Physical Activity, Sport and Recreation for Young People with Physical Disabilities: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) (Corrected reference errors) |
||
| (383 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
<div class=" | <div class="editorbox">'''Original Editor ''' - [[User:Dunika Dissanayake|Dunika Dissanayake]], [[User:Janan Kothari|Janan Kothari]], [[User:Orla Corrigan|Orla Corrigan]], [[User:Rhianne Joy Brisbane|Rhianne Brisbane]], [[User:Sinead Moloney|Sinead Moloney]] and [[User:Vanessa Puzzuoli|Vanessa Puzzuoli]] as part of the [[Current_and_Emerging_Roles_in_Physiotherapy_Practice|Queen Margaret University's Current and Emerging Roles in Physiotherapy Practice Project]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | |||
</div> | |||
Children should aim to take part in at least one hour of medium to hard intensity physical activity every day.<ref name="PAWHO">Physical Activity. World Health Organisation. Available from: http://www.who.int/mediacentre/factsheets/fs385/en/. [Accessed 16th November 2016].</ref> Encouraging children to be active with the distractions of technology can often be difficult but even more so if the child has a disability or medical condition. Guidance on how activities and exercises can be adapted can often be challenging that individuals living with disabilities were 82% more likely to take part in regular physical activity if a health professional advised it?<ref>Physical Activity and Health. Centres for Disease Control and Prevention. Available from: http://www.cdc.gov/physicalactivity/basics/pa-health/index.htm</ref> | |||
</ | |||
=== | <br>[[Image:Summarise.jpg]] | ||
=== Benefits of Physical Activity! === | |||
Physical activity is crucial for a child’s health an wellbeing, here are a few other benefits: | |||
*Can help a child feel more confident about themselves! | |||
*Can help to maintain a child's weight | |||
*Can improve motor skills, so they may find it a bit easier to perform certain movements they may have struggled with before<ref name="emck">Emck C, Bosscher R, Beek P, Doreleijers T. Gross motor performance and self‐perceived motor competence in children with emotional, behavioural, and pervasive developmental disorders: a review. Developmental Medicine & Child Neurology. 2009, Jul 1;51(7):501-17.</ref> | |||
*Can improve their participation in school and P.E. classes<ref name="emck" /> | |||
*Can improve their mood<ref name="emck" /> | |||
*Can help improve their breathing | |||
*Can improve their bone, muscle and heart health | |||
*Can reduce the risk of falls and fractures | |||
*Active wheelchair users are less likely to have pressure sores and kidney complications than those who don’t take part in much physical activity. | |||
*Physical activity can also help a child with problems related to their behaviour<ref>Moone MS, Renzaglia A. Physical fitness and the mentally retarded: a critical review of the literature Journal of Special Education. 1982;16(16) 3: 269 -287.</ref><ref>Nishiyama S, Kuwahara T, Maatsudea I. Decreased bone density in severely handicapped children and adults with reference to the influence of limited mobility and anticonvulsant medication European Journal of Pediatrics. 1986; 144(5): 457-763.</ref><ref>Lancioni GE. Procedures for promoting independent activity in people with severe and profound learning disability: A brief review: Mental Handicap Research. 1994; 7 (3):237-256</ref><ref>Lancioni GE, O'Reilly MF. A review of research on physical exercise with people with severe and profound developmental disabilities. Research in Development Disabilities. 1998; 19(6): 477-492.</ref><ref>Washburn RA, Zhu W, McAuley E, Frogle M, Figonis SF. The physical Activity Scale for individuals with physical disabilities: Development and Evaluation. Archives of Physical Medicine and Rehabilitation. 2002; 83:193-200.</ref><ref>Nary DE, Froehlich AK, White GW. Accessibility of fitness facilities for persons with physical disabilities using wheelchairs. Topics in Spinal Cord Injury Rehabilitation. 2000; 6(1): 90-101.</ref><ref>Boland M. Health promotion and health promotion needs assessment of people attending disability services in the HSE, East Coast Area. Doctorate of Medicine, University College Dublin. 2005</ref> | |||
*Physical activity plays an important part in maintaining good fitness and it lowers their chances of getting a lifelong illnesses and/or other health conditions.<ref>12. Fentem PH. Education and debate ABC of Sports Medicine: Benefits of exercise in health and disease. British Medical Journal. 1994;308:1291-1295.</ref> <br> | |||
== Physical Activity | === Benefits and Disadvantages o Physical Activity for Wheelchair Users === | ||
Manual wheelchair users often feel pain around their shoulders because shoulders are naturally made for moving around rather than for constantly lifting and pushing lots of weight!<ref name="fullerton">Fullerton HD, Borckardt JJ, Alfano AP. Shoulder pain: A comparison of wheelchair athletes and nonathletic wheelchair users. Med. Sci. Sports Exec. 2003. Vol 35, No 12, pp. 1958-1961.</ref> The day-to-day life of a person who uses a manual wheelchair often involves a lot of pushing and lifting; from pushing themselves around all day to lifting themselves into and out of their wheelchair. This means that any shoulder injury may limit the amount of things they can normally do for themselves.<ref name="fullerton" /><ref name="curtis">Curtis KA, Black K. Shoulder pain in female wheelchair basketball players. Journal of Orthopaedic & Sports Physical Therapy. 1999. Vol, 29N No 4, pp. 225–231.</ref> | |||
= | Many injuries can happen from carrying out a shoulder movement for a specific task that is difficult to complete. For example, lifting a very heavy object over the head or by repeatedly performing a normal movement so often that your joint begins to wear down.<ref name="fullerton" /> Activities like pushing a wheelchair for long distances or transferring in and out of a wheelchair many times throughout the day can cause an overuse injury.<ref name="fullerton" /><ref name="curtis" /> | ||
Getting exercise through sports is a great way to help strengthen your child’s muscles. Making sure their muscles and joints are strong means they will have the best chance at living independently, and goes a long way to improving their overall wellbeing!<ref name="fullerton" /><ref name="curtis" /> | |||
It is important to minimise the risk of injury. Some common problems that can occur and how to avoid them include: | |||
* Skin | |||
** Prevent blisters on hands with gloves | |||
** Prevent wheel-burns by covering the area with protective material | |||
** Decrease bruising by placing pads where needed, i.e. bony areas and retaining straps | |||
** Cover blisters | |||
* Swimming | |||
** Protect skin | |||
** Place mats at the poolside during transfers | |||
** Protect the feet | |||
* Muscles and Joints | |||
** Monitor for overuse | |||
** Closely observe any muscle or joint pain | |||
** Maintain flexibility with stretching | |||
* Hyperthermia (High body temperature) | |||
** Take into account temperature if exercising outdoors | |||
** Encourage to drink lots of water | |||
** Avoid direct sunlight | |||
* Pressure Sores | |||
** Use cushions and padding where needed | |||
** Change position and shift weight regularly<br> | |||
< | === Risks of Inactivity === | ||
Not taking part in enough physical activity is one of the biggest risk factors for death around the world. Individuals with disabilities have a 3 times higher chance of having health-related problems than individuals who do not have disabilities.<ref name="ref14">Increasing Physical Activity among Adults with Disabilities. Centres for Disease Control and Prevention. Available from: http://www.cdc.gov/ncbddd/disabilityandhealth/pa.html</ref> People who are less active have a 20-30% higher risk of death compared to people who are more active. Physical inactivity can also lead to fatigue and depression, putting on more weight, becoming more dependent on others. It also increases the risk of heart disease, type 2 diabetes, high blood pressure, stroke, pressure sores, weaker bones, depression and several cancers.<ref name="ref14" /> | |||
== Barriers and Facilitators to Exercise == | |||
A child’s disability may make taking part in physical activity more difficult as it may limit range of movement at joints, flexibility, agility, strength or endurance, and balance and coordination.<ref name="conchar">Conchar L, Bantjes J, Swartz L, Derman W. Barriers and facilitators to participation in physical activity: The experiences of a group of South African adolescents with cerebral palsy. Journal of health psychology. 2014 Mar 6:1359105314523305.</ref> Any of these limitations, may demotivate a child from taking part in more activities as well as: | |||
*Pain and/or fatigue may also limit a child from being active. It can often be due to overtraining, sitting for long periods or wearing their assistive devices such as an orthosis.<ref name="conchar" /> | |||
< | *A child may take more time to go outdoors during school breaks if they have to handle and wear orthoses. They may see it as an inconvenience and may stop using this time to play outside with their friends.<ref name="lauruschkus">Lauruschkus K, Nordmark E, Hallström I. “It’s fun, but…” Children with cerebral palsy and their experiences of participation in physical activities. Disability and rehabilitation. 2014 Feb 13;37(4):283-9</ref> | ||
*Physical strength and skills that a child develops may be lost due to interruptions in training or recovery after surgery.<ref name="conchar" /> | |||
<br> | *As a child gets older, the gap between able-bodied children and disabled athletes in terms of physical strength and agility grows larger. With this, the skills gap also widens and sports become more competitive. As a result, it may become more difficult for a child to continue taking part in mainstream activities.<ref name="conchar" /> <br> | ||
=== | === Psychosocial and Emotional Barriers === | ||
* | *Embarrassment, vulnerability, disappointment and shame at appearing physically incapable are just some of the uncomfortable emotions a child may experience. These feelings may lower their confidence and self-esteem. They may also feel frustrated at taking longer to learn a new skill and as a result, may avoid taking part in certain activities altogether.<ref name="conchar" /> | ||
< | *Negative attitudes from parents, staff and peers can hinder a child’s interest in physical activity.<ref name="jones">Jones DB. “Denied from a lot of places” barriers to participation in community recreation programs encountered by children with disabilities in Maine: perspectives of parents. Leisure/Loisir. 2003 Jan 1;28(1-2):49-69.</ref> It may come in the form of teasing from other children and/or teachers who lack training in adapting activities to suit your child needs. This also results in excluding them from taking part in school clubs and activities.<ref name="shields">Shields N, Synnot A. Perceived barriers and facilitators to participation in physical activity for children with disability: a qualitative study. BMC pediatrics. 2012 Jan 19;16(1):1.</ref> | ||
= | *As a result, a child may feel singled out and alone. These feelings can sometimes lead them to believe they are not good enough and can make it more difficult for them to persevere with physical activity.<ref name="lauruschkus" /> | ||
=== Cost and Environmental Barriers === | |||
& | *Finding time in the midst of appointments with various therapists, school runs, caring for other children, along with day-to-day duties poses as one of the main barriers to including physical activity in a child’s life. With the extra expenses of caring for a child with a disability and fewer earnings due to taking on caring responsibilities instead of work, there is often little money leftover to spend on membership for various classes and clubs.<ref name="shields" /> | ||
< | *Sporting opportunities specific to a child’s abilities, as well as those available locally are often poorly advertised.<ref name="jaarsma">Jaarsma EA, Dijkstra PU, de Blécourt AC, Geertzen JH, Dekker R. Barriers and facilitators of sports in children with physical disabilities: a mixed-method study. Disability and rehabilitation. 2015 Aug 28;37(18):1617-25.</ref><ref name="shields" /> | ||
* | *Sporting facilities that cater for a child’s needs may be often lacking in certain areas such as shortage of qualified staff willing to supervise activities for children with motor impairments and lack of equipment to aid sports, especially as a child gets older.<ref name="shields2">Shields N, Synnot A. Perceived barriers and facilitators to participation in physical activity for children with disability: a qualitative study. BMC pediatrics. 2016 Jan 19;16(1):1.</ref><ref name="lauruschkus" /> | ||
< | *Unfortunately, local clubs and societies may also face difficulties such recruiting enough children to make up teams or finding other teams to play against.<ref name="conchar" /> | ||
= | *With this comes the barrier of transport. Living far away from such facilities and having to travel to introduce a child to such activities, may not be always be easy to access via public transport.<ref name="conchar" /> | ||
*One off programmes as well as long waiting lists for specialised classes may also pose as a barrier to a child’s participation in physical activity.<ref name="shields" /> | |||
< | *Specialised adaptive equipment for sports is also costly and not always readily available.<ref name="rimmer">Rimmer JH, Riley B, Wang E, Rauworth A, Jurkowski J. Physical activity participation among persons with disabilities: barriers and facilitators. American journal of preventive medicine. 2004 Jun 30;26(5):419-25.</ref> | ||
*Environmental barriers may also get in the way to accessing sporting facilities. These may include lack of curb cuts and ramps, doors being too narrow for wheelchair access and reception desks being too high to talk to staff. <br> | |||
=== Social Facilitators === | |||
< | *Studies have shown that children (aged 4-7) of physically active mothers are twice as likely to take part in physical activity than children with inactive mothers. The are also 3.5 times more likely to engage in physical activity if they have active fathers. Those with two active parents are almost 6 times more likely to be physically active than children of inactive parents.<ref name="moore">Moore LL, Lombardi DA, White MJ, Campbell JL, Oliveria SA, Ellison RC. Influence of parents' physical activity levels on activity levels of young children. The Journal of pediatrics. 1991 Feb 28;118(2):215-9.</ref> | ||
* | *Encouraging parents to take an active interest in their child’s daily schedule. Suggest reducing screen time during the day and encouraging children to go outside and play. Factor in the time taken to go to the park or a class to include physical as a daily requirement. | ||
*Habits of friends and siblings can also impact a child’s decision to take part in activities. Children enjoy belonging to something or someone; taking part in activities with family and friends can give them a feeling of togetherness and of being noticed and accepted as part of a group. It also gives them the opportunity to meet others with similar abilities and most importantly to be seen as more than their disability! | |||
[[Image:6Fs.jpg|center]] | |||
== | == Conclusion == | ||
Physical activity is hugely important for everyone, and children with physical disabilities are no exception. Unfortunately, children with disabilities are less active than their able-bodied peers and therefore encouraging their participation in sporting and recreational activities is vital.<ref name="shields2" /> In this online resource we have talked you through the various physical and psychological advantages of being physically active such as, but not limited to improvements in body function, heart and bone health, psychological wellbeing and social engagement.<ref name="shields2" /> | |||
== References == | == References == | ||
<references /> | |||
[[Category:Sports Medicine]] | |||
[[Category:Younger Athlete]] | |||
[[Category:Occupational Health]] | |||
[[Category:Queen Margaret University Project]] | |||
[[Category:Current and Emerging Roles in Physiotherapy Practice]] | |||
Latest revision as of 13:07, 22 May 2020
Introduction[edit | edit source]
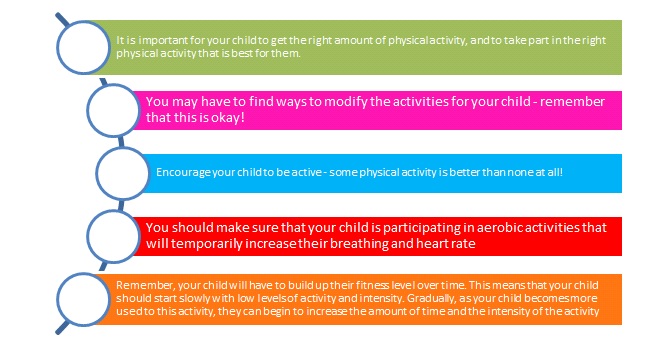
Children should aim to take part in at least one hour of medium to hard intensity physical activity every day.[1] Encouraging children to be active with the distractions of technology can often be difficult but even more so if the child has a disability or medical condition. Guidance on how activities and exercises can be adapted can often be challenging that individuals living with disabilities were 82% more likely to take part in regular physical activity if a health professional advised it?[2]
Benefits of Physical Activity![edit | edit source]
Physical activity is crucial for a child’s health an wellbeing, here are a few other benefits:
- Can help a child feel more confident about themselves!
- Can help to maintain a child's weight
- Can improve motor skills, so they may find it a bit easier to perform certain movements they may have struggled with before[3]
- Can improve their participation in school and P.E. classes[3]
- Can improve their mood[3]
- Can help improve their breathing
- Can improve their bone, muscle and heart health
- Can reduce the risk of falls and fractures
- Active wheelchair users are less likely to have pressure sores and kidney complications than those who don’t take part in much physical activity.
- Physical activity can also help a child with problems related to their behaviour[4][5][6][7][8][9][10]
- Physical activity plays an important part in maintaining good fitness and it lowers their chances of getting a lifelong illnesses and/or other health conditions.[11]
Benefits and Disadvantages o Physical Activity for Wheelchair Users[edit | edit source]
Manual wheelchair users often feel pain around their shoulders because shoulders are naturally made for moving around rather than for constantly lifting and pushing lots of weight![12] The day-to-day life of a person who uses a manual wheelchair often involves a lot of pushing and lifting; from pushing themselves around all day to lifting themselves into and out of their wheelchair. This means that any shoulder injury may limit the amount of things they can normally do for themselves.[12][13]
Many injuries can happen from carrying out a shoulder movement for a specific task that is difficult to complete. For example, lifting a very heavy object over the head or by repeatedly performing a normal movement so often that your joint begins to wear down.[12] Activities like pushing a wheelchair for long distances or transferring in and out of a wheelchair many times throughout the day can cause an overuse injury.[12][13]
Getting exercise through sports is a great way to help strengthen your child’s muscles. Making sure their muscles and joints are strong means they will have the best chance at living independently, and goes a long way to improving their overall wellbeing![12][13]
It is important to minimise the risk of injury. Some common problems that can occur and how to avoid them include:
- Skin
- Prevent blisters on hands with gloves
- Prevent wheel-burns by covering the area with protective material
- Decrease bruising by placing pads where needed, i.e. bony areas and retaining straps
- Cover blisters
- Swimming
- Protect skin
- Place mats at the poolside during transfers
- Protect the feet
- Muscles and Joints
- Monitor for overuse
- Closely observe any muscle or joint pain
- Maintain flexibility with stretching
- Hyperthermia (High body temperature)
- Take into account temperature if exercising outdoors
- Encourage to drink lots of water
- Avoid direct sunlight
- Pressure Sores
- Use cushions and padding where needed
- Change position and shift weight regularly
Risks of Inactivity[edit | edit source]
Not taking part in enough physical activity is one of the biggest risk factors for death around the world. Individuals with disabilities have a 3 times higher chance of having health-related problems than individuals who do not have disabilities.[14] People who are less active have a 20-30% higher risk of death compared to people who are more active. Physical inactivity can also lead to fatigue and depression, putting on more weight, becoming more dependent on others. It also increases the risk of heart disease, type 2 diabetes, high blood pressure, stroke, pressure sores, weaker bones, depression and several cancers.[14]
Barriers and Facilitators to Exercise[edit | edit source]
A child’s disability may make taking part in physical activity more difficult as it may limit range of movement at joints, flexibility, agility, strength or endurance, and balance and coordination.[15] Any of these limitations, may demotivate a child from taking part in more activities as well as:
- Pain and/or fatigue may also limit a child from being active. It can often be due to overtraining, sitting for long periods or wearing their assistive devices such as an orthosis.[15]
- A child may take more time to go outdoors during school breaks if they have to handle and wear orthoses. They may see it as an inconvenience and may stop using this time to play outside with their friends.[16]
- Physical strength and skills that a child develops may be lost due to interruptions in training or recovery after surgery.[15]
- As a child gets older, the gap between able-bodied children and disabled athletes in terms of physical strength and agility grows larger. With this, the skills gap also widens and sports become more competitive. As a result, it may become more difficult for a child to continue taking part in mainstream activities.[15]
Psychosocial and Emotional Barriers[edit | edit source]
- Embarrassment, vulnerability, disappointment and shame at appearing physically incapable are just some of the uncomfortable emotions a child may experience. These feelings may lower their confidence and self-esteem. They may also feel frustrated at taking longer to learn a new skill and as a result, may avoid taking part in certain activities altogether.[15]
- Negative attitudes from parents, staff and peers can hinder a child’s interest in physical activity.[17] It may come in the form of teasing from other children and/or teachers who lack training in adapting activities to suit your child needs. This also results in excluding them from taking part in school clubs and activities.[18]
- As a result, a child may feel singled out and alone. These feelings can sometimes lead them to believe they are not good enough and can make it more difficult for them to persevere with physical activity.[16]
Cost and Environmental Barriers[edit | edit source]
- Finding time in the midst of appointments with various therapists, school runs, caring for other children, along with day-to-day duties poses as one of the main barriers to including physical activity in a child’s life. With the extra expenses of caring for a child with a disability and fewer earnings due to taking on caring responsibilities instead of work, there is often little money leftover to spend on membership for various classes and clubs.[18]
- Sporting opportunities specific to a child’s abilities, as well as those available locally are often poorly advertised.[19][18]
- Sporting facilities that cater for a child’s needs may be often lacking in certain areas such as shortage of qualified staff willing to supervise activities for children with motor impairments and lack of equipment to aid sports, especially as a child gets older.[20][16]
- Unfortunately, local clubs and societies may also face difficulties such recruiting enough children to make up teams or finding other teams to play against.[15]
- With this comes the barrier of transport. Living far away from such facilities and having to travel to introduce a child to such activities, may not be always be easy to access via public transport.[15]
- One off programmes as well as long waiting lists for specialised classes may also pose as a barrier to a child’s participation in physical activity.[18]
- Specialised adaptive equipment for sports is also costly and not always readily available.[21]
- Environmental barriers may also get in the way to accessing sporting facilities. These may include lack of curb cuts and ramps, doors being too narrow for wheelchair access and reception desks being too high to talk to staff.
Social Facilitators[edit | edit source]
- Studies have shown that children (aged 4-7) of physically active mothers are twice as likely to take part in physical activity than children with inactive mothers. The are also 3.5 times more likely to engage in physical activity if they have active fathers. Those with two active parents are almost 6 times more likely to be physically active than children of inactive parents.[22]
- Encouraging parents to take an active interest in their child’s daily schedule. Suggest reducing screen time during the day and encouraging children to go outside and play. Factor in the time taken to go to the park or a class to include physical as a daily requirement.
- Habits of friends and siblings can also impact a child’s decision to take part in activities. Children enjoy belonging to something or someone; taking part in activities with family and friends can give them a feeling of togetherness and of being noticed and accepted as part of a group. It also gives them the opportunity to meet others with similar abilities and most importantly to be seen as more than their disability!
Conclusion[edit | edit source]
Physical activity is hugely important for everyone, and children with physical disabilities are no exception. Unfortunately, children with disabilities are less active than their able-bodied peers and therefore encouraging their participation in sporting and recreational activities is vital.[20] In this online resource we have talked you through the various physical and psychological advantages of being physically active such as, but not limited to improvements in body function, heart and bone health, psychological wellbeing and social engagement.[20]
References[edit | edit source]
- ↑ Physical Activity. World Health Organisation. Available from: http://www.who.int/mediacentre/factsheets/fs385/en/. [Accessed 16th November 2016].
- ↑ Physical Activity and Health. Centres for Disease Control and Prevention. Available from: http://www.cdc.gov/physicalactivity/basics/pa-health/index.htm
- ↑ 3.0 3.1 3.2 Emck C, Bosscher R, Beek P, Doreleijers T. Gross motor performance and self‐perceived motor competence in children with emotional, behavioural, and pervasive developmental disorders: a review. Developmental Medicine & Child Neurology. 2009, Jul 1;51(7):501-17.
- ↑ Moone MS, Renzaglia A. Physical fitness and the mentally retarded: a critical review of the literature Journal of Special Education. 1982;16(16) 3: 269 -287.
- ↑ Nishiyama S, Kuwahara T, Maatsudea I. Decreased bone density in severely handicapped children and adults with reference to the influence of limited mobility and anticonvulsant medication European Journal of Pediatrics. 1986; 144(5): 457-763.
- ↑ Lancioni GE. Procedures for promoting independent activity in people with severe and profound learning disability: A brief review: Mental Handicap Research. 1994; 7 (3):237-256
- ↑ Lancioni GE, O'Reilly MF. A review of research on physical exercise with people with severe and profound developmental disabilities. Research in Development Disabilities. 1998; 19(6): 477-492.
- ↑ Washburn RA, Zhu W, McAuley E, Frogle M, Figonis SF. The physical Activity Scale for individuals with physical disabilities: Development and Evaluation. Archives of Physical Medicine and Rehabilitation. 2002; 83:193-200.
- ↑ Nary DE, Froehlich AK, White GW. Accessibility of fitness facilities for persons with physical disabilities using wheelchairs. Topics in Spinal Cord Injury Rehabilitation. 2000; 6(1): 90-101.
- ↑ Boland M. Health promotion and health promotion needs assessment of people attending disability services in the HSE, East Coast Area. Doctorate of Medicine, University College Dublin. 2005
- ↑ 12. Fentem PH. Education and debate ABC of Sports Medicine: Benefits of exercise in health and disease. British Medical Journal. 1994;308:1291-1295.
- ↑ 12.0 12.1 12.2 12.3 12.4 Fullerton HD, Borckardt JJ, Alfano AP. Shoulder pain: A comparison of wheelchair athletes and nonathletic wheelchair users. Med. Sci. Sports Exec. 2003. Vol 35, No 12, pp. 1958-1961.
- ↑ 13.0 13.1 13.2 Curtis KA, Black K. Shoulder pain in female wheelchair basketball players. Journal of Orthopaedic & Sports Physical Therapy. 1999. Vol, 29N No 4, pp. 225–231.
- ↑ 14.0 14.1 Increasing Physical Activity among Adults with Disabilities. Centres for Disease Control and Prevention. Available from: http://www.cdc.gov/ncbddd/disabilityandhealth/pa.html
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 Conchar L, Bantjes J, Swartz L, Derman W. Barriers and facilitators to participation in physical activity: The experiences of a group of South African adolescents with cerebral palsy. Journal of health psychology. 2014 Mar 6:1359105314523305.
- ↑ 16.0 16.1 16.2 Lauruschkus K, Nordmark E, Hallström I. “It’s fun, but…” Children with cerebral palsy and their experiences of participation in physical activities. Disability and rehabilitation. 2014 Feb 13;37(4):283-9
- ↑ Jones DB. “Denied from a lot of places” barriers to participation in community recreation programs encountered by children with disabilities in Maine: perspectives of parents. Leisure/Loisir. 2003 Jan 1;28(1-2):49-69.
- ↑ 18.0 18.1 18.2 18.3 Shields N, Synnot A. Perceived barriers and facilitators to participation in physical activity for children with disability: a qualitative study. BMC pediatrics. 2012 Jan 19;16(1):1.
- ↑ Jaarsma EA, Dijkstra PU, de Blécourt AC, Geertzen JH, Dekker R. Barriers and facilitators of sports in children with physical disabilities: a mixed-method study. Disability and rehabilitation. 2015 Aug 28;37(18):1617-25.
- ↑ 20.0 20.1 20.2 Shields N, Synnot A. Perceived barriers and facilitators to participation in physical activity for children with disability: a qualitative study. BMC pediatrics. 2016 Jan 19;16(1):1.
- ↑ Rimmer JH, Riley B, Wang E, Rauworth A, Jurkowski J. Physical activity participation among persons with disabilities: barriers and facilitators. American journal of preventive medicine. 2004 Jun 30;26(5):419-25.
- ↑ Moore LL, Lombardi DA, White MJ, Campbell JL, Oliveria SA, Ellison RC. Influence of parents' physical activity levels on activity levels of young children. The Journal of pediatrics. 1991 Feb 28;118(2):215-9.