Osteoid Osteoma: Difference between revisions
No edit summary |
(added category Oncology) |
||
| (136 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class=" | <div class="editorbox"> | ||
'''Original Editors '''- [[User:Michelle Quill|Michelle Quill]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Definition/Description == | |||
A benign osteoblastic tumor consisting of vascular osteoid tissue centrally called the Nidus and sclerotic bone peripherally. Osteoid Osteoma does not grow or behave in a locally aggressive manner, and it has no potential for malignant transformation.<ref name="p9">Atesok KI, Alman BA, Schemitsch EH, Peyser A, Mankin H. Osteoid osteoma and osteoblastoma. The Journal of the American Academy of Orthopaedic Surgeons. https://www.ncbi.nlm.nih.gov/pubmed/22052644. Published November 2011.</ref> May initially appear on a radiograph as a small sclerotic bone island within a circular lucency.<ref name="p8" />It is classified as a stage I (latent) bone tumor.<ref name="p8" /> In >50% of cases, the lesion occurs in the metaphysis and diaphysis of the long bones, particularly the femur and tibia. Other anatomic sites of involvement include the spine, upper extremity, pelvis, sacrum, ribs, hands, and feet.<ref name="p1">Goodman, Snyder. Differential Diagnosis for Physical Therapists: 5th Edition. Screening for Referral. St. Louis, Missouri: Saunders Elsevier; 2013.</ref><ref name="p2">Goodman CG, Fuller KS. Pathology: Implications for the Physical Thearpist, 4th Edition. St. Louis, Missouri: Saunders Elsevier; 2014.</ref><ref name="p4">Atar D, Lehman WB, Grant AD. Tips of the trade. Computerized tomography--guided excision of osteoid osteoma. Orthop Rev. Dec 1992;21(12):1457-8.</ref> | |||
<br> | |||
{{#ev:youtube|mL4H3Qzz7Bc|300}}<ref>ctisus. Osteoid Osteoma Tibia on X ray. YouTube. https://www.youtube.com/watch?v=mL4H3Qzz7Bc#action=share. Published March 31, 2016. Accessed April 10, 2017.fckLR</ref> | |||
<br> | |||
== Prevalence == | |||
Osteoid osteomas account for 1/8 to 1/10 of symptomatic bone tumors and 5% of all primary bone tumors.<ref name="Lenke">Lenke LG, Sutherland CJ, Gilula LA.Osteoid osteoma of the proximal femur: CT-guided preoperative localization. Orthopedics. Mar 1994;17(3):289-92 fckLR</ref> Osteoid osteomas are the 2nd most common benign primary bone tumors resulting in 10-12% of all benign tumors.<ref name="p1" /> | |||
Osteoid osteomas occur in children and young adults between the ages of 7 and 25. All ages can be effected but 75-80% of patients are less than 25 years of age. The male to female ratio is 2-3:1 putting boys and young males at the greatest risk for developing osteoid osteomas.<ref name="p2" /><ref name="p0">Osteoid Osteoma: Symptoms, Causes & Treatment. UCSF Radiology. https://radiology.ucsf.edu/patient-care/services/osteoid-osteoma#accordion-imaging-of-osteoid-osteoma. Published February 23, 2016. Accessed April 10, 2017.</ref><ref name="p9" /><ref name="p3">Lenke LG, Sutherland CJ, Gilula LA. Osteoid osteoma of the proximal femur: CT-guided preoperative localization. Orthopedics. Mar 1994;17(3):289-92 fckLR</ref> <br> | |||
== Characteristics/Clinical Presentation == | |||
{{#ev:youtube|ZVNw6P_kfac}} | |||
<br> | |||
'''Presentation''' <br> <br> '''Early'''<br>• Local pain that is typically more frequent and severe at night <br>• Pain that is relieved by aspirin within 30 minutes (75% of cases)<br>• Pain that increases with activity and alcohol consumption<br>• Local swelling and point tenderness | |||
== | <ref name="p2" /><ref name="p3" /><ref name="p8">Leung, Albert HMS III. Osteoid Osteoma. http://eradiology.bidmc.harvard.edu/LearningLab/musculo/Leung.pdf</ref><br> <br>'''Late''' <br> • Bony deformity<br> • Gait disturbances<br>• Muscle atrophy<br> • Leg length discrepancy (longer leg on involved side)<br> • Scoliosis (concavity same side as lesion)<br> • Growth Disturbances<br> • OA | ||
<ref name="p9" /><br> '''Characteristics''' <br> • Most commonly found in diaphysis of long bones 70% of the time, the femur/tibia accounting for 55%, phalanges of hands and feet 20%, and the spine 10% (lamina and spinous processes)<ref name="p2" /><ref name="p3" /><ref name="p8" /><ref name="p9" /><br> • Around 1.5 cm in size<ref name="p2" /><ref name="p8" /><ref name="p9" /><ref name="p3" /><br>• Central Nidus, with circular lucency<ref name="p2" /><ref name="p8" /><ref name="p9" /><ref name="p3" /><br> • Osteoid Osteomas and osteoblastomas are histologically similar but differ in size, pain intensity, location, aggressiveness, and neural staining patterns<ref name="p8" /><br> • Osteoid Osteomas are classified by their relative position to the bone: cortical, cancellous, intraarticular, and subperiosteal<ref name="p8" /> | |||
'''<br>Classifications (based on location)<ref name="p8" />''' | |||
1.Cortical<br>•Most common location (80%)<br>•Radiolucent nidus seen within the bone cortex and surrounded by fusiform cortical thickening/laminated periosteal formation | |||
2.Cancellous<br>•Intramedullary lesion; mild reactive sclerosis & difficult to identify, significantly delaying the diagnosis<br>•Common sites: femoral neck, posterior spine, hands & feet | |||
3.Intraarticular<br>•Joint effusion or synovitis | |||
4.Subperiosteal<br>•Round mass adjacent to cortex<br>•Absent periosteal reaction<br>•Very rare<br><br> Due to the age of onset osteoid osteomas can easily be mis-diagnosed as a musculoskeletal disorder because when someone in their twenties reports pain, the vast majority of people assume the pain is musculoskeletal in nature.<ref name="p3" /> The true diagnosis is easily overlooked because epiphyseal lesions mimic intra-articular derangement and pain is typically localized to the site of the lesion, so the location of pain can be anywhere, and may coincide with common sites of musculoskeletal inflammation or strain.<ref name="p4" />Another reason diagnosis is easily misled is that pain usually occurs before the lesions are visible on radiographs and in the early stages can be easily missed on a radiograph.<ref name="p5">Pettine KA, Klassen RA. Osteoid-osteoma and osteoblastoma of the spine. J Bone Joint Surg Am. Mar 1986;68(3):354-61.</ref>Finally, these lesions may be associated with proliferative synovitis due to prostaglandin secretion that decreases range of motion, creates joint effusion, and can mimic inflammatory arthritis.<ref name="p6">Frassica FJ, Waltrip RL, Sponseller PD, et al. Clinicopathologic features and treatment of osteoid osteoma and osteoblastoma in children and adolescents. Orthop Clin North Am. Jul 1996;27(3):559-74.</ref><br> | |||
== Associated Comorbidities == | |||
No known causes | |||
== Medications == | == Medications == | ||
Pain caused by osteoid osteomas can be relieved with aspirin and NSAIDS, which inhibit the prostaglandins released by the tumor cells. Prostaglandins cause changes in vascular pressure, which stimulates sensory nerve endings locally, causing pain. Inhibition of these prostaglandins relieves pain.<ref name="p2" /><ref name="p3" /> <ref name="p9" />. Few studies have shown lasting affects of syptom relief after long term use of NSAIDS, some studies have shown without surigical management there is a probablity of evoltion into a osteoblastoma.<ref name="p9" /> | |||
== Diagnostic Tests/Lab Tests/Lab Values == | == Diagnostic Tests/Lab Tests/Lab Values == | ||
Osteoid osteomas can be detected on an MRI and CT scan, which are often used to identify the location of the nidus when the tumor is intra-articular. A CT scan will reveal the nidus as a small area of low attenuation surrounded by reactive bone formation, seen as a larger area of higher attenuation.<ref name="p1" /> <ref name="p2" /> | |||
Radiograph reveals a well demarcated area of translucency (nidus) inside the bone, often times with a central calcified dot. This is surrounded by bony sclerosis. Usually less than 1 cm in size<ref name="p7" /> | |||
An osteoid osteoma can also be detected with bone scan, or scintigraphy, which will show a focal uptake of the radiotracer by the tumor.<sup></sup>Scintigraphy is often used to detect an osteoid osteoma that is not easily seen on a radiograph, such as a vertebral tumor.<ref name="p2" /> | |||
Overall, CT scans are the best imaging tool for diagnosing osteoid osteomas.<ref name="p9" /> | |||
[[Image:Osteoid osteoma pics.jpg]] | |||
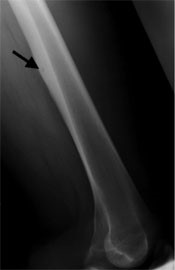
•This is an X-ray of an osteoid osteoma of the thigh(femur) with increased bone formation and subtle lucency(arrow).<ref name="p0" /> | |||
[[Image:Ctscan thigh.jpg]] | |||
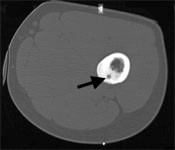
•This is a CT scan of an osteoid osteoma of the thigh(femur), a small, round lytic focus(arrow) surrounded by dense bone is demonstrated.<ref name="p0" /> | |||
[[Image:Mri.jpg]] | |||
• This is an MRI of an osteoid osteoma of the thigh(femur). There is increased bone formation(dark)surrounding a brighter spot. The bright spot represents the nidus(arrow)of the osteoid osteoma.<ref name="p0" /> | |||
== Causes == | == Causes == | ||
The actual cause of osteiod osteomas is unknown. The nidus has been found to contian abundant nerve fibers within its matrix, adjacent to areas rich in arterioles. Prostoglanden synthesis has been shown to occur in the nidus. These reports suggest an important pathophysiologic role for prostaglandins both as mediators of pain and vasodilation that may stimulate the nerve endings by increasing the blood flow within the tumor.<ref name="p9" /> An osteoid osteoma is a vascular lesion consisting of an area of immature bone surrounded by osteoblasts and osteoclasts. The tumor starts with the nidus, or nest of vascular osteoid tissue in the center of the tumor. The nidus then becomes surrounded by reactive bone sclerosis. After the removal of the nidus, the secondary bone sclerosis generally disappears gradually.<ref name="p7">Baggat M, Robbin M. emedicine.medscape.com/article/392850-media Case Eighty Four - Osteoid Osteoma retrieved from Musculoskeletal Imaging Teaching Files at http://www.uhrad.com/msiarc/msi084.htm</ref><br> | |||
== Systemic Involvement == | == Systemic Involvement == | ||
Systemic involvement is uncommon with an osteoid osteoma.<ref name="p2" /> | |||
Stomach ulcers, heartburn and bleeding problems can occur due to the prolonged use of NSAIDs in pain management. <ref name="p7" /> | |||
== Medical Management (current best evidence) == | == Medical Management (current best evidence) == | ||
'''NonSurgical''' <br>• NSAIDS | |||
<br>'''Surgical''' (three most common operations) <br>1.'''Open Excision'''- intraoperatively cut out tumor, difficult for surgeon, hard to see. Can result in longer hospital stay for patient with activity and weight bearing restrictions. Oldest method.<br>2. '''CT-guided Percutaneous Excision'''-CT image guidance to remove nidus with excision<br>3. '''CT-guided Radiofrequency Ablation'''-CT image guidance to remove nidus with heat using probe (quick recovery, most common procedure today) | |||
{{#ev:youtube| cb5WXtv5Xhk}} | |||
== Physical Therapy Management (current best evidence) == | == Physical Therapy Management (current best evidence) == | ||
None<br><br> | |||
== Case Reports == | == Case Reports == | ||
== Resources <br> == | [Http://www.uhrad.com/msiarc/msi084.htm www.uhrad.com/msiarc/msi084.htm Http://www.uhrad.com/msiarc/msi084.htm www.uhrad.com/msiarc/msi084.htm] | ||
<br> | |||
This is a link to a slide show containing three examples of different presentations of Osteoid Osteomas. | |||
[http://eradiology.bidmc.harvard.edu/LearningLab/musculo/Leung.pdf http://eradiology.bidmc.harvard.edu/LearningLab/musculo/Leung.pdf<br>][[]] | |||
== Resources == | |||
{{#ev:youtube|G4JJv1dhEa0}}<ref>P. osteoid osteoma. YouTube. https://www.youtube.com/watch?v=G4JJv1dhEa0. Published July 30, 2016. Accessed April 10, 2017.</ref> | |||
<br>Great review of the literature specific to osteoid osteoma of the foot and ankle. | |||
http://www.sciencedirect.com.libproxy.bellarmine.edu/science/article/pii/S1268773115000697?_rdoc=1&_fmt=high&_origin=gateway&_docanchor=&md5=b8429449ccfc9c30159a5f9aeaa92ffb&ccp=y<br> | |||
== References == | |||
<references /> | |||
<br> | |||
<br> | |||
[[Category:Oncology]] | |||
Latest revision as of 20:58, 30 June 2020
Original Editors - Michelle Quill from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Jacquelyn Moriah Facktor, Elaine Lonnemann, Admin, Chad Simmons, Michelle Quill, 127.0.0.1, WikiSysop, Rachael Lowe, Wendy Walker, Kim Jackson and Vidya Acharya
Definition/Description[edit | edit source]
A benign osteoblastic tumor consisting of vascular osteoid tissue centrally called the Nidus and sclerotic bone peripherally. Osteoid Osteoma does not grow or behave in a locally aggressive manner, and it has no potential for malignant transformation.[1] May initially appear on a radiograph as a small sclerotic bone island within a circular lucency.[2]It is classified as a stage I (latent) bone tumor.[2] In >50% of cases, the lesion occurs in the metaphysis and diaphysis of the long bones, particularly the femur and tibia. Other anatomic sites of involvement include the spine, upper extremity, pelvis, sacrum, ribs, hands, and feet.[3][4][5]
Prevalence[edit | edit source]
Osteoid osteomas account for 1/8 to 1/10 of symptomatic bone tumors and 5% of all primary bone tumors.[7] Osteoid osteomas are the 2nd most common benign primary bone tumors resulting in 10-12% of all benign tumors.[3]
Osteoid osteomas occur in children and young adults between the ages of 7 and 25. All ages can be effected but 75-80% of patients are less than 25 years of age. The male to female ratio is 2-3:1 putting boys and young males at the greatest risk for developing osteoid osteomas.[4][8][1][9]
Characteristics/Clinical Presentation[edit | edit source]
Presentation
Early
• Local pain that is typically more frequent and severe at night
• Pain that is relieved by aspirin within 30 minutes (75% of cases)
• Pain that increases with activity and alcohol consumption
• Local swelling and point tenderness
[4][9][2]
Late
• Bony deformity
• Gait disturbances
• Muscle atrophy
• Leg length discrepancy (longer leg on involved side)
• Scoliosis (concavity same side as lesion)
• Growth Disturbances
• OA
[1]
Characteristics
• Most commonly found in diaphysis of long bones 70% of the time, the femur/tibia accounting for 55%, phalanges of hands and feet 20%, and the spine 10% (lamina and spinous processes)[4][9][2][1]
• Around 1.5 cm in size[4][2][1][9]
• Central Nidus, with circular lucency[4][2][1][9]
• Osteoid Osteomas and osteoblastomas are histologically similar but differ in size, pain intensity, location, aggressiveness, and neural staining patterns[2]
• Osteoid Osteomas are classified by their relative position to the bone: cortical, cancellous, intraarticular, and subperiosteal[2]
Classifications (based on location)[2]
1.Cortical
•Most common location (80%)
•Radiolucent nidus seen within the bone cortex and surrounded by fusiform cortical thickening/laminated periosteal formation
2.Cancellous
•Intramedullary lesion; mild reactive sclerosis & difficult to identify, significantly delaying the diagnosis
•Common sites: femoral neck, posterior spine, hands & feet
3.Intraarticular
•Joint effusion or synovitis
4.Subperiosteal
•Round mass adjacent to cortex
•Absent periosteal reaction
•Very rare
Due to the age of onset osteoid osteomas can easily be mis-diagnosed as a musculoskeletal disorder because when someone in their twenties reports pain, the vast majority of people assume the pain is musculoskeletal in nature.[9] The true diagnosis is easily overlooked because epiphyseal lesions mimic intra-articular derangement and pain is typically localized to the site of the lesion, so the location of pain can be anywhere, and may coincide with common sites of musculoskeletal inflammation or strain.[5]Another reason diagnosis is easily misled is that pain usually occurs before the lesions are visible on radiographs and in the early stages can be easily missed on a radiograph.[10]Finally, these lesions may be associated with proliferative synovitis due to prostaglandin secretion that decreases range of motion, creates joint effusion, and can mimic inflammatory arthritis.[11]
Associated Comorbidities[edit | edit source]
No known causes
Medications[edit | edit source]
Pain caused by osteoid osteomas can be relieved with aspirin and NSAIDS, which inhibit the prostaglandins released by the tumor cells. Prostaglandins cause changes in vascular pressure, which stimulates sensory nerve endings locally, causing pain. Inhibition of these prostaglandins relieves pain.[4][9] [1]. Few studies have shown lasting affects of syptom relief after long term use of NSAIDS, some studies have shown without surigical management there is a probablity of evoltion into a osteoblastoma.[1]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Osteoid osteomas can be detected on an MRI and CT scan, which are often used to identify the location of the nidus when the tumor is intra-articular. A CT scan will reveal the nidus as a small area of low attenuation surrounded by reactive bone formation, seen as a larger area of higher attenuation.[3] [4]
Radiograph reveals a well demarcated area of translucency (nidus) inside the bone, often times with a central calcified dot. This is surrounded by bony sclerosis. Usually less than 1 cm in size[12]
An osteoid osteoma can also be detected with bone scan, or scintigraphy, which will show a focal uptake of the radiotracer by the tumor.Scintigraphy is often used to detect an osteoid osteoma that is not easily seen on a radiograph, such as a vertebral tumor.[4]
Overall, CT scans are the best imaging tool for diagnosing osteoid osteomas.[1]
•This is an X-ray of an osteoid osteoma of the thigh(femur) with increased bone formation and subtle lucency(arrow).[8]
•This is a CT scan of an osteoid osteoma of the thigh(femur), a small, round lytic focus(arrow) surrounded by dense bone is demonstrated.[8]
• This is an MRI of an osteoid osteoma of the thigh(femur). There is increased bone formation(dark)surrounding a brighter spot. The bright spot represents the nidus(arrow)of the osteoid osteoma.[8]
Causes[edit | edit source]
The actual cause of osteiod osteomas is unknown. The nidus has been found to contian abundant nerve fibers within its matrix, adjacent to areas rich in arterioles. Prostoglanden synthesis has been shown to occur in the nidus. These reports suggest an important pathophysiologic role for prostaglandins both as mediators of pain and vasodilation that may stimulate the nerve endings by increasing the blood flow within the tumor.[1] An osteoid osteoma is a vascular lesion consisting of an area of immature bone surrounded by osteoblasts and osteoclasts. The tumor starts with the nidus, or nest of vascular osteoid tissue in the center of the tumor. The nidus then becomes surrounded by reactive bone sclerosis. After the removal of the nidus, the secondary bone sclerosis generally disappears gradually.[12]
Systemic Involvement[edit | edit source]
Systemic involvement is uncommon with an osteoid osteoma.[4]
Stomach ulcers, heartburn and bleeding problems can occur due to the prolonged use of NSAIDs in pain management. [12]
Medical Management (current best evidence)[edit | edit source]
NonSurgical
• NSAIDS
Surgical (three most common operations)
1.Open Excision- intraoperatively cut out tumor, difficult for surgeon, hard to see. Can result in longer hospital stay for patient with activity and weight bearing restrictions. Oldest method.
2. CT-guided Percutaneous Excision-CT image guidance to remove nidus with excision
3. CT-guided Radiofrequency Ablation-CT image guidance to remove nidus with heat using probe (quick recovery, most common procedure today)
Physical Therapy Management (current best evidence)[edit | edit source]
None
Case Reports[edit | edit source]
This is a link to a slide show containing three examples of different presentations of Osteoid Osteomas.
http://eradiology.bidmc.harvard.edu/LearningLab/musculo/Leung.pdf
[[]]
Resources[edit | edit source]
Great review of the literature specific to osteoid osteoma of the foot and ankle.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Atesok KI, Alman BA, Schemitsch EH, Peyser A, Mankin H. Osteoid osteoma and osteoblastoma. The Journal of the American Academy of Orthopaedic Surgeons. https://www.ncbi.nlm.nih.gov/pubmed/22052644. Published November 2011.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Leung, Albert HMS III. Osteoid Osteoma. http://eradiology.bidmc.harvard.edu/LearningLab/musculo/Leung.pdf
- ↑ 3.0 3.1 3.2 Goodman, Snyder. Differential Diagnosis for Physical Therapists: 5th Edition. Screening for Referral. St. Louis, Missouri: Saunders Elsevier; 2013.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Goodman CG, Fuller KS. Pathology: Implications for the Physical Thearpist, 4th Edition. St. Louis, Missouri: Saunders Elsevier; 2014.
- ↑ 5.0 5.1 Atar D, Lehman WB, Grant AD. Tips of the trade. Computerized tomography--guided excision of osteoid osteoma. Orthop Rev. Dec 1992;21(12):1457-8.
- ↑ ctisus. Osteoid Osteoma Tibia on X ray. YouTube. https://www.youtube.com/watch?v=mL4H3Qzz7Bc#action=share. Published March 31, 2016. Accessed April 10, 2017.fckLR
- ↑ Lenke LG, Sutherland CJ, Gilula LA.Osteoid osteoma of the proximal femur: CT-guided preoperative localization. Orthopedics. Mar 1994;17(3):289-92 fckLR
- ↑ 8.0 8.1 8.2 8.3 Osteoid Osteoma: Symptoms, Causes & Treatment. UCSF Radiology. https://radiology.ucsf.edu/patient-care/services/osteoid-osteoma#accordion-imaging-of-osteoid-osteoma. Published February 23, 2016. Accessed April 10, 2017.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Lenke LG, Sutherland CJ, Gilula LA. Osteoid osteoma of the proximal femur: CT-guided preoperative localization. Orthopedics. Mar 1994;17(3):289-92 fckLR
- ↑ Pettine KA, Klassen RA. Osteoid-osteoma and osteoblastoma of the spine. J Bone Joint Surg Am. Mar 1986;68(3):354-61.
- ↑ Frassica FJ, Waltrip RL, Sponseller PD, et al. Clinicopathologic features and treatment of osteoid osteoma and osteoblastoma in children and adolescents. Orthop Clin North Am. Jul 1996;27(3):559-74.
- ↑ 12.0 12.1 12.2 Baggat M, Robbin M. emedicine.medscape.com/article/392850-media Case Eighty Four - Osteoid Osteoma retrieved from Musculoskeletal Imaging Teaching Files at http://www.uhrad.com/msiarc/msi084.htm
- ↑ P. osteoid osteoma. YouTube. https://www.youtube.com/watch?v=G4JJv1dhEa0. Published July 30, 2016. Accessed April 10, 2017.