Management of Ankle Osteochondral Lesions: Difference between revisions
No edit summary |
m (Protected "Management of the Ankle Osteochondral Lesions" ([Edit=⧼protect-level-ppadmin⧽] (indefinite) [Move=⧼protect-level-ppadmin⧽] (indefinite))) |
(No difference)
| |
Revision as of 16:56, 1 August 2022
Definition[edit | edit source]
Osteochondral lesions (OCL) are defects affecting the structure of the cartilaginous surface and underlying subchondral bone. [1]The etiology of the lesion can be:[1]
- traumatic (most cases)
- joint malalignments
- instability
- genetic predisposition
- endocrine factors
- avascular necrosis
There are three types of trauma leading to development of OCL: compaction, shearing or avulsion.
Osteochondral Lesion of the Ankle[edit | edit source]
According to Ferkel et al[2] a high percentage of patients with lateral ankle instability developed intra-articular pathology. In the ankle joint, the osteochondral lesion can be found in the talar. The osteochondral lesion of the talar cartilage (OCT) and subchondral bone can cause a partial or complete detachment of the fragment. There are six categories of the lesion:
- chondral (cartilage only)
- chondral-subchondral (cartilage and bone)
- subchondral (intact overlying cartilage)
- cystic
In addition to the above categories of the lesion, OCT can be stable or unstable, non-displaced or displaced. Patient will report deep ankle pain associated with weightbearing, restricted range of motion, impaired function,stiffness, catching, locking and swelling. [3]
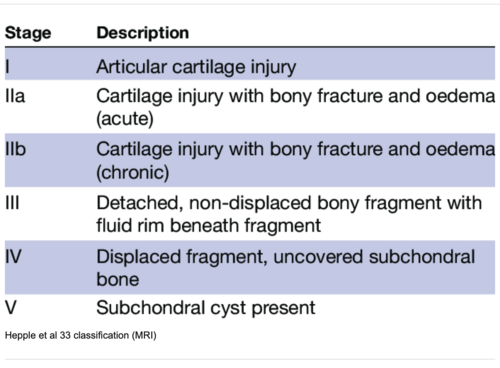
Classification System for OCT[edit | edit source]
- Berndt and Harty[4] classification system for radiographic staging of osteochondral lesions of the talus. It applies to traumatic and non-traumatic aetiology of the lesion:[3]
- Stage I: with the foot in inverted position, the lateral border is compressed against the face of the fibula, the collateral ligament remains intact.
- Stage II: with progressive foot inversion, lateral ligament is ruptured and the avulsion of the chip begins
- Stage III: the chip is fully detached but remains in place
- Stage IV: detached chip is displaced following inversion
- Loomer et al[5] added a stage V to Berndt and Harty classification system:[3]
- Stage I -IV as above
- Stage V: presence of a subchondral cyst.
- Ferkel and Sgaglione [6] developed a classification system based on computed tomography (CT)
- Stage I: Cystic lesion with dome of talus (intact roof)
- Stage IIa:Cystic lesion with communication to talar dome surface
- Stage IIb: Open articular surface lesion with overlying undisplaced fragment
- Stage III: Undisplaced lesion with lucency
- Stage IV: Displaced fragment[7]
Clinical Presentation[edit | edit source]
Patient with OCL will report deep ankle pain associated with weightbearing, restricted range of motion, impaired function,stiffness, catching, locking and swelling. [3]
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Intervention[edit | edit source]
General principles in rehabilitation management[edit | edit source]
- Lack of high quality evidence
- Follow biological phases of healing
Special Concerns[edit | edit source]
In the management of the osteochondral lesions the following rehabilitation considerations must apply:
- Avoid shear forces
- Avoid comprehensive forces
- Recovery is slow
- Monitor pain
- Watch for development of the compensatory movements
Shear forces[edit | edit source]
Shear forces are to be avoided over 3 months shear focus often underlying cause for OCL in Chronic Ankle Instability
Compressive forces[edit | edit source]
Fibre cartilage is not as strong as hyaline cartilage
Slow Recovery[edit | edit source]
Cartilage repair takes time
Monitor pain[edit | edit source]
Compensatory movements[edit | edit source]
Early motion is required for healing delay full weight bearing for 6 weeks or longer based on certain clinical factors, semi-rigid braces, or lace-up braces, crutches
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ 1.0 1.1 Mosca M, Grassi A, Caravelli S. Osteochondral Lesions of Ankle and Knee. Will Future Treatments Really Be Represented by Custom-Made Metal Implants?. Journal of Clinical Medicine. 2022 Jul 1;11(13):3817.
- ↑ Ferkel RD, Chams RN. Chronic lateral instability: arthroscopic findings and long-term results. Foot Ankle Int. 2007 Jan;28(1):24-31.
- ↑ 3.0 3.1 3.2 3.3 Badekas T, Takvorian M, Souras N. Treatment principles for osteochondral lesions in foot and ankle. Int Orthop. 2013 Sep;37(9):1697-706. doi: 10.1007/s00264-013-2076-1.
- ↑ BERNDT AL, HARTY M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959 Sep;41-A:988-1020.
- ↑ Loomer R, Fisher C, Lloyd-Smith R, Sisler J, Cooney T. Osteochondral lesions of the talus. Am J Sports Med. 1993 Jan-Feb;21(1):13-9.
- ↑ Ferkel RD, Sgaglione NA, DelPizzo W. Arthroscopic treatment of osteochondral lesions of the talus: long-term results. Orthop Trans. 1990;14:172–173.
- ↑ 7.0 7.1 Elghawy AA, Sesin C, Rosselli M. Osteochondral defects of the talus with a focus on platelet-rich plasma as a potential treatment option: a review. BMJ Open Sport Exerc Med. 2018 Feb 1;4(1):e000318.
- ↑ Hepple S, Winson IG, Glew D. Osteochondral lesions of the talus: a revised classification. Foot Ankle Int. 1999 Dec;20(12):789-93.