Management of Ankle Osteochondral Lesions: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Definitions == | == Definitions == | ||
Cartilage is a connective tissue characterised by three components:<ref name=":3">Armiento AR, Alini M, Stoddart MJ. [https://www.sciencedirect.com/science/article/pii/S0169409X18303193?via%3Dihub Articular fibrocartilage - Why does hyaline cartilage fail to repair?] Adv Drug Deliv Rev. 2019 Jun;146:289-305.</ref> | |||
* Polysaccharides ( a cellular component composed of ground substance) | |||
* Fibrous proteins | |||
* Interstitial fluid with water as the main component | |||
* [[Cartilage|Hyaline cartilage]]: is a connective tissue located at the ends of bones. Its primary cells are chondrocytes. Their role is to maintain the cartilage extracellular matrix (ECM), which is responsible for biological and mechanical function of the cartilage. Hyaline cartilage ECM contains:<ref>Lakin BA, Snyder BD, Grinstaff MW. [https://www.annualreviews.org/doi/full/10.1146/annurev-bioeng-071516-044525 Assessing cartilage biomechanical properties: techniques for evaluating the functional performance of cartilage in health and disease. Annual review of biomedical engineering]. 2017 Jun 21;19:27-55.</ref> | Cartilage gets its nutrition via diffusion from surrounding tissues as it has no direct blood supply, lymphatics and nerves.<ref name=":3" /> Each of the three cartilaginous tissues has different composition and function, including hyaline, fibrocartilage and elastic cartilage. | ||
*[[Cartilage|Hyaline cartilage]]: is a connective tissue located at the ends of bones. Its primary cells are chondrocytes. Their role is to maintain the cartilage extracellular matrix (ECM), which is responsible for the biological and mechanical function of the cartilage. Hyaline cartilage ECM contains:<ref>Lakin BA, Snyder BD, Grinstaff MW. [https://www.annualreviews.org/doi/full/10.1146/annurev-bioeng-071516-044525 Assessing cartilage biomechanical properties: techniques for evaluating the functional performance of cartilage in health and disease. Annual review of biomedical engineering]. 2017 Jun 21;19:27-55.</ref> | |||
** Collagen type II (10-20%) | ** Collagen type II (10-20%) | ||
** Proteoglycan (1-10%) | ** Proteoglycan (1-10%) | ||
** Water (65-85%) | ** Water (65-85%) | ||
* [[Cartilage|Fibrocartilage]] is a "transitional tissue between hyaline cartilage and dense regular connective tissue such as tendons and ligaments."<ref name=":3" /> It contains: | *[[Cartilage|Fibrocartilage]] is a "transitional tissue between hyaline cartilage and dense regular connective tissue such as tendons and ligaments."<ref name=":3" /> It contains: | ||
** High levels of type I collagen | ** High levels of type I collagen | ||
** Type II collagen | ** Type II collagen | ||
** Small component of ground substance <ref name=":3" /> | ** Small component of ground substance <ref name=":3" /> | ||
* [[Cartilage|Elastic cartilage]]: is | *[[Cartilage|Elastic cartilage]]: is flexible connective tissue cartilage that can withstand repeated bending.<ref name=":3" /> The components of the cartilage are:<ref name=":3" /> | ||
** Type II collagen | ** Type II collagen | ||
** Elastic fibres | ** Elastic fibres | ||
** Large chondrocytes | ** Large chondrocytes | ||
[[Bone|Subchondral bone]] is located below the hyaline cartilage and cement line and is responsible for providing mechanical and nutritional support for cartilage. Its mechanical properties include shock absorption. <ref>Hu Y, Chen X, Wang S, Jing Y, Su J. [https://www.nature.com/articles/s41413-021-00147-z.pdf Subchondral bone microenvironment in osteoarthritis and pain]. Bone research. 2021 Mar 17;9(1):1-3.</ref> | [[Bone|Subchondral bone]] is located below the hyaline cartilage and cement line and is responsible for providing mechanical and nutritional support for cartilage. Its mechanical properties include shock absorption. <ref>Hu Y, Chen X, Wang S, Jing Y, Su J. [https://www.nature.com/articles/s41413-021-00147-z.pdf Subchondral bone microenvironment in osteoarthritis and pain]. Bone research. 2021 Mar 17;9(1):1-3.</ref> In addition, the subchondral bone contains vessels that directly interact with the hyaline cartilage layer. The perfusion mechanism of the subchondral bone vessels is responsible for distributing 50% of cartilage nutrients..<ref>Imhof H, Sulzbacher I, Grampp S, Czerny C, Youssefzadeh S, Kainberger F. Subchondral bone and cartilage disease: a rediscovered functional unit. Investigative radiology. 2000 Oct 1;35(10):581-8.</ref> | ||
'''Osteochondral lesions (OCL)''' are defects affecting the structure of the cartilaginous surface and underlying subchondral bone. When lesion's healing phase begins and tissue | '''Osteochondral lesions (OCL)''' are defects affecting the structure of the cartilaginous surface and underlying subchondral bone. When the lesion's healing phase begins and tissue forms, the fibrocartilage is often the new tissue, which has mechanical disadvantages to the hyaline. In some cases, hyaline cartilage forms during the repair process, but the mechanism of hyaline vs fibrocartilage formation is unknown.<ref name=":3" /> | ||
== Healing of OCL == | == Healing of OCL == | ||
Osteochondral lesions have poor healing capacity. <ref name=":4">Lydon H, Getgood A, Henson FMD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6376560/ Healing of Osteochondral Defects via Endochondral Ossification in an Ovine Model]. Cartilage. 2019 Jan;10(1):94-101.</ref> The study completed in animals<ref>Shapiro F, Koide S, Glimcher MJ. Cell origin and differentiation in the repair of full-thickness defects of articular cartilage. J Bone Joint Surg Am. 1993 Apr;75(4):532-53. </ref> demonstrates the following stages of healing in the OCL:<ref name=":4" /> | Osteochondral lesions have poor healing capacity. <ref name=":4">Lydon H, Getgood A, Henson FMD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6376560/ Healing of Osteochondral Defects via Endochondral Ossification in an Ovine Model]. Cartilage. 2019 Jan;10(1):94-101.</ref> The study completed in animals<ref>Shapiro F, Koide S, Glimcher MJ. Cell origin and differentiation in the repair of full-thickness defects of articular cartilage. J Bone Joint Surg Am. 1993 Apr;75(4):532-53. </ref> demonstrates the following stages of healing in the OCL:<ref name=":4" /> | ||
Week 1-2: Initial fibrin repair, damaged site begins to fill with blood clot and fibrous tissue, mesenchymal cell recruitment | Week 1-2: Initial fibrin repair, the damaged site begins to fill with a blood clot and fibrous tissue, mesenchymal cell recruitment initiates | ||
Week 4-8: Cartilage formation starts adjacent to the damaged cartilage | Week 4-8: Cartilage formation starts adjacent to the damaged cartilage | ||
| Line 46: | Line 51: | ||
* avascular necrosis<ref name=":0" /> | * avascular necrosis<ref name=":0" /> | ||
* metabolic factors<ref name=":5" /> | * metabolic factors<ref name=":5" /> | ||
There are three types of trauma leading to development of OCL: compaction, shearing or avulsion. | There are three types of trauma leading to the development of OCL: compaction, shearing or avulsion. | ||
== Osteochondral Lesion of the Ankle == | == Osteochondral Lesion of the Ankle == | ||
According to Ferkel et al,<ref>Ferkel RD, Chams RN. Chronic lateral instability: arthroscopic findings and long-term results. Foot Ankle Int. 2007 Jan;28(1):24-31.</ref> a high percentage of patients with lateral ankle instability developed intra-articular pathology. In the ankle joint, the osteochondral lesion | According to Ferkel et al.,<ref>Ferkel RD, Chams RN. Chronic lateral instability: arthroscopic findings and long-term results. Foot Ankle Int. 2007 Jan;28(1):24-31.</ref> a high percentage of patients with lateral ankle instability developed intra-articular pathology. In the ankle joint, the osteochondral lesion is present in the talar. The osteochondral lesion of the talar cartilage (OCT) and subchondral bone can cause a partial or complete detachment of the fragment. There are six categories of the lesion: | ||
* chondral (cartilage only) | * chondral (cartilage only) | ||
| Line 56: | Line 61: | ||
* cystic | * cystic | ||
In addition to the above categories | In addition to the above lesion categories, OCT can be stable or unstable, non-displaced or displaced. | ||
=== Classification System for OCT === | === Classification System for OCT === | ||
* Berndt and Harty<ref>BERNDT AL, HARTY M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959 Sep;41-A:988-1020.</ref> classification system for radiographic staging of osteochondral lesions of the talus. It applies to traumatic and non-traumatic aetiology of the lesion:<ref name=":1">Badekas T, Takvorian M, Souras N. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3764304/ Treatment principles for osteochondral lesions in foot and ankle]. Int Orthop. 2013 Sep;37(9):1697-706. </ref> | * Berndt and Harty<ref>BERNDT AL, HARTY M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959 Sep;41-A:988-1020.</ref> classification system for radiographic staging of osteochondral lesions of the talus. It applies to traumatic and non-traumatic aetiology of the lesion:<ref name=":1">Badekas T, Takvorian M, Souras N. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3764304/ Treatment principles for osteochondral lesions in foot and ankle]. Int Orthop. 2013 Sep;37(9):1697-706. </ref> | ||
** Stage I: with the foot in inverted position, the lateral border is compressed against the face of the fibula, | ** Stage I: with the foot in an inverted position, the lateral border is compressed against the face of the fibula, and the collateral ligament remains intact. | ||
** Stage II: with progressive foot inversion, lateral ligament is ruptured and the avulsion of the chip begins | ** Stage II: with progressive foot inversion, the lateral ligament is ruptured, and the avulsion of the chip begins | ||
** Stage III: the chip is fully detached but remains in place | ** Stage III: the chip is fully detached but remains in place | ||
** Stage IV: detached | ** Stage IV: displacement of a detached fragment following inversion | ||
* Loomer et al<ref>Loomer R, Fisher C, Lloyd-Smith R, Sisler J, Cooney T. Osteochondral lesions of the talus. Am J Sports Med. 1993 Jan-Feb;21(1):13-9. </ref | * Loomer et al.<ref>Loomer R, Fisher C, Lloyd-Smith R, Sisler J, Cooney T. Osteochondral lesions of the talus. Am J Sports Med. 1993 Jan-Feb;21(1):13-9. </ref> added a Stage V to Berndt and Harty classification system:<ref name=":1" /> | ||
** Stage I -IV as<nowiki/> above | ** Stage I -IV as<nowiki/> above | ||
** Stage V: | ** Stage V: the p<nowiki/>resence of a subchondral cyst. | ||
* Ferkel and Sgaglione <ref>Ferkel RD, Sgaglione NA, DelPizzo W. Arthroscopic treatment of osteochondral lesions of the talus: long-term results. Orthop Trans. 1990;14:172–173.</ref> developed a classification system based on computed tomography (CT) | * Ferkel and Sgaglione <ref>Ferkel RD, Sgaglione NA, DelPizzo W. Arthroscopic treatment of osteochondral lesions of the talus: long-term results. Orthop Trans. 1990;14:172–173.</ref> developed a classification system based on computed tomography (CT): | ||
** Stage I: Cystic lesion with dome of talus (intact roof) | ** Stage I: Cystic lesion with the dome of the talus (intact roof) | ||
** Stage IIa:Cystic lesion with communication to talar dome surface | ** Stage IIa: Cystic lesion with communication to the talar dome surface | ||
** Stage IIb: Open articular surface lesion with overlying undisplaced fragment | ** Stage IIb: Open articular surface lesion with overlying undisplaced fragment | ||
** Stage III: Undisplaced lesion with lucency | ** Stage III: Undisplaced lesion with lucency | ||
** Stage IV: Displaced fragment<ref name=":2">Elghawy AA, Sesin C, Rosselli M. [https://bmjopensem.bmj.com/content/4/1/e000318 Osteochondral defects of the talus with a focus on platelet-rich plasma as a potential treatment option: a review.] BMJ Open Sport Exerc Med. 2018 Feb 1;4(1):e000318. </ref> | ** Stage IV: Displaced fragment<ref name=":2">Elghawy AA, Sesin C, Rosselli M. [https://bmjopensem.bmj.com/content/4/1/e000318 Osteochondral defects of the talus with a focus on platelet-rich plasma as a potential treatment option: a review.] BMJ Open Sport Exerc Med. 2018 Feb 1;4(1):e000318. </ref> | ||
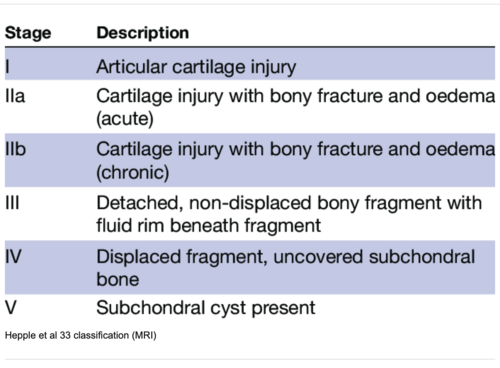
* Hepple et al<ref>Hepple S, Winson IG, Glew D. Osteochondral lesions of the talus: a revised classification. Foot Ankle Int. 1999 Dec;20(12):789-93.</ref> developed a classification system based on magnetic resonance imaging (MRI). <ref name=":2" /> | * Hepple et al.<ref>Hepple S, Winson IG, Glew D. Osteochondral lesions of the talus: a revised classification. Foot Ankle Int. 1999 Dec;20(12):789-93.</ref> developed a classification system based on magnetic resonance imaging (MRI). <ref name=":2" /> | ||
[[File:OCL MRI classification.png|center|thumb|500x500px|<small>MRI classification of OCL. Adapted from AA, Sesin C, Rosselli M. Osteochondral defects of the talus with a focus on platelet-rich plasma as a potential treatment option: a review. BMJ Open Sport Exerc Med. 2018 Feb 1;4(1):e000318.</small> ]] | [[File:OCL MRI classification.png|center|thumb|500x500px|<small>MRI classification of OCL. Adapted from AA, Sesin C, Rosselli M. Osteochondral defects of the talus with a focus on platelet-rich plasma as a potential treatment option: a review. BMJ Open Sport Exerc Med. 2018 Feb 1;4(1):e000318.</small> ]] | ||
== Clinical Presentation == | == Clinical Presentation == | ||
Patients with OCL will report deep ankle pain associated with weight-bearing, limitations in range of motion, impaired function, stiffness, and feeling of catching and locking. In addition, the patient may experience tenderness and swelling around the medial and lateral ankle. <ref name=":5" />Examination often reveals subtalar and talonavicular joints range of motion restrictions, impaired ligamentous ankle stability and hindfoot malalignment. <ref name=":1" /> <ref name=":5" /> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
* AP and lateral X-ray completed in weight-bearing position<ref name=":5" /> | * AP and lateral X-ray completed in a weight-bearing position. <ref name=":5" /> | ||
* MRI captures the integrity of soft tissue and subchondral cancellous bone<ref>Sophia Fox AJ, Bedi A, Rodeo SA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445147/ The basic science of articular cartilage: structure, composition, and function. Sports Health]. 2009 Nov;1(6):461-8. </ref> | * MRI captures the integrity of soft tissue and subchondral cancellous bone. <ref>Sophia Fox AJ, Bedi A, Rodeo SA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445147/ The basic science of articular cartilage: structure, composition, and function. Sports Health]. 2009 Nov;1(6):461-8. </ref> | ||
* CT allows a better resolution of bony pathologies | * CT allows a better resolution of bony pathologies but offers less information on articular cartilage wear and soft tissues.<ref name=":5" /> | ||
* SPECT CT enables information received from both MRI and CT . | * SPECT CT enables information received from both MRI and CT. Caution: the amount of radiation the patient is exposed to by having this procedure.<ref name=":5" /> | ||
* Ankle arthroscopy allows for | * Ankle arthroscopy allows for direct visualisation of the entire joint. <ref name=":5" /> | ||
== Outcome Measures == | == Outcome Measures == | ||
| Line 100: | Line 105: | ||
=== General principles in rehabilitation management === | === General principles in rehabilitation management === | ||
There is a lack of high quality evidence for a specific treatment protocol | There is a lack of high-quality evidence for a specific treatment protocol for managing the ankle osteochondral lesion. <ref name=":6">Simpson H. Osteochondral Lesions Course. Physioplus 2022</ref> Therefore, when establishing goals, planning the treatment and choosing the interventions, the clinician must consider the biological phases of healing. In general, rehabilitation program should: | ||
* Be comprehensive and include multi-modal functional training | * Be comprehensive and include multi-modal functional training | ||
* Include minimum of six weeks of supervised rehabilitation training | * Include a minimum of six weeks of supervised rehabilitation training | ||
* Address postural control, balance and proprioception retraining | * Address postural control, balance and proprioception retraining | ||
* Incorporate entire kinetic chain to improve overall strength | * Incorporate the entire kinetic chain to improve overall strength | ||
* Include activities to maintain range of movement | * Include activities to maintain a range of movement | ||
* Include measures to protect the ankle joint by making the patient wear a lace-up brace | * Include measures to protect the ankle joint by making the patient wear a lace-up brace | ||
* Continue to monitor the patient for unexplained increase in pain up to 2 years | * Continue to monitor the patient for an unexplained increase in pain for up to 2 years | ||
=== Special Concerns === | === Special Concerns === | ||
In the management of | In the management of osteochondral lesions, the following rehabilitation considerations must apply:<ref name=":6" /> | ||
# '''Avoid shear forces''' | # '''Avoid shear forces''' | ||
| Line 116: | Line 121: | ||
# '''Adequate pacing of the activities due to slow recovery''' | # '''Adequate pacing of the activities due to slow recovery''' | ||
# '''Monitor pain''' | # '''Monitor pain''' | ||
# '''Prevent development of the compensatory movements''' | # '''Prevent the development of the compensatory movements''' | ||
==== Shear forces ==== | ==== Shear forces ==== | ||
Shear forces are often the underlying cause | Shear forces are often the underlying cause of OCL in chronic ankle instability. <blockquote>Avoid shear forces for over three months. <ref name=":6" /> </blockquote> | ||
==== Compressive forces ==== | ==== Compressive forces ==== | ||
Fibrocartilage is not as strong as hyaline cartilage.<blockquote> | Fibrocartilage is not as strong as hyaline cartilage.<blockquote>Delay full weight bearing for as long as six weeks, based on specific clinical factors.<ref name=":6" /></blockquote> | ||
==== Slow Recovery ==== | ==== Slow Recovery ==== | ||
Repair of cartilage takes time.<blockquote>Take it easy with | Repair of cartilage takes time.<blockquote>Take it easy with steps 1 and 2 and maintain partial weight bearing.<ref name=":6" /></blockquote> | ||
==== Monitor pain ==== | ==== Monitor pain ==== | ||
<blockquote> | <blockquote>Individualise treatment and respect patient's pain. <ref name=":6" /></blockquote> | ||
==== Compensatory movements ==== | ==== Compensatory movements ==== | ||
<blockquote> | <blockquote>Correct faulty motor patterns. <ref name=":6" /></blockquote> | ||
=== Ankle Osteochondral Lesions Treatment Strategies<ref name=":6" /> === | === Ankle Osteochondral Lesions Treatment Strategies<ref name=":6" /> === | ||
| Line 138: | Line 143: | ||
* Take it EASY | * Take it EASY | ||
* Move the | * Move the talocrural joints, but DO NOT compress or shear | ||
* Incorporate cardiovascular fitness | * Incorporate cardiovascular fitness | ||
* Maintain partial weight bearing | * Maintain partial weight bearing | ||
| Line 146: | Line 151: | ||
==== Stage 2 ==== | ==== Stage 2 ==== | ||
* This | * This phase focuses on function | ||
* It is considered a pre-participation phase | * It is considered a pre-participation phase | ||
* Focus on details | * Focus on details | ||
| Line 163: | Line 168: | ||
* ''Have pain-free full range of loaded dorsiflexion'' | * ''Have pain-free full range of loaded dorsiflexion'' | ||
* ''Perform a single hop test without pain and in good alignment'' | * ''Perform a single hop test without pain and in good alignment'' | ||
* ''Demonstate | * ''Demonstate reasonable motor control in posterior medial movement'' | ||
</blockquote> | </blockquote> | ||
Revision as of 18:50, 4 August 2022
Definitions[edit | edit source]
Cartilage is a connective tissue characterised by three components:[1]
- Polysaccharides ( a cellular component composed of ground substance)
- Fibrous proteins
- Interstitial fluid with water as the main component
Cartilage gets its nutrition via diffusion from surrounding tissues as it has no direct blood supply, lymphatics and nerves.[1] Each of the three cartilaginous tissues has different composition and function, including hyaline, fibrocartilage and elastic cartilage.
- Hyaline cartilage: is a connective tissue located at the ends of bones. Its primary cells are chondrocytes. Their role is to maintain the cartilage extracellular matrix (ECM), which is responsible for the biological and mechanical function of the cartilage. Hyaline cartilage ECM contains:[2]
- Collagen type II (10-20%)
- Proteoglycan (1-10%)
- Water (65-85%)
- Fibrocartilage is a "transitional tissue between hyaline cartilage and dense regular connective tissue such as tendons and ligaments."[1] It contains:
- High levels of type I collagen
- Type II collagen
- Small component of ground substance [1]
- Elastic cartilage: is flexible connective tissue cartilage that can withstand repeated bending.[1] The components of the cartilage are:[1]
- Type II collagen
- Elastic fibres
- Large chondrocytes
Subchondral bone is located below the hyaline cartilage and cement line and is responsible for providing mechanical and nutritional support for cartilage. Its mechanical properties include shock absorption. [3] In addition, the subchondral bone contains vessels that directly interact with the hyaline cartilage layer. The perfusion mechanism of the subchondral bone vessels is responsible for distributing 50% of cartilage nutrients..[4]
Osteochondral lesions (OCL) are defects affecting the structure of the cartilaginous surface and underlying subchondral bone. When the lesion's healing phase begins and tissue forms, the fibrocartilage is often the new tissue, which has mechanical disadvantages to the hyaline. In some cases, hyaline cartilage forms during the repair process, but the mechanism of hyaline vs fibrocartilage formation is unknown.[1]
Healing of OCL[edit | edit source]
Osteochondral lesions have poor healing capacity. [5] The study completed in animals[6] demonstrates the following stages of healing in the OCL:[5]
Week 1-2: Initial fibrin repair, the damaged site begins to fill with a blood clot and fibrous tissue, mesenchymal cell recruitment initiates
Week 4-8: Cartilage formation starts adjacent to the damaged cartilage
Weeks 8 -12: Bone formation begins through endochondral ossification
Week 18: New bone formation continues
Week 26: Completion of the healing process
OCL Aetiology[edit | edit source]
The aetiology of the osteochondral lesion can be:
- traumatic (80% of cases)[7]
- joint malalignments[8]
- ligament laxity (38% of patients)[7]
- instability (39% of patients)[7]
- genetic predisposition[8]
- endocrine factors[7][8]
- avascular necrosis[8]
- metabolic factors[7]
There are three types of trauma leading to the development of OCL: compaction, shearing or avulsion.
Osteochondral Lesion of the Ankle[edit | edit source]
According to Ferkel et al.,[9] a high percentage of patients with lateral ankle instability developed intra-articular pathology. In the ankle joint, the osteochondral lesion is present in the talar. The osteochondral lesion of the talar cartilage (OCT) and subchondral bone can cause a partial or complete detachment of the fragment. There are six categories of the lesion:
- chondral (cartilage only)
- chondral-subchondral (cartilage and bone)
- subchondral (intact overlying cartilage)
- cystic
In addition to the above lesion categories, OCT can be stable or unstable, non-displaced or displaced.
Classification System for OCT[edit | edit source]
- Berndt and Harty[10] classification system for radiographic staging of osteochondral lesions of the talus. It applies to traumatic and non-traumatic aetiology of the lesion:[11]
- Stage I: with the foot in an inverted position, the lateral border is compressed against the face of the fibula, and the collateral ligament remains intact.
- Stage II: with progressive foot inversion, the lateral ligament is ruptured, and the avulsion of the chip begins
- Stage III: the chip is fully detached but remains in place
- Stage IV: displacement of a detached fragment following inversion
- Loomer et al.[12] added a Stage V to Berndt and Harty classification system:[11]
- Stage I -IV as above
- Stage V: the presence of a subchondral cyst.
- Ferkel and Sgaglione [13] developed a classification system based on computed tomography (CT):
- Stage I: Cystic lesion with the dome of the talus (intact roof)
- Stage IIa: Cystic lesion with communication to the talar dome surface
- Stage IIb: Open articular surface lesion with overlying undisplaced fragment
- Stage III: Undisplaced lesion with lucency
- Stage IV: Displaced fragment[14]
Clinical Presentation[edit | edit source]
Patients with OCL will report deep ankle pain associated with weight-bearing, limitations in range of motion, impaired function, stiffness, and feeling of catching and locking. In addition, the patient may experience tenderness and swelling around the medial and lateral ankle. [7]Examination often reveals subtalar and talonavicular joints range of motion restrictions, impaired ligamentous ankle stability and hindfoot malalignment. [11] [7]
Diagnostic Procedures[edit | edit source]
- AP and lateral X-ray completed in a weight-bearing position. [7]
- MRI captures the integrity of soft tissue and subchondral cancellous bone. [16]
- CT allows a better resolution of bony pathologies but offers less information on articular cartilage wear and soft tissues.[7]
- SPECT CT enables information received from both MRI and CT. Caution: the amount of radiation the patient is exposed to by having this procedure.[7]
- Ankle arthroscopy allows for direct visualisation of the entire joint. [7]
Outcome Measures[edit | edit source]
- Lower Extremity Functional Scale (LEFS)
- Foot and Ankle Ability Measure (FAAM)
- The Foot & Ankle Disability Index Score (FADI)
- Foot Function Index (FFI)
Comprehensive Rehabilitation[edit | edit source]
General principles in rehabilitation management[edit | edit source]
There is a lack of high-quality evidence for a specific treatment protocol for managing the ankle osteochondral lesion. [17] Therefore, when establishing goals, planning the treatment and choosing the interventions, the clinician must consider the biological phases of healing. In general, rehabilitation program should:
- Be comprehensive and include multi-modal functional training
- Include a minimum of six weeks of supervised rehabilitation training
- Address postural control, balance and proprioception retraining
- Incorporate the entire kinetic chain to improve overall strength
- Include activities to maintain a range of movement
- Include measures to protect the ankle joint by making the patient wear a lace-up brace
- Continue to monitor the patient for an unexplained increase in pain for up to 2 years
Special Concerns[edit | edit source]
In the management of osteochondral lesions, the following rehabilitation considerations must apply:[17]
- Avoid shear forces
- Avoid comprehensive forces
- Adequate pacing of the activities due to slow recovery
- Monitor pain
- Prevent the development of the compensatory movements
Shear forces[edit | edit source]
Shear forces are often the underlying cause of OCL in chronic ankle instability.
Avoid shear forces for over three months. [17]
Compressive forces[edit | edit source]
Fibrocartilage is not as strong as hyaline cartilage.
Delay full weight bearing for as long as six weeks, based on specific clinical factors.[17]
Slow Recovery[edit | edit source]
Repair of cartilage takes time.
Take it easy with steps 1 and 2 and maintain partial weight bearing.[17]
Monitor pain[edit | edit source]
Individualise treatment and respect patient's pain. [17]
Compensatory movements[edit | edit source]
Correct faulty motor patterns. [17]
Ankle Osteochondral Lesions Treatment Strategies[17][edit | edit source]
Stage 1[edit | edit source]
- Take it EASY
- Move the talocrural joints, but DO NOT compress or shear
- Incorporate cardiovascular fitness
- Maintain partial weight bearing
Examples of exercises:
Stage 2[edit | edit source]
- This phase focuses on function
- It is considered a pre-participation phase
- Focus on details
- Progress from partial to full weight bearing and standing on two feet
- Progress in load and complexity of the movement
Examples of exercises:
Stage 3[edit | edit source]
- Fitness activities
Examples of exercises:
Before proceeding to stage 4 patient must:
- Receive good scores on Star Excursion Balance Test(SEBT)
- Have pain-free full range of loaded dorsiflexion
- Perform a single hop test without pain and in good alignment
- Demonstate reasonable motor control in posterior medial movement
Stage 4[edit | edit source]
- Plyometrics
Resources[edit | edit source]
- Saccomanni B. Osteochondral Lesions of Talus: A Comprehensive Review. Mathews J Orthop. 2018; 3(1): 021.
- Hannon CP, Smyth NA, Murawski CD, Savage-Elliott I, Deyer TW, Calder JD, Kennedy JG. Osteochondral lesions of the talus: aspects of current management. Bone Joint J. 2014 Feb;96-B(2):164-71.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Armiento AR, Alini M, Stoddart MJ. Articular fibrocartilage - Why does hyaline cartilage fail to repair? Adv Drug Deliv Rev. 2019 Jun;146:289-305.
- ↑ Lakin BA, Snyder BD, Grinstaff MW. Assessing cartilage biomechanical properties: techniques for evaluating the functional performance of cartilage in health and disease. Annual review of biomedical engineering. 2017 Jun 21;19:27-55.
- ↑ Hu Y, Chen X, Wang S, Jing Y, Su J. Subchondral bone microenvironment in osteoarthritis and pain. Bone research. 2021 Mar 17;9(1):1-3.
- ↑ Imhof H, Sulzbacher I, Grampp S, Czerny C, Youssefzadeh S, Kainberger F. Subchondral bone and cartilage disease: a rediscovered functional unit. Investigative radiology. 2000 Oct 1;35(10):581-8.
- ↑ 5.0 5.1 Lydon H, Getgood A, Henson FMD. Healing of Osteochondral Defects via Endochondral Ossification in an Ovine Model. Cartilage. 2019 Jan;10(1):94-101.
- ↑ Shapiro F, Koide S, Glimcher MJ. Cell origin and differentiation in the repair of full-thickness defects of articular cartilage. J Bone Joint Surg Am. 1993 Apr;75(4):532-53.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 Krause F, Anwander H. Osteochondral lesion of the talus: still a problem?. EFORT open reviews. 2022 Jun 1;7(6):337-43.
- ↑ 8.0 8.1 8.2 8.3 Mosca M, Grassi A, Caravelli S. Osteochondral Lesions of Ankle and Knee. Will Future Treatments Really Be Represented by Custom-Made Metal Implants?. Journal of Clinical Medicine. 2022 Jul 1;11(13):3817.
- ↑ Ferkel RD, Chams RN. Chronic lateral instability: arthroscopic findings and long-term results. Foot Ankle Int. 2007 Jan;28(1):24-31.
- ↑ BERNDT AL, HARTY M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959 Sep;41-A:988-1020.
- ↑ 11.0 11.1 11.2 Badekas T, Takvorian M, Souras N. Treatment principles for osteochondral lesions in foot and ankle. Int Orthop. 2013 Sep;37(9):1697-706.
- ↑ Loomer R, Fisher C, Lloyd-Smith R, Sisler J, Cooney T. Osteochondral lesions of the talus. Am J Sports Med. 1993 Jan-Feb;21(1):13-9.
- ↑ Ferkel RD, Sgaglione NA, DelPizzo W. Arthroscopic treatment of osteochondral lesions of the talus: long-term results. Orthop Trans. 1990;14:172–173.
- ↑ 14.0 14.1 Elghawy AA, Sesin C, Rosselli M. Osteochondral defects of the talus with a focus on platelet-rich plasma as a potential treatment option: a review. BMJ Open Sport Exerc Med. 2018 Feb 1;4(1):e000318.
- ↑ Hepple S, Winson IG, Glew D. Osteochondral lesions of the talus: a revised classification. Foot Ankle Int. 1999 Dec;20(12):789-93.
- ↑ Sophia Fox AJ, Bedi A, Rodeo SA. The basic science of articular cartilage: structure, composition, and function. Sports Health. 2009 Nov;1(6):461-8.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 Simpson H. Osteochondral Lesions Course. Physioplus 2022