity. Haemophilia 2013;19(4):487-498. http://www.ncbi.nlm.nih.gov/pubmed/23534844 (accessed 7 Jan 2016).</ref>. | ||
<br> | Physical activity promotion for health exists worldwide <ref name="Heath et al. 2012">Heath GW, Parra DC, Sarmiento OL, Andersen LB, Owen N, Goenka S, Montes F, Brownson RC. Evidence-based intervention in physical activity: lessons from around the world. Lancet 2012; 380(9838):272-81. http://www.ncbi.nlm.nih.gov/pubmed/22818939 (accessed 26 Jan 2016).</ref>. The benefits of such in the general population are widely known, providing health improvements along with the potential for enhancing disease outcomes<ref>World Health Organization. Health Promotion. http://www.who.int/topics/health_promotion/en/ (accessed 28 Dec 2015).</ref>. National and international guideliness set out clear recommendations on the physical activity levels required to promote health<ref name="Department of Health">Department of Health. Multidisciplinary teams (MDT’s). http://www.health.nt.gov.au/Cancer_Services/CanNET_NT/Multidisciplinary_Teams/index.aspx (accessed 7 Jan 2016).</ref>. Although many studies have reported the benefits of participation in physical activity for PWH, researchers in the USA have identified a lack of knowledge among young haemophilia patients (aged 13–18 years) as to the role of exercise in the management of their condition. | ||
=== Physical Activity - Associated Risks and Considerations === | |||
As physiotherapists it is vital to be aware of risks and considerations when advising patients to participate in physical activity or exercise. <br><br>Knowing whether patients have target joint bleeds allows the physiotherapist to adapt and alter their advice and treatment plan. Discussion can then be made around the use of protective equipment for the target joint, or whether there are any other activities which may reduce the risk of contact involving that specific joint. <br><br>It is important to know when the patient’s last acute bleed was and where. Activity must be gradually re-introduced following a bleed to minimise the chance of it reoccurring<ref>World Federation of Haemophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd 2012;2:6-73. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 Oct 2015).</ref>.<br><br>Appropriate timing of prophylaxis treatment surrounding physical activity is critical when striving to prevent bleeds. Prophylaxis should be individualised and taken to coincide with exercise. The aim being the factor will be at its peak during the period of activity<ref>Anderson A, Forsyth A. Playing it safe: Bleeding Disorders, Sport and Exercise New York: National Haemophilia Foundation. 1- 44. https://www.hemophilia.org/…/docume…/files/PlayingItSafe.pdf (accessed 6 Oct 2015).</ref>. This will minimise the risk or potential for bleeds<ref>World Federation of Haemophilia. About bleeding disorders. http://www.wfh.org/en/page.aspx?pid=642 (accessed 7 Jan 2016).</ref>. As discussed previously, physiotherapists must be aware of this and communicate with the patient’s medical team regarding best advice. | |||
==== Exercising with Inhibitors ==== | |||
< | Approximately 30% of patients with haemophilia will develop an immune response to medications used to treat the condition. If this occurs an alternative treatment may be necessary to manage bleeds. Immune tolerance therapy is introduced which aims to help the individual become accustomed to the factor<ref>The Haemophilia Society. Inhibitors. http://www.haemophilia.org.uk/bleeding_disorders/bleeding_disorders/inhibitors (accessed 26 Jan 2016).</ref>. | ||
< | Individuals with inhibitors may initially be apprehensive towards engaging in activity and exercise, causing their physical condition to rapidly decline. A program consisting of active range of motion, isometric and isotonic strengthening along with balance exercises can facilitate function and help to maintain independence<ref>Caviglia H, Narayan P, Forsyth A, Giangrande P, Gilbert M, Goddard N, Mulder K, Rahima S. Musculoskeletal problems in persons with inhibitors: How do we treat?. Haemophilia 2012;18(4):54-60. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2012.02874.x/epdf (accessed 26 Jan 2016).</ref>. | ||
=== Guidelines and Recommendations === | |||
It is important to note that the recommended guidelines for physical activity in children with haemophilia are the same as those advised for healthy individuals. Government-issued guidelines exist for children and young people aged 4 – 18. These guidelines state that this age group should be participating in 60 minutes of moderate to vigorous activity each day. Vigorous activity, which strengthens muscle and bone, should take place at least 3 times a week<ref>Department of Health. Physical Activity Guidelines for Children and Young People. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213739/dh_128144.pdf (accessed 10 Oct 2016).</ref>.<br>The World Haemophilia Federation<ref>World Federation of Heamophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd 2012;2:6-73. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 Oct 2015).</ref> has released updated guidelines for the management of people with haemophilia: | |||
*The primary aim of management is to prevent and treat bleeds | |||
*Comprehensive care aims to promote health physically and psychosocially, as well as improving quality of life and reducing morbidity and mortality. Physiotherapists may play a more significant role in this aspect compared to managing the more acute phase of a bleed. Physiotherapy involvement contributes to both the prevention and treatment of bleeds. | |||
*Children and adolescents should be reviewed every 6 months by a physiotherapist for assessment and management planning | |||
*Physiotherapy has a main role in promoting physical activity: to improve fitness, neuromuscular development, strengthening, coordination, functioning, weight management and self esteem | |||
*Weight bearing activities should be encouraged to enhance bone mineral accrural | |||
*A physical activity plan should be tailored to individuals preference, abilities and considering the severity of their condition | |||
*Non-contact sports will be encouraged – i.e. swimming, walking, golf, badminton, cycling, table tennis | |||
*Contact sports and high velocity sports are strongly discouraged due to the risk of a fatal bleed – i.e. rugby, boxing, wrestling, racing, skiing | |||
*Target joints can be protected using braces or splints during activities | |||
*Following a bleed the activity should be reintroduced gradually to minimise the risk of re-bleeding | |||
*Adjunctive management is also vital to physiotherapy. This means activity should be undertaken in conjunction with factor replacement. Physiotherapy can also help to reduce the amount of factor required. | |||
*In the acute phase, PRICE will be used by the physiotherapist | |||
*Following this, rehabilitation is required to restore function | |||
<br> "Playing it Safe"<ref>National Haemophilia Foundation. Play it Safe. https://www.hemophilia.org/sites/default/files/document/files/PlayingItSafe.pdf (accessed 20 Oct 2015).</ref> is an online document which provides recommendations and advice regarding participation in sport and exercise when suffering with a bleeding disorder. | |||
<br> | |||
=== Personal Protective Equipment === | === Personal Protective Equipment === | ||
<br>Protective equipment can be worn by individuals to minimise risk of bleeding either | <br>Protective equipment can be worn by individuals to minimise the risk of bleeding either at a very young age or when taking part in sports and activities at an older age<ref>Cassis FRMY. Treatment of Haemophilia. Psychosocial Care for people with Haemophilia 2007;1-12. https://haemophilia.ie/PDF/Psychosocial-Care.pdf (accessed 10 Jan 2016).</ref>. This is generally used considering personal preference, the child’s compliance and the level of sporting activity undertaken. Splints or braces can be useful in protecting target joints whilst participating in sports<ref>World Federation of Haemophilia. About bleeding disorders. http://www.wfh.org/en/page.aspx?pid=642 (accessed 7 Jan 2016).</ref>. | ||
Joints which are considered at high risk of bleeds are the elbows, wrists, knees and ankles. Toddlers are encouraged to be protected with elbow and knee pads when crawling and helmets can also be used to protect children from falls, especially when cycling or running. Due to the introduction and advances in prophylaxis, the need for protective equipment in day to day activities has been reduced. It is suggested that although previously considered extremely important and beneficial, the social risks now outweigh the potential benefits of protective equipment. However, this is a decision that must be made based on the type and competitiveness of the activity the individual is participating in. | |||
There are many different types of protective equipment available and multiple ways of modifying home environments to make it safer for toddlers and young children. | |||
=== How to Approach Conversations Regarding Physical Activity === | === How to Approach Conversations Regarding Physical Activity === | ||
It can sometimes be difficult for | It can sometimes be difficult for physiotherapists to approach the subject of physical activity with an individual and encouraging behavioural change can be increasingly difficult in AWH. This is due to the nature of the condition as this is normally a stage in their life where physical activity levels reduce<ref>Majumdar S, Morris A, Gordon C, Kermode CJ, Forsythe A, Herrington B, Megason GC, Iyar R. Alarmingly high prevalence of obesity in haemophilia in the state of Mississippi. Haemophilia 2010;16;455-459. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2009.02187.x/epdf (accessed 28 Jan 2016).</ref><span style="line-height: 1.5em; font-size: 13.28px; font-weight: normal;">.</span> Physiotherapists can offer education and advice about what type of activity to undertake in order to prevent bleeds occurring.<br>Appropriate communication is essential when discussing physical activity with patients. The Royal College of General Practitioners<ref name="Royal College of General Practitioners">Royal College of General Practitioners. Health literacy: report from an RCGP-led health literacy workshop. http://www.rcgp.org.uk/clinical-and-research/a-to-z-clinical-resources/~/media/Files/CIRC/Health-Literacy-Report/Health%20Literacy%20Final%20edition%2029%2007%202014.ashx (accessed 20 Nov 2015).</ref> makes recommendations on how to appropriately communicate ideas to a patient. | ||
< | |||
== Benefits of Physical Activity == | == Benefits of Physical Activity == | ||
The | The video below offers some general advice and recommendations regarding increasing physical activity in PWH. It follows the story of Sean, an individual with haemophilia, as he discusses some of the benefits he believes are associated with being physically active when living with this condition. {{#ev:youtube|7wSlRbwqiE8}}<br>Video used with permission from Clinical Specialist Physiotherapist, Jenna Reid. | ||
=== Physical Activity Relating to Obesity === | |||
Childhood obesity is prevalent in AWH, as well as the general population. However, the consequences of weight gain in sufferers can cause additional issues, such as increased risk of joint arthropathy<ref name="Young">Young G. New challenges in hemophilia: long-term outcomes and complications. Hematology 2012;1:362 - 368. http://asheducationbook.hematologylibrary.org/…/362.full.pd… (accessed 26 Oct 2015).</ref>. Excess weight can induce joint bleeds due to added stresses placed on the joints <ref name="Tuinenburg et al. 2013">Tuinenburg A, Biere-rafi S, Peters M, Verhamme P, Peerlinck K, Kruip MJHA, Laros-van Gorkom BAP, Roest M, Meijers JCM, Kamphuisen PW, Schutgens REG. Obesity in haemophilia patients: effect on bleeding frequency, clotting factor concentrate usage, and haemostatic and fibrinolytic parameters. Haemophilia 2013;(19):744-752. http://www.pfizerpro.com.co/sites/g/files/g10017511/f/publicaciones/092013%20V19%20I5%20-Obesity%20in%20haemophilia%20patients%20effect%20on%20bleeding%20frequency,%20clotting%20factor%20concentrate%20usage,%20and%20haemostatic%20and%20fibrinolytic%20parameters.pdf (accessed 2 Dec 2015).</ref>. Effects of obesity and overweight can also exacerbate existing arthropathies and influence development of cardiovascular disease<ref>Douma-van Riet DMC, Engelbert RHH, Van Genderen FR, Horst-De Ronde MTM, Goede-Bolders A, Hartman A. Physical fitness in children with haemophilia and the effect of overweight. Haemophilia 2009;15:519-527. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2008.01928.x/epdf (accessed 22 Jan 2016).</ref>. | |||
== | Parental influence is also considered to be a contributing factor to obesity and overweight in this population. Many parents tend to be very protective of their child, preventing them from engaging in physical activity. It was not until the 1970s that exercise in this population was recognised as effective. Prior to this it was considered to increase the risk of haemarthroses<ref name="Broderick et al. 2006">Broderick CR, Herbert RD, Latimer J, Curtin JA, Selvadurai HC. The Effect Of An Exercise Intervention On Aerobic Fitness, Strength and Quality of life in children with Haemophilia. BMC Blood Disorders 2006;6:2. http://www.biomedcentral.com/content/pdf/1471-2326-6-2.pdf (accessed 9 Oct 2015).</ref>. A previously discussed, it is now recommended for particular activities, mainly swimming, with aims of improved quality of life. This new treatment approach is largely due to recent advances in safety and availability in the clotting factor used to prevent bleeds<ref name="Querol et al. 2010">Querol F, Perez-alendaa S, Gallachc JE, Devis-devis J, Valencia-peris A, Gonzalez Moreno LM. Haemophilia: exercise and sport. Apunts Med Esport 2010;46(165:29-39. http://www.elsevier.es/…/277/277v46n169a90001817pdf001_2.pdf (accessed 15 Oct 2015)</ref>. Buzzard and Beeton<ref>Buzzard B, Beeton K. Physiotherapy Management of Haemophilia. Oxford: Wiley, 2008.</ref> also report evidence to suggest changes in blood clotting factors due to exercise. | ||
A study conducted | The benefits of physical activity in the general population are widely known, providing general health improvements along with potential enhancement in disease outcomes<ref>Durstine JL, Gordon B, Wang Z, Luo X. Chronic disease and the link to physical activity. Journal of Sport and Health Science 2013;2(1)3-11. http://www.sciencedirect.com/science/article/pii/S2095254612000701 (accessed 13 Dec 2015).</ref>. However, Philpott et al.<ref name="Philpott et al. 2010" /> believe children suffering with a chronic disease or disability are less active than their age-matched healthy peers. A study conducted by Hofstede et al.<ref name="Hofstede et al. 2008">Hofstede FG, Fijnvandraat K, Plug I, Kamphuisen PW, Rosendaal FR, Peters M. Obesity: a new disaster for haemophiliac patients? A nationwide survey. Haemophilia 2008;14:1035-1038. http://onlinelibrary.wiley.com/…/j.1365-2516.2008.01806.x.p… (accessed 30 Sept 2015).</ref> comparing healthy subjects to AWH reiterates; revealing triple the number of obese boys with haemophilia in relation to the comparable healthy subjects. Contrary to this finding, a 2010 study quantifying physical activity levels through accelerometry, revealed AWH to be more involved in physical activity compared to their healthy peers. However, the study also stated the time dedicated to physical activity was mainly focused towards low-intensity activities and sedentary behaviours<ref name="Buxbaum et al. 2010">Buxbaum NP, Ponce P, Saidi P, Michaels LA. Psychosocial correlates of physical activity in adolescents with haemophilia. Haemophilia. 2010;16:656-61. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2010.02217.x/epdf. (accessed 21 Jan 2016).</ref>. Several studies have reported an association between an increase in obesity levels and sedentary behaviours particularly amoung AWH. This increase is concerning, however does not differ much from the un-affected population<ref>Hofstede FG, Fijnvandraat K, Plug I, Kamphuisen PW, Rosendaal FR, Peters M. Obesity: a new disaster for haemophiliac patients? A nationwide survey. Haemophilia 2008;14:1035-1038. http://onlinelibrary.wiley.com/…/j.1365-2516.2008.01806.x.p… (accessed 30 Sept 2015).</ref>;<ref>Douma-van Riet DMC, Engelbert RHH, Van Genderen FR, Horst-De Ronde MTM, Goede-Bolders A, Hartman A. Physical fitness in children with haemophilia and the effect of overweight. Haemophilia 2009;15:519-527. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2008.01928.x/epdf (accessed 22 Jan 2016).</ref>. | ||
= | The overall consensus, as previous stated, is that an accumulation of 60 minutes or more physical activity of moderate intensity, consisting of both aerobic daily activity and vigorous intensity aerobic activity across a minimum of 3 days per week is advised <ref name="Licence 2004">Licence K. Promoting and protecting the health of children and young people. Child: care, health and development 2004;30(6):623-635. http://onlinelibrary.wiley.com/enhanced/doi/10.1111/j.1365-2214.2004.00473.x (accessed 22 Jan 2016).</ref>. However, the physical activity recommendations remain limited<ref>Beardsley DS. Sport and Exercise for children with chronic health conditions. Champaign IL:Human Kinetics 1995:302-9.</ref>;<ref name="Buzzard 1996">Buzzard BM. Sports and haemophilia: antagonist or protagonist. Clinical Orthopaedics and Related Research 1996;328:25-30. http://www.ncbi.nlm.nih.gov/pubmed/8653965 (accessed 19 Jan 2016).</ref>, with findings from recent studies demonstrating controversial outcomes. | ||
==== Childhood Development ==== | |||
Adolescents undergo more physical changes at this age than throughout any other stage of their life. The rate of growth in itself can predispose the child to bleeds. Growth spurts around puberty may decrease the muscle mass surrounding joints and consequently increase joint bleeding during this period<ref name="Johnson et al. 2013">Johnson MJ, Gorlin JB. Child Development with a Bleeding Disorder and Transition. New York: National Hemophilia Foundation 2013:1-16. https://www.hemophilia.org/…/Nurses-Guide-Chapter-13a-Child… (accessed 10 Oct 2015).</ref>. | |||
Weight-bearing activities are crucial in ensuring adequate generation of bone mass throughout childhood and may be even be considered more important than calcium intake through diet<ref name="Barnes et al. 2004">Barnes C, Wong P, Egan B, Speller T, Cameron F, Jones G, Ekert H, Monagle P. Reduced Bone Density Among Children With Severe Hemophilia. Pediatrics 2004;114:2:e177-e181. http://www.ncbi.nlm.nih.gov/pubmed/15286254 (accessed 9 Oct 2015).</ref>. A study conducted in 2008, by Tlacuilo-Parra et al.<ref name="Tlacuilo-parra et al. 2008">Tlacuilo-parra A, Morales-zambrano R, Tostadorabago N, Esparza-Flores MA, Lopez-Guido B, Orozcalcala J. Inactivity is a risk factor for low bone mineral density among haemophilic children. British Journal of Haematology 2008;140:562-567 http://onlinelibrary.wiley.com/…/j.1365-2141.2007.06972.x.p… (accessed 8 Nov 2015).</ref> revealed a significant reduction in lumbar spine bone mineral density in children with haemophilia in comparison to healthy subjects of matched age and sex. The results demonstrated statistically significant differences in activity between the groups, with the haemophilia population at three times the risk of inactivity. These results confirm that long periods of inactivity and immobility, with reduced weight-bearing (such as following joint bleeds) are directly related to low bone mineral density in AWH. | |||
=== Psychosocial Factors Associated With Physical Activity === | |||
Due to the nature of the condition, AWH are usually diagnosed and aware of their condition from a very young age. Psychosocial, as well as physical barriers may exist in relation to participation in physical activity<ref name="ICF 2016">ICF. International Classification of Functioning, Disability and Health (ICF). http://www.who.int/classifications/icf/en/ (accessed 5 Jan 2016).</ref><span style="line-height: 1.5em; font-size: 13.28px;">.</span> | |||
<br> | <br><br>The World Federation of Haemophilia (WFH) separates a number of different psychosocial issues into specific age groups<ref>Cassis FRMY. Treatment of Haemophilia. Psychosocial Care for people with Haemophilia 2007;1-12. https://haemophilia.ie/PDF/Psychosocial-Care.pdf (accessed 10 Jan 2016).</ref>:<br> | ||
* Infant to toddler (newborn to age 5) | |||
* Early childhood (6-9 years) | |||
* Pre-adolescence (10-13 years) | |||
* Adolescence (14-17 years) | |||
* Adulthood (18 years +)<br> | |||
It is important that at every stage of the child’s journey there is help and support available to the individual and family to ensure that psychosocial barriers are minimised<ref>Cassis FRMY. Treatment of Haemophilia. Psychosocial Care for people with Haemophilia 2007;1-12. https://haemophilia.ie/PDF/Psychosocial-Care.pdf (accessed 10 Jan 2016).</ref>. Some of the psychosocial issues that are common in adolescence are discussed below.<br> | |||
==== Transition Phase ==== | |||
In the adolescence stage, there is a transition of care from paediatrics to general practitioners. During this period it is important to focus on self -management and increasing independence in treatment. Although this can increase confidence in self-treatment with greater control over their condition, a common issue at this age is compliance. | |||
Cassis | ==== Compliance ==== | ||
Cassis<ref>Cassis FRMY. Treatment of Haemophilia. Psychosocial Care for people with Haemophilia 2007;1-12. https://haemophilia.ie/PDF/Psychosocial-Care.pdf (accessed 12 Jan 2016).</ref> states that at this stage of development, teenagers are often focussed on present events and do not consider the long term consequences of poorly managing their condition. As a child begins to mature, other activities may take priority over physiotherapy or exercise therefore, it is important that they are aware of the harmful consequences associated with inactivity. | |||
Physical activity can play a large part in a child’s social and emotional well-being. Through team-based sports they learn how to work with other peers. Improved emotional status has also demonstrated marked clinical benefits with reported reductions in spontaneous bleeds<ref>Anderson A, Forsyth A. Playing it safe: Bleeding Disorders, Sport and Exercise New York: National Haemophilia Foundation. 1- 44. https://www.hemophilia.org/…/docume…/files/PlayingItSafe.pdf (accessed 6 Oct 2015).</ref>. | |||
< | Cassis et al.<ref>Cassis FR, Querol F, Forsyth A, Iorio A. Psychosocial aspects of haemophilia: a systematic review of methodologies and findings. Haemophilia 2012; 18:3:101-14. http://www.ncbi.nlm.nih.gov/pubmed/22059839. (accessed 22 Jan 2016).</ref> conducted a systematic review comparing 24 studies considering the psychosocial aspects concerned with haemophilia. Results demonstrated psychosocial factors to have a significant impact on quality of life for patients with chronic conditions such as haemophilia. One of the studies, found the most common stressor associated with psychological factors to be reductions in lifestyle activity, including sport. This may be due to fear of inducing a bleed through exercise, or the stigma associated with wearing protective equipment. | ||
< | The review also found that for PWH, participation in physical activites and sports will positively effect not only physical well-being but also self-esteem and social interactions. This is further supported by Sherlock<ref>Sherlock E, O’Donnell JS, White B, Blake C. Physical activity levels and participation in sports in Irish people with haemophilia. Haemophilia 2010;16:202-9. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2009.02111.x/epdf. (accessed 21 Jan 2016).</ref> who found that non-physical benefits of sporting activities included improved self-esteem and perceived social acceptance. It also supported the above view that quality of life in PWH is impaired by limitations in sporting activity. | ||
< | However, Buxaum et al.<ref>Buxbaum NP, Ponce P, Saidi P, Michaels LA. Psychocial correlates of physical activity in adolescents with haemophilia. Haemophilia 2010;16:656-61. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2010.02217.x/epdf. (accessed 21 Jan 2016).</ref> conducted a study which aimed to establish social and cognitive factors associated with exercise in PWH. All particpants were aged between 11 and 18. The 'Peirs Harris Childrens Concept Scale' and the 'Childrens Manifest Anxiety Scale' were used to measure self-esteem and anxiety, as these are self-reported scales results must be interpreted with caution. The study found no differences in outcomes when comparing PWH to healthy controls. This conflicts with previous evidence, however, due to its small sample size with only 17 recruits in the haemophilia group, this reduces power to detect significant differences. | ||
< | |||
Although results are well supported by similar small studies, it is evident that research into the psychosocial aspects of haemophilia is limited<ref>Cassis FR, Querol F, Forsyth A, Iorio A. Psychosocial aspects of haemophilia: a systematic review of methodologies and findings. Haemophilia 2012; 18:3:101-14. http://www.ncbi.nlm.nih.gov/pubmed/22059839. (accessed 22 Jan 2016).</ref> and participation in physical activity among PWH has not been well studied<ref>Buxbaum NP, Ponce P, Saidi P, Michaels LA. Psychocial correlates of physical activity in adolescents with haemophilia. Haemophilia 2010;16:656-61. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2010.02217.x/epdf. (accessed 21 Jan 2016).</ref>. | |||
== References == | |||
<references /> | <references /> | ||
[[Category:Queen_Margaret_University_Project]] | |||
[[Category:Physical_Activity]] | |||
[[Category:Blood Disorders]] | |||
[[Category:Paediatrics]] | |||
[[Category:Paediatrics - Conditions]] | |||
Latest revision as of 18:05, 3 January 2023
Original Editor - Caitlin MacRae, Hazel Burt, Steven Flett, Alex Leishman and Chloe Allan as part of the Queen Margaret University's Current and Emerging Roles in Physiotherapy Practice Project
Top Contributors - Caitlin MacRae, Hazel Burt, Alex Leishman, Chloe Allan, Kim Jackson, Steven flett, Rucha Gadgil, 127.0.0.1, Admin, Jane Hislop, Michelle Lee and Tarina van der Stockt
Introduction[edit | edit source]
Physical activity and exercise, are often used synonymously, however, physical activity is defined as “as any bodily movement produced by skeletal muscles that require energy expenditure” [1], and exercise is a subsection of physical activity, involving planned or structured activity which aims to improve or maintain physical fitness [2].
The physiotherapist's role in treating and managing adolescents with haemophilia (AWH) is extremely important, and recent developments within this profession have increased its value [3]. One of the key interventions involved in its treatment is the promotion of physical activity [4].
Definition[edit | edit source]
Haemophilia is a rare inherited disorder where blood in the body has an inability to produce sufficient clotting factor, a protein which controls bleeding [5]. This lack of clotting factor can lead to severe and prolonged bleeds which may cause permanent damage to the site of haemorrhage and surrounding tissues[6]. There are an estimated 6000 people living in the United Kingdom with the condition. It occurs mainly through a gene passed from parent to child on the X chromosome, i.e. it mainly affects males[7].
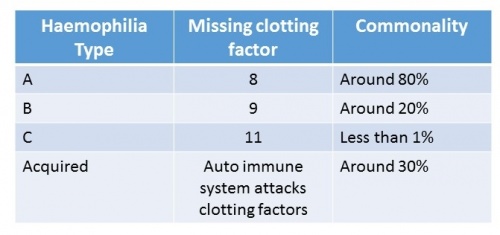
There are four main types of haemophilia. The table below shows the missing clotting factor and commonality for each type:
- Haemophilia A is the most common type affecting around 80% of the haemophilic population[8]. This is where the individual will either have low levels of clotting factor eight or it is completely missing.
- Haemophilia B is less common. This is where clotting factor nine is either very low or is missing from the blood. Around 20% of PWH will have this type[9].
- Haemophilia C is ten times rarer than type A and differs from both A and B as it can present in both genders. However, this is extremely rare and can only occur when the mother and father are both carriers of the gene [10]. Individuals with type C will have low levels of clotting factor eleven, or this will be completed absent.
- Acquired Haemophilia is extremely rare. This type is not inherited in the same way, as it is an auto-immune disorder. This is where the body's immune system attacks the clotting factors. This condition can also affect both males and females [11].
Classifications and Severities[edit | edit source]
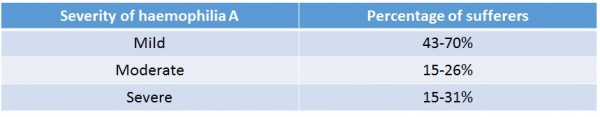
The table below categorises haemophilia into mild, moderate and severe, showing the percentage of sufferers in each category [12].
Like other disorders, haemophilia can affect individuals to varying degrees. The symptoms can be mild, moderate or severe, depending on the level of clotting factor present[13].
Multidisciplinary Team Involvement [edit | edit source]
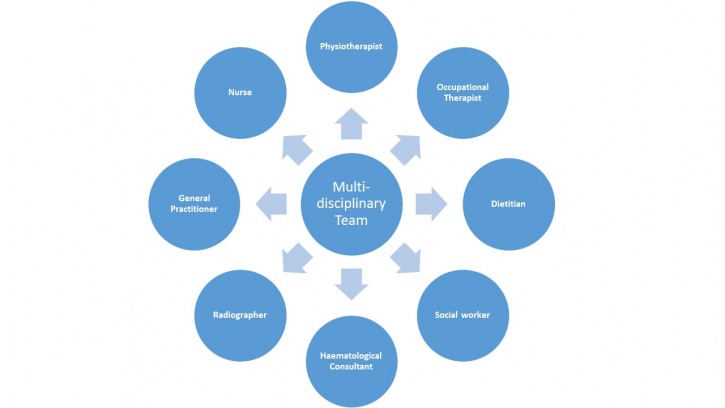
Despite recent development in the management of the condition, patients still require comprehensive multidisciplinary care throughout all stages of their life [14]. A multidisciplinary team involves a range of professionals who collaborate together to structure a treatment plan for an individual, aiming to achieve high quality patient-centered care [15].
The collaboration of all professionals allows a holistic approach to be considered which takes into account the individual’s physical, social, emotional, cultural and spiritual needs [16]. This is especially important during the transition from childhood into adulthood which can cause additional stress for those with chronic disorders. Therefore during this time they need for the MDT to work together is essential [14]. This may mean referring the patient to another team member to allow high-quality treatment, specific to the patients needs.
The Role of the Physiotherapist[edit | edit source]
Assessment[edit | edit source]
When assessing a patients condition or evaluating the success of interventions it is often beneficial for the physiotherapist to use a standardised outcome measure. These offer an objective measure which can help to monitor change in a patients symptoms[17].
Symptoms of a joint bleed may include swollen and hot joints, pain in the area and stiffness when mobilising. Many patients have described the overall feeling as an 'aura' surrounding the joint[18], for example swelling in the knee during a joint bleed.
Outcome Measures:[edit | edit source]
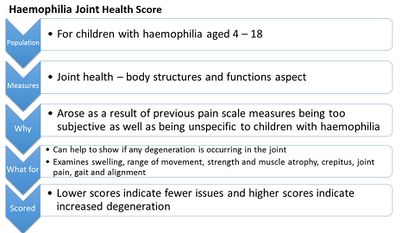
'The Haemophilia Joint Health Score' [19] is designed for physiotherapists and recommended for use by professionals specialised in haemophilia treatment. The outcome measure takes approximately 45 – 60 minutes to complete and is designed specifically for children with haemophilia. It examines the condition of a joint affected by a bleed and can be used to demonstrate degeneration in a joint over time.
The 'Paediatric Haemophilia Activities List’ is another outcome measure used for individuals with haemophilia. Adolescents will complete the child/teenager version explaining to what extent their haemophilia impacts upon their daily activities The questionnaire can then be used by healthcare professionals involved in their care[20].
Although outcome measures exist for the assessment of children with haemophilia many of these have demonstrated poor validity and reliability[21].
Management[edit | edit source]
The main role of the physiotherapist when treating an AWH involves the management of impairments from a musculoskeletal perspective, aiming to restore and improve function. Some of these include: haemarthoses, synovitis, joint contractures, haemotomas and haemophilic arthropathys[22].
During the acute phase, the physiotherapist will attempt to minimise bleeding using the PRICE regime (protection, rest, ice, compression elevation)[23]. This will also work in conjunction with factor replacement if necessary.
Following the acute phase, the physiotherapy management will focus on regaining full range of movement, muscle strength and reducing pain[24]. As soon as the pain and swelling begin to decrease, the patient should be encouraged to gradually increase the joint range aiming to achieve complete extension. This should be done actively by the patient to encourage muscle contraction, however passive movements may initially be used. It is vital that early active muscle control occurs to prevent the loss of joint movement [25];[26];[27]. Rehabilitation involving active exercises and proprioceptive training must then be continued until full pre-bleed joint ROM and function is restored [28].
Another key role of the physiotherapist when treating an AWH is promotion of physical activity. Exercise is encouraged as it will improve the child’s fitness, reduce obesity levels, improve muscular strength, and reduce frequency of bleeding episodes and joint deterioration [29]. The World Federation of Haemophilia[30] advise particular focus towards strengthening, co-ordination, achieving a healthy body weight and improving self-esteem. As well as the physical aspects concerned, a major aspect of physiotherapy management focuses on education and advice.
Education[edit | edit source]
Below is a mind map which summarises key points regarding the advice that should be offered to patients around physical activity.
The physiotherapist plays a crucial role in:
- Educating patients regarding physical activity, exercise prescription and selection of appropriate activities[31].
- Ensuring patients, relatives and peers are made aware of the positive impact physical activity can have, helping to prevent joint damage and functional impairment[32]. Individuals who regularly exercise will also experience fewer bleeds[33].
- Informing patients that just as with healthy individuals, exercise has various benefits. Additional benefits such as enhanced lean tissue mass, improved fitness and strength and a decrease in body fat percentage are apparent during puberty in adolescents[34].
- Advising them to attempt non-contact sports such as swimming, walking, cycling, golf, archery, badminton, rowing and sailing in place of contact sports like rugby [35].
- Working in conjunction with the medical team when advising timing of prophylaxis appropriate to their chosen sport or activity[36];[37].
- Educating on and encouraging the use of protective equipment e.g if patient has a target joint, or does not take prophylaxis prior to activity [38]. Protective equipment is discussed later in the module.
- Educating school personnel regarding suitable activities for the child, discussing immediate care in case of a bleed, and explaining modifications in activities that may be necessary following bleeds[37].
Some parents have found a traffic light coding system beneficial to inform teachers at school of the appropriate actions to take in event of specific injuries or bleed. This is also alluded to in the “get fit and active” video later in the module.
Figure 10. Traffic light system
Physical Activity Promotion[edit | edit source]
It is believed that physical activity in this population is reduced compared to healthy age-matched peers[39]. The Kings Fund[40] acknowledge health behaviour patterns to impact an individual's overall health by as much as 40%, when compared to healthcare which contributes only 10%. Therefore, as Physiotherapists, our role in health and activity promotion is crucial in order to influence positive behavioural change to impact upon health[41].
Health promotion involves supporting people to gain control and responsibility over improving their own health. It extends beyond focusing on individual behaviour and includes a variety of social and environmental interventions[42].
The Corporate Policy and Strategy Committee have introduced a Physical Activity for Health Pledge which the NHS is engaging with. This pledge involves ensuring primary care staff have the necessary skills and resources available to assess physical activity levels. It also ensures they offer education detailing recommended minimum requirements for physical activity, brief advice and intervention, along with increasing awareness of available community resources. Unpublished data from NHS Health Scotland reveals only 13% of primary care practitioners are presently aware of the recommended weekly activity levels [43]. It can therefore be assumed this is not currently being promoted effectively.
The following video "23 and a 1/2 hours" strongly promotes physical activity for at least 30 minutes of your day. Although not specific to the haemophilic population, the take home message can be followed for AWH.
Although various studies have described the benefits of engaging in physical activity for people with haemophilia (PWH), results from research conducted in the USA among adolescent haemophilia patients have demonstrated a lack of knowledge concerning the role of physical activity in managing their condition[44]. Whilst it is recognised this information is important, this study has not been conducted in the UK so results must be generalised with caution. However, this suggests more work must be done to promote physical activity and emphasise its positive role in enhancing the lives of PWH [45].
Physical activity promotion for health exists worldwide [46]. The benefits of such in the general population are widely known, providing health improvements along with the potential for enhancing disease outcomes[47]. National and international guideliness set out clear recommendations on the physical activity levels required to promote health[48]. Although many studies have reported the benefits of participation in physical activity for PWH, researchers in the USA have identified a lack of knowledge among young haemophilia patients (aged 13–18 years) as to the role of exercise in the management of their condition.
Physical Activity - Associated Risks and Considerations[edit | edit source]
As physiotherapists it is vital to be aware of risks and considerations when advising patients to participate in physical activity or exercise.
Knowing whether patients have target joint bleeds allows the physiotherapist to adapt and alter their advice and treatment plan. Discussion can then be made around the use of protective equipment for the target joint, or whether there are any other activities which may reduce the risk of contact involving that specific joint.
It is important to know when the patient’s last acute bleed was and where. Activity must be gradually re-introduced following a bleed to minimise the chance of it reoccurring[49].
Appropriate timing of prophylaxis treatment surrounding physical activity is critical when striving to prevent bleeds. Prophylaxis should be individualised and taken to coincide with exercise. The aim being the factor will be at its peak during the period of activity[50]. This will minimise the risk or potential for bleeds[51]. As discussed previously, physiotherapists must be aware of this and communicate with the patient’s medical team regarding best advice.
Exercising with Inhibitors[edit | edit source]
Approximately 30% of patients with haemophilia will develop an immune response to medications used to treat the condition. If this occurs an alternative treatment may be necessary to manage bleeds. Immune tolerance therapy is introduced which aims to help the individual become accustomed to the factor[52].
Individuals with inhibitors may initially be apprehensive towards engaging in activity and exercise, causing their physical condition to rapidly decline. A program consisting of active range of motion, isometric and isotonic strengthening along with balance exercises can facilitate function and help to maintain independence[53].
Guidelines and Recommendations[edit | edit source]
It is important to note that the recommended guidelines for physical activity in children with haemophilia are the same as those advised for healthy individuals. Government-issued guidelines exist for children and young people aged 4 – 18. These guidelines state that this age group should be participating in 60 minutes of moderate to vigorous activity each day. Vigorous activity, which strengthens muscle and bone, should take place at least 3 times a week[54].
The World Haemophilia Federation[55] has released updated guidelines for the management of people with haemophilia:
- The primary aim of management is to prevent and treat bleeds
- Comprehensive care aims to promote health physically and psychosocially, as well as improving quality of life and reducing morbidity and mortality. Physiotherapists may play a more significant role in this aspect compared to managing the more acute phase of a bleed. Physiotherapy involvement contributes to both the prevention and treatment of bleeds.
- Children and adolescents should be reviewed every 6 months by a physiotherapist for assessment and management planning
- Physiotherapy has a main role in promoting physical activity: to improve fitness, neuromuscular development, strengthening, coordination, functioning, weight management and self esteem
- Weight bearing activities should be encouraged to enhance bone mineral accrural
- A physical activity plan should be tailored to individuals preference, abilities and considering the severity of their condition
- Non-contact sports will be encouraged – i.e. swimming, walking, golf, badminton, cycling, table tennis
- Contact sports and high velocity sports are strongly discouraged due to the risk of a fatal bleed – i.e. rugby, boxing, wrestling, racing, skiing
- Target joints can be protected using braces or splints during activities
- Following a bleed the activity should be reintroduced gradually to minimise the risk of re-bleeding
- Adjunctive management is also vital to physiotherapy. This means activity should be undertaken in conjunction with factor replacement. Physiotherapy can also help to reduce the amount of factor required.
- In the acute phase, PRICE will be used by the physiotherapist
- Following this, rehabilitation is required to restore function
"Playing it Safe"[56] is an online document which provides recommendations and advice regarding participation in sport and exercise when suffering with a bleeding disorder.
Personal Protective Equipment[edit | edit source]
Protective equipment can be worn by individuals to minimise the risk of bleeding either at a very young age or when taking part in sports and activities at an older age[57]. This is generally used considering personal preference, the child’s compliance and the level of sporting activity undertaken. Splints or braces can be useful in protecting target joints whilst participating in sports[58].
Joints which are considered at high risk of bleeds are the elbows, wrists, knees and ankles. Toddlers are encouraged to be protected with elbow and knee pads when crawling and helmets can also be used to protect children from falls, especially when cycling or running. Due to the introduction and advances in prophylaxis, the need for protective equipment in day to day activities has been reduced. It is suggested that although previously considered extremely important and beneficial, the social risks now outweigh the potential benefits of protective equipment. However, this is a decision that must be made based on the type and competitiveness of the activity the individual is participating in.
There are many different types of protective equipment available and multiple ways of modifying home environments to make it safer for toddlers and young children.
How to Approach Conversations Regarding Physical Activity[edit | edit source]
It can sometimes be difficult for physiotherapists to approach the subject of physical activity with an individual and encouraging behavioural change can be increasingly difficult in AWH. This is due to the nature of the condition as this is normally a stage in their life where physical activity levels reduce[59]. Physiotherapists can offer education and advice about what type of activity to undertake in order to prevent bleeds occurring.
Appropriate communication is essential when discussing physical activity with patients. The Royal College of General Practitioners[60] makes recommendations on how to appropriately communicate ideas to a patient.
Benefits of Physical Activity[edit | edit source]
The video below offers some general advice and recommendations regarding increasing physical activity in PWH. It follows the story of Sean, an individual with haemophilia, as he discusses some of the benefits he believes are associated with being physically active when living with this condition.
Video used with permission from Clinical Specialist Physiotherapist, Jenna Reid.
Physical Activity Relating to Obesity[edit | edit source]
Childhood obesity is prevalent in AWH, as well as the general population. However, the consequences of weight gain in sufferers can cause additional issues, such as increased risk of joint arthropathy[61]. Excess weight can induce joint bleeds due to added stresses placed on the joints [62]. Effects of obesity and overweight can also exacerbate existing arthropathies and influence development of cardiovascular disease[63].
Parental influence is also considered to be a contributing factor to obesity and overweight in this population. Many parents tend to be very protective of their child, preventing them from engaging in physical activity. It was not until the 1970s that exercise in this population was recognised as effective. Prior to this it was considered to increase the risk of haemarthroses[64]. A previously discussed, it is now recommended for particular activities, mainly swimming, with aims of improved quality of life. This new treatment approach is largely due to recent advances in safety and availability in the clotting factor used to prevent bleeds[65]. Buzzard and Beeton[66] also report evidence to suggest changes in blood clotting factors due to exercise.
The benefits of physical activity in the general population are widely known, providing general health improvements along with potential enhancement in disease outcomes[67]. However, Philpott et al.[38] believe children suffering with a chronic disease or disability are less active than their age-matched healthy peers. A study conducted by Hofstede et al.[68] comparing healthy subjects to AWH reiterates; revealing triple the number of obese boys with haemophilia in relation to the comparable healthy subjects. Contrary to this finding, a 2010 study quantifying physical activity levels through accelerometry, revealed AWH to be more involved in physical activity compared to their healthy peers. However, the study also stated the time dedicated to physical activity was mainly focused towards low-intensity activities and sedentary behaviours[69]. Several studies have reported an association between an increase in obesity levels and sedentary behaviours particularly amoung AWH. This increase is concerning, however does not differ much from the un-affected population[70];[71].
The overall consensus, as previous stated, is that an accumulation of 60 minutes or more physical activity of moderate intensity, consisting of both aerobic daily activity and vigorous intensity aerobic activity across a minimum of 3 days per week is advised [72]. However, the physical activity recommendations remain limited[73];[74], with findings from recent studies demonstrating controversial outcomes.
Childhood Development[edit | edit source]
Adolescents undergo more physical changes at this age than throughout any other stage of their life. The rate of growth in itself can predispose the child to bleeds. Growth spurts around puberty may decrease the muscle mass surrounding joints and consequently increase joint bleeding during this period[75].
Weight-bearing activities are crucial in ensuring adequate generation of bone mass throughout childhood and may be even be considered more important than calcium intake through diet[76]. A study conducted in 2008, by Tlacuilo-Parra et al.[77] revealed a significant reduction in lumbar spine bone mineral density in children with haemophilia in comparison to healthy subjects of matched age and sex. The results demonstrated statistically significant differences in activity between the groups, with the haemophilia population at three times the risk of inactivity. These results confirm that long periods of inactivity and immobility, with reduced weight-bearing (such as following joint bleeds) are directly related to low bone mineral density in AWH.
Psychosocial Factors Associated With Physical Activity[edit | edit source]
Due to the nature of the condition, AWH are usually diagnosed and aware of their condition from a very young age. Psychosocial, as well as physical barriers may exist in relation to participation in physical activity[78].
The World Federation of Haemophilia (WFH) separates a number of different psychosocial issues into specific age groups[79]:
- Infant to toddler (newborn to age 5)
- Early childhood (6-9 years)
- Pre-adolescence (10-13 years)
- Adolescence (14-17 years)
- Adulthood (18 years +)
It is important that at every stage of the child’s journey there is help and support available to the individual and family to ensure that psychosocial barriers are minimised[80]. Some of the psychosocial issues that are common in adolescence are discussed below.
Transition Phase[edit | edit source]
In the adolescence stage, there is a transition of care from paediatrics to general practitioners. During this period it is important to focus on self -management and increasing independence in treatment. Although this can increase confidence in self-treatment with greater control over their condition, a common issue at this age is compliance.
Compliance[edit | edit source]
Cassis[81] states that at this stage of development, teenagers are often focussed on present events and do not consider the long term consequences of poorly managing their condition. As a child begins to mature, other activities may take priority over physiotherapy or exercise therefore, it is important that they are aware of the harmful consequences associated with inactivity.
Physical activity can play a large part in a child’s social and emotional well-being. Through team-based sports they learn how to work with other peers. Improved emotional status has also demonstrated marked clinical benefits with reported reductions in spontaneous bleeds[82].
Cassis et al.[83] conducted a systematic review comparing 24 studies considering the psychosocial aspects concerned with haemophilia. Results demonstrated psychosocial factors to have a significant impact on quality of life for patients with chronic conditions such as haemophilia. One of the studies, found the most common stressor associated with psychological factors to be reductions in lifestyle activity, including sport. This may be due to fear of inducing a bleed through exercise, or the stigma associated with wearing protective equipment.
The review also found that for PWH, participation in physical activites and sports will positively effect not only physical well-being but also self-esteem and social interactions. This is further supported by Sherlock[84] who found that non-physical benefits of sporting activities included improved self-esteem and perceived social acceptance. It also supported the above view that quality of life in PWH is impaired by limitations in sporting activity.
However, Buxaum et al.[85] conducted a study which aimed to establish social and cognitive factors associated with exercise in PWH. All particpants were aged between 11 and 18. The 'Peirs Harris Childrens Concept Scale' and the 'Childrens Manifest Anxiety Scale' were used to measure self-esteem and anxiety, as these are self-reported scales results must be interpreted with caution. The study found no differences in outcomes when comparing PWH to healthy controls. This conflicts with previous evidence, however, due to its small sample size with only 17 recruits in the haemophilia group, this reduces power to detect significant differences.
Although results are well supported by similar small studies, it is evident that research into the psychosocial aspects of haemophilia is limited[86] and participation in physical activity among PWH has not been well studied[87].
References[edit | edit source]
- ↑ World Health Organization. Physical Activity. http://www.who.int/topics/physical_activity/en/ (accessed 25 January 2016).
- ↑ Casperson SJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public health Rep 1985;100;(2):126–131. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1424733/ (accessed 25 January 2016).
- ↑ Buzzard B, Beeton K. Physiotherapy Management of Haemophilia. Oxford: Wiley, 2008.
- ↑ World Federation of Heamophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd 2012;2:6-73. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 October 2015).
- ↑ NHS Choices. Haemophilia. http://www.nhs.uk/conditions/haemophilia/Pages/Introduction.aspx (accessed 7 Jan 2016).
- ↑ World Federation of Haemophilia. Severity of hemophilia. http://www.wfh.org/en/page.aspx?pid=643 (accessed 7 January 2016).
- ↑ Great Ormond Street Hospital. What causes Haemophilia? http://www.gosh.nhs.uk/medical-information/search-medical-conditions/haemophilia (accessed 10 Jan 2016).
- ↑ The Haemophilia Society. Haemophilia A.fckLRhttp://www.haemophilia.org.uk/bleeding_disorders/bleeding_disorders/haemophilia_a (accessed 9 November 2015).
- ↑ The Haemophilia Society. Haemophilia B. fckLRhttp://www.haemophilia.org.uk/bleeding_disorders/bleeding_disorders/haemophilia_fckLRb (accessed 9 November 2015).
- ↑ Haemophilia Information. Haemophilia Genetics. http://www.hemophilia-information.com/hemophilia-genetics.html (accessed 12 September 2015).
- ↑ Grethlein SJ. Acquired Haemophilia. http://emedicine.medscape.com/article/211186-overview#a2fckLR (accessed 7 January 2016).
- ↑ Preston FE, Kitchen S, Jennings L, Woods TA, Mackris M. SSC/ISTH classification of hemophilia A: can hemophilia center laboratories achieve the new criteria? J Thromb Haemost 2004;(2):271-4. http://www.ncbi.nlm.nih.gov/pubmed/14995989 (accessed 10 January 2016).
- ↑ NHS Choices. Haemophilia symptoms. http://www.nhs.uk/Conditions/Haemophilia/Pages/Symptoms.aspx (accessed 10 Jan 2016).
- ↑ 14.0 14.1 Breakey VR, Blanchette VS, Bolton-Maggs PHB. Towards comprehensive care in transition for young people with haemophilia. Haemophilia 2010;16(6):848-857. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2010.02249.x/abstract (accessed 18 Dec 2015).
- ↑ Department of Health. Multidisciplinary teams (MDT’s). http://www.health.nt.gov.au/Cancer_Services/CanNET_NT/Multidisciplinary_Teams/index.aspx (accessed 7 Jan 2016).
- ↑ Chartered Society of Physiotherapy. Physiotherapy works for social care – Why Physiotherapy? http://www.csp.org.uk/physiotherapy-works-social-care (accessed 10 Jan 2016).
- ↑ American Physical Therapy Association. Outcome Measures in Patient Care. http://www.apta.org/OutcomeMeasures/ (accessed 20 Jan 2016).
- ↑ Haemophilia Care. How to recognise a bleed. http://www.haemophiliacare.co.uk/how-to-recognise-a-bleed.html (accessed 7 Jan 2016)
- ↑ International Prophylaxis Study Group. HJHS. http://ipsg.ca/working-groups/physical-therapy/info/hjhs (accessed 15 Dec 2015).
- ↑ World Federation of Haemophilia, Paediatric Haemophilia Activities List: http://www.wfh.org/en/page.aspx?pid=886 (accessed 20 Oct 2015).
- ↑ Stephensen D, Drechsler WI, Scott OM. Outcome measures monitoring physical function in children with haemophilia: a systematic review. Haemophilia 2014;20:306-321. http://onlinelibrary.wiley.com/doi/10.1111/hae.12299/epdf (accessed 19 Jan 2016).
- ↑ Buzzard B, Beeton K. Physiotherapy Management of Haemophilia. Wiley-Blackwell, 2010.
- ↑ Haemophilia Care. How is Physiotherapy used in Haemophilia care. http://www.haemophiliacare.co.uk/physiotherapy.html (accessed 10 Oct 2015).
- ↑ Talking Joints. Let’s talk about physiotherapy for haemophilia patients. https://www.novonordisk.com/content/dam/Denmark/HQ/aboutus/documents/cpih-2015-talkingjoints-brochure-lets-talk-physiotherapy.pdf (accessed 10 Oct 2016).
- ↑ Hermans C, De Moerloose P, Fischer K, Holstein K, Klamroth R, Lambert T, Lavigne-Lissalde G, Perez R, Richards M, Dolan G. European Haemophilia Therapy Standardisation Board. Management of acute haemarthrosis in haemophilia A without inhibitors: literature review, European survey and recommendations. Haemophilia 2011;17(3):383-92. http://www.ncbi.nlm.nih.gov/pubmed/21323794 (accessed 30 Sept 2015).
- ↑ Gomis M, Querol F, Gallach JE, Gonzalez LM, Aznar JA. Exercise and sport in the treatment of haemophilic patients: a systematic review. Haemophilia 2009;15(1):43-54. http://www.ncbi.nlm.nih.gov/pubmed/18721151 (accessed 10 Jan 2016).
- ↑ Mulder K. Exercises for people with haemophilia. Montreal: World Federation of Haemophilia. 2006. http://scholar.google.co.uk/scholar_url?url=http%3A%2F%2Fhaemophilia.ie%2FPDF%2FExercise_Guide_med.pdf(accessed 22 Jan 2016).
- ↑ Heijnen L, Buzzard BB. The role of physical therapy and rehabilitation in the management of hemophilia in developing countries. Semin Thromb Hemost 2005;31(5):513-7. http://www.ncbi.nlm.nih.gov/pubmed/16276459 (accessed 25 Sept 2015).
- ↑ Blamey G, Forsyth A, Zourikian N, Short L, Jankovic N, Kleijn PDE, Flannery T. Comprehensive elements of a physiotherapy exercise program in haemophilia – a global perspective. World Federation of Haemophilia 2010;16:136-145 http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2010.02312.x/abstract;jsessionid=BB3B137A0C21342D378A949A977850CA.f04t01fckLR(accessed 10 Oct 2015).
- ↑ World Federation of Heamophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd 2012;2:6-73. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 Oct 2015).
- ↑ Heijnen L. Rehabilitation and the role of the physical therapist. Southeast Asian J Trop Med Public Health 1993;24(Suppl. 1):26–9. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3570911/ (accessed 25 Sept 2015).
- ↑ Buzzard B. Physiotherapy for Prevention and Treatment of Chronic Haemophilic Synovitis. Clinical Orthopaedics and Related Research. Orthopaedics and Related Research 1997;343:42-46. http://www.ncbi.nlm.nih.gov/pubmed/9345204 (accessed 9 Jan 2016).
- ↑ Tiktinsky R, Falk B, Heim M, Martinovitz U. The effect of resistance training on the frequency of bleeding in haemophilia patients: a pilot study. Haemophilia 2002;8:22–7. http://www.ncbi.nlm.nih.gov/pubmed/11886461 (accessed 15 Dec 2015).
- ↑ U.S. Department of Health and Human Services. Physical Activity Guidelines Advisory Committee report. http://health.gov/paguidelines/report/pdf/committeereport.pdf (accessed 17 Jan 2016).
- ↑ World Federation of Hemophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd. 2012;2:6-73. 2012. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 Oct 2015).
- ↑ McGee S et al. Organized sports participation and the association with injury in paediatric patients with haemophilia. Haemophilia 2015;21(4):538-542. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2786948/ (accessed 15 Nov 2015).
- ↑ 37.0 37.1 World Federation of Heamophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd 2012;2:6-73. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 Oct 2015).
- ↑ 38.0 38.1 Philpott J, Houghton K, Luke A. Physical activity recommendations for children with specific chronic health conditions: Juvenile idiopathic arthritis, hemophilia, asthma and cystic fibrosis. Paediatrics Child Health 2010;15(4):213-218. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2866314/ fckLR(accessed 6 Oct 2015).
- ↑ Darby SC, Wan Kan S, Spooner RJ, Giangrande PLF, Hill FGH, Hay CRM, Lee CA, Ludlam CA, Williams M. Mortality rates, life expectancy, and causes of death in people with hemophilia A or B in the United Kingdom who were not infected with HIV. Blood 2007;110(3):815-825. :http://www.bloodjournal.org/content/110/3/815?sso-checked=true (accessed 2 Jan 2016).
- ↑ The Kings Fund. Inequalities in life expectancy Changes over time and implications for policy. http://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/inequalities-in-life-expectancy-kings-fund-aug15.pdf (accessed 24 Nov 2015).
- ↑ Chartered Society of Physiotherapy. Physio 15: Physios can improve public health by influencing behaviour and promoting physical activity. http://www.csp.org.uk/news/2015/10/21/physio-15-physios-can-improve-public-health-influencing-behaviour-promoting-physical (accessed 27 Nov 2015).
- ↑ World Health Organization. Health Promotion. http://www.who.int/topics/health_promotion/en/ (accessed 28 Dec 2015).
- ↑ Corporate Policy and Strategy Committee. Physical Activity for Health Pledge. 2-12 www.edinburgh.gov.uk (accessed 8 Oct 2015).
- ↑ Nazzaro AM, Owens S, Hoots WK, Larson KL. Knowledge, attitudes, and behaviors of youths in the US hemophilia population: results of a national survey. American Journal of Public Health 2006;96(9):1618-1622. http://www.ncbi.nlm.nih.gov/pubmed/16873741 (accessed 3 Jan 2016).
- ↑ Negrier C, Seuser A, Forsyth A, Lobet S, Llinas A, Roas M, Heijnen L. The benefits of exercise for patients with haemophilia and recommendations for safe and effective physical activity. Haemophilia 2013;19(4):487-498. http://www.ncbi.nlm.nih.gov/pubmed/23534844 (accessed 7 Jan 2016).
- ↑ Heath GW, Parra DC, Sarmiento OL, Andersen LB, Owen N, Goenka S, Montes F, Brownson RC. Evidence-based intervention in physical activity: lessons from around the world. Lancet 2012; 380(9838):272-81. http://www.ncbi.nlm.nih.gov/pubmed/22818939 (accessed 26 Jan 2016).
- ↑ World Health Organization. Health Promotion. http://www.who.int/topics/health_promotion/en/ (accessed 28 Dec 2015).
- ↑ Department of Health. Multidisciplinary teams (MDT’s). http://www.health.nt.gov.au/Cancer_Services/CanNET_NT/Multidisciplinary_Teams/index.aspx (accessed 7 Jan 2016).
- ↑ World Federation of Haemophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd 2012;2:6-73. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 Oct 2015).
- ↑ Anderson A, Forsyth A. Playing it safe: Bleeding Disorders, Sport and Exercise New York: National Haemophilia Foundation. 1- 44. https://www.hemophilia.org/…/docume…/files/PlayingItSafe.pdf (accessed 6 Oct 2015).
- ↑ World Federation of Haemophilia. About bleeding disorders. http://www.wfh.org/en/page.aspx?pid=642 (accessed 7 Jan 2016).
- ↑ The Haemophilia Society. Inhibitors. http://www.haemophilia.org.uk/bleeding_disorders/bleeding_disorders/inhibitors (accessed 26 Jan 2016).
- ↑ Caviglia H, Narayan P, Forsyth A, Giangrande P, Gilbert M, Goddard N, Mulder K, Rahima S. Musculoskeletal problems in persons with inhibitors: How do we treat?. Haemophilia 2012;18(4):54-60. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2012.02874.x/epdf (accessed 26 Jan 2016).
- ↑ Department of Health. Physical Activity Guidelines for Children and Young People. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213739/dh_128144.pdf (accessed 10 Oct 2016).
- ↑ World Federation of Heamophilia. Guidelines for the Management of Haemophilia. Canada: Blackwell Publishing Ltd 2012;2:6-73. http://www1.wfh.org/publication/files/pdf-1472.pdf (accessed 2 Oct 2015).
- ↑ National Haemophilia Foundation. Play it Safe. https://www.hemophilia.org/sites/default/files/document/files/PlayingItSafe.pdf (accessed 20 Oct 2015).
- ↑ Cassis FRMY. Treatment of Haemophilia. Psychosocial Care for people with Haemophilia 2007;1-12. https://haemophilia.ie/PDF/Psychosocial-Care.pdf (accessed 10 Jan 2016).
- ↑ World Federation of Haemophilia. About bleeding disorders. http://www.wfh.org/en/page.aspx?pid=642 (accessed 7 Jan 2016).
- ↑ Majumdar S, Morris A, Gordon C, Kermode CJ, Forsythe A, Herrington B, Megason GC, Iyar R. Alarmingly high prevalence of obesity in haemophilia in the state of Mississippi. Haemophilia 2010;16;455-459. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2009.02187.x/epdf (accessed 28 Jan 2016).
- ↑ Royal College of General Practitioners. Health literacy: report from an RCGP-led health literacy workshop. http://www.rcgp.org.uk/clinical-and-research/a-to-z-clinical-resources/~/media/Files/CIRC/Health-Literacy-Report/Health%20Literacy%20Final%20edition%2029%2007%202014.ashx (accessed 20 Nov 2015).
- ↑ Young G. New challenges in hemophilia: long-term outcomes and complications. Hematology 2012;1:362 - 368. http://asheducationbook.hematologylibrary.org/…/362.full.pd… (accessed 26 Oct 2015).
- ↑ Tuinenburg A, Biere-rafi S, Peters M, Verhamme P, Peerlinck K, Kruip MJHA, Laros-van Gorkom BAP, Roest M, Meijers JCM, Kamphuisen PW, Schutgens REG. Obesity in haemophilia patients: effect on bleeding frequency, clotting factor concentrate usage, and haemostatic and fibrinolytic parameters. Haemophilia 2013;(19):744-752. http://www.pfizerpro.com.co/sites/g/files/g10017511/f/publicaciones/092013%20V19%20I5%20-Obesity%20in%20haemophilia%20patients%20effect%20on%20bleeding%20frequency,%20clotting%20factor%20concentrate%20usage,%20and%20haemostatic%20and%20fibrinolytic%20parameters.pdf (accessed 2 Dec 2015).
- ↑ Douma-van Riet DMC, Engelbert RHH, Van Genderen FR, Horst-De Ronde MTM, Goede-Bolders A, Hartman A. Physical fitness in children with haemophilia and the effect of overweight. Haemophilia 2009;15:519-527. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2008.01928.x/epdf (accessed 22 Jan 2016).
- ↑ Broderick CR, Herbert RD, Latimer J, Curtin JA, Selvadurai HC. The Effect Of An Exercise Intervention On Aerobic Fitness, Strength and Quality of life in children with Haemophilia. BMC Blood Disorders 2006;6:2. http://www.biomedcentral.com/content/pdf/1471-2326-6-2.pdf (accessed 9 Oct 2015).
- ↑ Querol F, Perez-alendaa S, Gallachc JE, Devis-devis J, Valencia-peris A, Gonzalez Moreno LM. Haemophilia: exercise and sport. Apunts Med Esport 2010;46(165:29-39. http://www.elsevier.es/…/277/277v46n169a90001817pdf001_2.pdf (accessed 15 Oct 2015)
- ↑ Buzzard B, Beeton K. Physiotherapy Management of Haemophilia. Oxford: Wiley, 2008.
- ↑ Durstine JL, Gordon B, Wang Z, Luo X. Chronic disease and the link to physical activity. Journal of Sport and Health Science 2013;2(1)3-11. http://www.sciencedirect.com/science/article/pii/S2095254612000701 (accessed 13 Dec 2015).
- ↑ Hofstede FG, Fijnvandraat K, Plug I, Kamphuisen PW, Rosendaal FR, Peters M. Obesity: a new disaster for haemophiliac patients? A nationwide survey. Haemophilia 2008;14:1035-1038. http://onlinelibrary.wiley.com/…/j.1365-2516.2008.01806.x.p… (accessed 30 Sept 2015).
- ↑ Buxbaum NP, Ponce P, Saidi P, Michaels LA. Psychosocial correlates of physical activity in adolescents with haemophilia. Haemophilia. 2010;16:656-61. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2010.02217.x/epdf. (accessed 21 Jan 2016).
- ↑ Hofstede FG, Fijnvandraat K, Plug I, Kamphuisen PW, Rosendaal FR, Peters M. Obesity: a new disaster for haemophiliac patients? A nationwide survey. Haemophilia 2008;14:1035-1038. http://onlinelibrary.wiley.com/…/j.1365-2516.2008.01806.x.p… (accessed 30 Sept 2015).
- ↑ Douma-van Riet DMC, Engelbert RHH, Van Genderen FR, Horst-De Ronde MTM, Goede-Bolders A, Hartman A. Physical fitness in children with haemophilia and the effect of overweight. Haemophilia 2009;15:519-527. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2008.01928.x/epdf (accessed 22 Jan 2016).
- ↑ Licence K. Promoting and protecting the health of children and young people. Child: care, health and development 2004;30(6):623-635. http://onlinelibrary.wiley.com/enhanced/doi/10.1111/j.1365-2214.2004.00473.x (accessed 22 Jan 2016).
- ↑ Beardsley DS. Sport and Exercise for children with chronic health conditions. Champaign IL:Human Kinetics 1995:302-9.
- ↑ Buzzard BM. Sports and haemophilia: antagonist or protagonist. Clinical Orthopaedics and Related Research 1996;328:25-30. http://www.ncbi.nlm.nih.gov/pubmed/8653965 (accessed 19 Jan 2016).
- ↑ Johnson MJ, Gorlin JB. Child Development with a Bleeding Disorder and Transition. New York: National Hemophilia Foundation 2013:1-16. https://www.hemophilia.org/…/Nurses-Guide-Chapter-13a-Child… (accessed 10 Oct 2015).
- ↑ Barnes C, Wong P, Egan B, Speller T, Cameron F, Jones G, Ekert H, Monagle P. Reduced Bone Density Among Children With Severe Hemophilia. Pediatrics 2004;114:2:e177-e181. http://www.ncbi.nlm.nih.gov/pubmed/15286254 (accessed 9 Oct 2015).
- ↑ Tlacuilo-parra A, Morales-zambrano R, Tostadorabago N, Esparza-Flores MA, Lopez-Guido B, Orozcalcala J. Inactivity is a risk factor for low bone mineral density among haemophilic children. British Journal of Haematology 2008;140:562-567 http://onlinelibrary.wiley.com/…/j.1365-2141.2007.06972.x.p… (accessed 8 Nov 2015).
- ↑ ICF. International Classification of Functioning, Disability and Health (ICF). http://www.who.int/classifications/icf/en/ (accessed 5 Jan 2016).
- ↑ Cassis FRMY. Treatment of Haemophilia. Psychosocial Care for people with Haemophilia 2007;1-12. https://haemophilia.ie/PDF/Psychosocial-Care.pdf (accessed 10 Jan 2016).
- ↑ Cassis FRMY. Treatment of Haemophilia. Psychosocial Care for people with Haemophilia 2007;1-12. https://haemophilia.ie/PDF/Psychosocial-Care.pdf (accessed 10 Jan 2016).
- ↑ Cassis FRMY. Treatment of Haemophilia. Psychosocial Care for people with Haemophilia 2007;1-12. https://haemophilia.ie/PDF/Psychosocial-Care.pdf (accessed 12 Jan 2016).
- ↑ Anderson A, Forsyth A. Playing it safe: Bleeding Disorders, Sport and Exercise New York: National Haemophilia Foundation. 1- 44. https://www.hemophilia.org/…/docume…/files/PlayingItSafe.pdf (accessed 6 Oct 2015).
- ↑ Cassis FR, Querol F, Forsyth A, Iorio A. Psychosocial aspects of haemophilia: a systematic review of methodologies and findings. Haemophilia 2012; 18:3:101-14. http://www.ncbi.nlm.nih.gov/pubmed/22059839. (accessed 22 Jan 2016).
- ↑ Sherlock E, O’Donnell JS, White B, Blake C. Physical activity levels and participation in sports in Irish people with haemophilia. Haemophilia 2010;16:202-9. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2009.02111.x/epdf. (accessed 21 Jan 2016).
- ↑ Buxbaum NP, Ponce P, Saidi P, Michaels LA. Psychocial correlates of physical activity in adolescents with haemophilia. Haemophilia 2010;16:656-61. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2010.02217.x/epdf. (accessed 21 Jan 2016).
- ↑ Cassis FR, Querol F, Forsyth A, Iorio A. Psychosocial aspects of haemophilia: a systematic review of methodologies and findings. Haemophilia 2012; 18:3:101-14. http://www.ncbi.nlm.nih.gov/pubmed/22059839. (accessed 22 Jan 2016).
- ↑ Buxbaum NP, Ponce P, Saidi P, Michaels LA. Psychocial correlates of physical activity in adolescents with haemophilia. Haemophilia 2010;16:656-61. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2516.2010.02217.x/epdf. (accessed 21 Jan 2016).